Non-pharmacological therapies for normal ageing and dementia are a set of treatment programmes intended to improve the performance of cognitive processes, improve emotional well-being, promote independence in daily life activities, and ultimately increase patients’ quality of life.
MethodsWe applied a battery of tests assessing four major domains (general mental state, emotional well-being, quality of life, and daily life activities) to a sample of 317 adults older than 64 (240 with normal ageing and 77 with cognitive impairment). They were then assigned to non-pharmacological therapy groups according to their abilities or other non-specific activities. Progress was assessed 9 months later using the same test battery.
ResultsThe results show a general improvement in mental state in the group with normal ageing and absence of disease progression in the group with pathological ageing. In both groups, emotional well-being (anxiety and depression) and self-identified quality of life both benefited from non-pharmacological therapy. However, other aspects commonly included among the therapeutic targets did not seem to improve, including independence in daily life activities.
ConclusionsThis study provides evidence that non-pharmacological therapy in ageing patients can produce positive results. It must be stressed that benefits are greater in individuals with cognitive impairment, although generalising use of this therapy could prove to be an excellent primary programme for preventing cognitive and emotional disorders.
Las terapias no farmacológicas (TNF) en el envejecimiento y las demencias representan un conjunto de intervenciones orientadas a estimular el rendimiento de los procesos cognitivos, mejorar la afectividad, potenciar la independencia en la vida cotidiana y, en última instancia, incrementar la calidad de vida de los pacientes.
MétodosSe aplicó una batería de pruebas que valoraban 4 dominios principales (estado mental general, afectividad, calidad de vida y actividades de la vida diaria) a una muestra de 317 adultos con más de 64 años (240 con envejecimiento normal y 77 con deterioro cognitivo). Posteriormente, fueron asignados a grupos de TNF en función de sus capacidades o a otras actividades no específicas. Se valoró el beneficio tras 9 meses de TNF con la misma batería de pruebas.
ResultadosLos resultados evidencian una mejora del estado mental general en el envejecimiento sano y ausencia de progresión en el envejecimiento patológico. En los 2 grupos, la afectividad (ansiedad y depresión) y la calidad de vida autopercibida se vio beneficiada por la TNF. No obstante, no parecen mejorar otros aspectos habitualmente incluidos entre los objetivos terapéuticos, como la independencia en las actividades de la vida diaria.
ConclusionesEste trabajo evidencia los resultados positivos que se obtienen por la aplicación de un programa de TNF en el envejecimiento. Es importante destacar que los individuos con deterioro cognitivo se benefician más del mismo, si bien su aplicación generalizada parece resultar un óptimo programa preventivo primario en estos aspectos cognitivos y emocionales.
In recent years, doctors have begun to consider the effectiveness of using non-pharmacological therapies (NPT) for ageing and dementia in order to boost performance of cognitive tasks, improve emotional well-being, increase independence in daily life, and generally improve quality of life for the elderly.1–4 NPTs are defined as non-chemical interventions that are theory-based, focused, and repeatable. They are performed on either the patient or the carer, and may be able to deliver substantial benefits.5 As stated by Peña-Casanova,6 the specific treatment objectives of this type of intervention are as follows: (a) stimulate and maintain mental capacity; (b) foster interaction with surroundings and strengthen social relationships; (c) provide a sense of security and increase patient independence; (d) stimulate the patient's identity and self-worth; (e) minimise stress and prevent abnormal psychological reactions; (f) improve cognitive performance; (g) improve functional performance; (h) increase personal independence in activities of daily living; (i) improve the state and perception of health; and (j) improve quality of life for the patient and family members/carers.
Some of the most commonly used patient-oriented NPTs include cognitive stimulation, behavioural intervention, physical exercise, music therapy, training in activities of daily life, reminiscence therapy, and muscle relaxation.7,8 Of all of these activities, cognitive stimulation is the therapy with the most empirical support,9 and has even been proposed as the first NPT to be carried out in cases of dementia.10 Some of the most widely-used standard cognitive stimulation programmes in Spain include Programa de Psicoestimulación Integral,11Programa Activemos la Mente,12el Baúl de los Recuerdos used by Spain's national Alzheimer association,13 and Programa de Memoria used by the municipal government of Madrid.14
The use of models with different exercises for cognitive stimulation in elderly patients has increased in the last few years. This has provided a certain amount of accumulated evidence regarding the utility of such exercises in normal ageing,15–19 mild cognitive impairment,20 and Alzheimer disease in conjunction with procholinergic drug therapy.21,22 Doctors generally agree that this type of NPT, which permits and even promotes group therapy, is no substitute for an individually-designed neuropsychological intervention programme. One reason is that the number of patients requesting NPT through the public healthcare system makes it difficult to provide this type of specific intervention. With the above in mind, we need additional studies analysing real benefits obtained from group interventions and generic exercises. It would also be interesting to determine if results from generic exercises affect all the areas listed above as treatment objectives. This study therefore aims to evaluate the effects of group NPT by examining results in 4 main areas: general mental state, emotional response, other psychological variables including subjective well-being or satisfaction with life, and independence in activities of daily living.
MethodParticipantsThe sample consisted of a total of 317 adult subjects aged 65 and older who applied to participate in social and cultural activities offered by free, public institutions (municipal senior centres in Madrid's central district). Subjects included 273 women (86.1%) and 44 men (13.9%) with a mean age of 77 years and 5 months (typical deviation, 6 years and 3 months). All subjects had either normal vision and hearing or devices to correct vision and hearing. None of the participants had motor impairments that would prevent them from performing the exercises. Performance was also largely contingent on the patient having been educated well enough to read and write in Spanish. All subjects were informed of the evaluation's dual focus (as a clinical and research study) and consented to their data being used anonymously.
InstrumentsA structured interview was used to obtain participants’ sociodemographic information, including sex, age, educational level (functionally illiterate, primary studies, secondary studies, university); occupation (home-maker, unskilled worker, semi-skilled worker, skilled worker); marital status (single, married, divorced/separated, widowed); number of children or living arrangement (alone, with a partner, with children, with other family members, or with a paid carer).
Subjects’ general cognitive state was evaluated using the Miniexamen Cognoscitivo (MEC)23 and the adapted and validated Spanish-language version24 of the Short Portable Mental Status Questionnaire (SPMSQ) by Pfeiffer.25 Emotional state and levels of anxiety and depression in particular were assessed using the adapted version27 of the State-Trait Anxiety Inventory (STAI)26 and the Geriatric Depression Scale (GDS).28 Lastly, to analyse other psychological and social adjustment variables, we used the following:
- –
Rosenberg's Self-Esteem Scale, (RSES)29,30 consisting of 10 questions regarding self-perceived levels of self-esteem that are answered using a 4-point Likert scale (1: strongly agree, 2: agree, 3: disagree, and 4: strongly disagree). Scores range from 10 to 40, with scores higher than 25 suggesting low self-esteem.
- –
The Satisfaction with Life Scale (SWLS),31,32 consisting of 5 questions whose answers correspond to a 5-point Likert scale (1: strongly disagree, 2: disagree, 3: neither agree nor disagree, 4: agree, and 5: strongly agree). Higher scores are indicative of a greater degree of satisfaction with life.
- –
The Life Orientation Test (LOT-R)33,34 contains 10 questions answered with a 5-point Likert scale similar to the one described above. Scores range from 0 to 40, with a score of 40 indicating a very high level of optimism.
- –
The OARS Social Resource Scale35,36 consists of 10 questions with either yes/no answers or Likert scale answers. The score resulting from the answers selected is given as follows: 1: excellent social resources, 2: good social resources, 3: mildly socially impaired, 4: moderately socially impaired, 5: severely socially impaired, and 6: totally socially impaired.
We used the Katz Index of Independence in Activities of Daily Living37 (Spanish-language version38,39) and the Lawton and Brody Instrumental Activities of Daily Living Scale (IADL)40 to determine the degree of functional dependence or independence.
ProcedureThose patients who lacked a previous neurological or psychiatric diagnosis and showed no symptoms of cognitive decline in the examination completed prior to therapy were invited to participate in cognitive stimulation treatment groups intended to prevent impairment in individuals with normal ageing. Patients who had previously been diagnosed with mild cognitive impairment or early-stage Alzheimer disease were assigned to cognitive stimulation groups according to the abilities they displayed in the evaluation.
This is therefore an observational study with consecutive recruitment of all individuals participating in cognitive stimulation groups and whose clinical assessment revealed normal ageing (NA-NPT), whether or not they voiced subjective concerns about memory, and of all individuals undergoing cognitive stimulation and diagnosed with cognitive impairment, whether mild cognitive impairment or early-stage Alzheimer disease (CI-NPT). Meanwhile, consecutive recruitment was also used for individuals of any diagnostic status who did not participate in cognitive stimulation groups due to schedule incompatibilities with domestic or family tasks (caring for grandchildren, etc.). This provided a control group with normal ageing (NA-noNPT) and another with cognitive impairment (CI-noNPT). The latter 2 groups were involved in different, non-specific leisure activities at other times. At the end of the study, they were included in the cognitive stimulation groups corresponding to their levels of ability if they were both interested in and available for those activities.
NPT groups were made up of a maximum of 20 subjects and monitored for 9 months (October to June). Therapy was scheduled for 1 hour a day, 2 days a week. The methodology for the group work sessions included the following:
Cognitive stimulation exercises created or modified on an ad hoc basis by staff at the senior centre according to each group's abilities. Exercises covered a wide range of cognitive processes: attention, perception, memory, language, inhibition, planning, reasoning, arithmetic, drawing, etc.41–54
Group dynamics tasks designed to strengthen social skills, the expression of positive feelings, and interaction between participants. Different sessions focused on awareness of general topics such as depression, anxiety, memory, self-esteem, and the concept of happiness.
Art therapy, conducted in partnership with the Thyssen museum, and team-building workshops were also used by the group to increase social participation and prevent isolation.
Following 9 months with either NPT (experimental group) or leisure activities (control group), we repeated the same test battery used before beginning the NPT programme. All intersubject measurements were taken a minimum of 10 months and a maximum of 12 months apart.
Statistical analysisFive age groups were established at this point in order to analyse the effect of age on testing performance. Groups were constituted as follows: age range 65 to 69 (n=74; 23.3%); 70 to 74 (n=81; 25.6%); 75 to 79 (n=90; 28.4%); 80 to 84 (n=48; 15.1%); and older than 84 (n=24; 7.6%).
The homogeneity of all the recorded sociodemographic variables was checked between the 2 groups (NA and CI) using the Mann–Whitney U test. Homogeneity between pre-treatment values was tested using ANOVA. A t-test (difference of means) was later performed for each group to let us know the effect of the passing of time, whether with or without NPT. Lastly, we ran a general linear analysis of the differences between the mean scores recorded prior to and following the intervention. This let us check for variables that might influence performance, such as sex, age group, and educational level. To estimate the magnitude of the effect of such differences in multivariate comparisons of the corrected model, we used the partial eta-squared value (η2p).
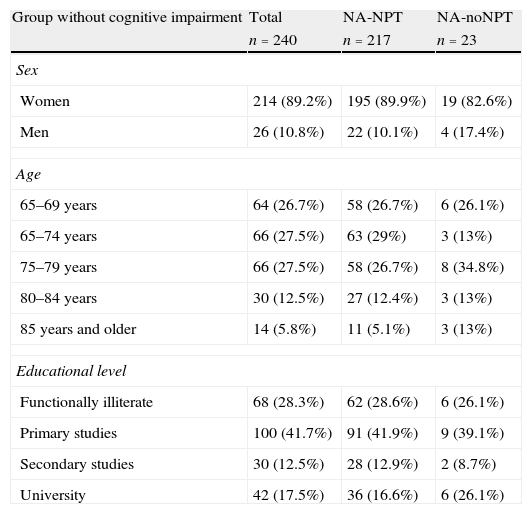
ResultsThe definitive sample that made up the normal ageing group (NA) was composed of 240 participants; 217 received NPT (NA-NPT) and 23 attended other leisure, social, or cultural activities (NA-noNPT). The analysis showed no significant differences in composition of the 2 groups with regard to either sociodemographic variables (P>.05 in all cases) or pre-treatment values (P>.05 in all cases). Table 1 shows the most important sociodemographic characteristics broken down by the groups that were created.
Principal sociodemographic variables for the group without cognitive impairment.
| Group without cognitive impairment | Total | NA-NPT | NA-noNPT |
| n=240 | n=217 | n=23 | |
| Sex | |||
| Women | 214 (89.2%) | 195 (89.9%) | 19 (82.6%) |
| Men | 26 (10.8%) | 22 (10.1%) | 4 (17.4%) |
| Age | |||
| 65–69 years | 64 (26.7%) | 58 (26.7%) | 6 (26.1%) |
| 65–74 years | 66 (27.5%) | 63 (29%) | 3 (13%) |
| 75–79 years | 66 (27.5%) | 58 (26.7%) | 8 (34.8%) |
| 80–84 years | 30 (12.5%) | 27 (12.4%) | 3 (13%) |
| 85 years and older | 14 (5.8%) | 11 (5.1%) | 3 (13%) |
| Educational level | |||
| Functionally illiterate | 68 (28.3%) | 62 (28.6%) | 6 (26.1%) |
| Primary studies | 100 (41.7%) | 91 (41.9%) | 9 (39.1%) |
| Secondary studies | 30 (12.5%) | 28 (12.9%) | 2 (8.7%) |
| University | 42 (17.5%) | 36 (16.6%) | 6 (26.1%) |
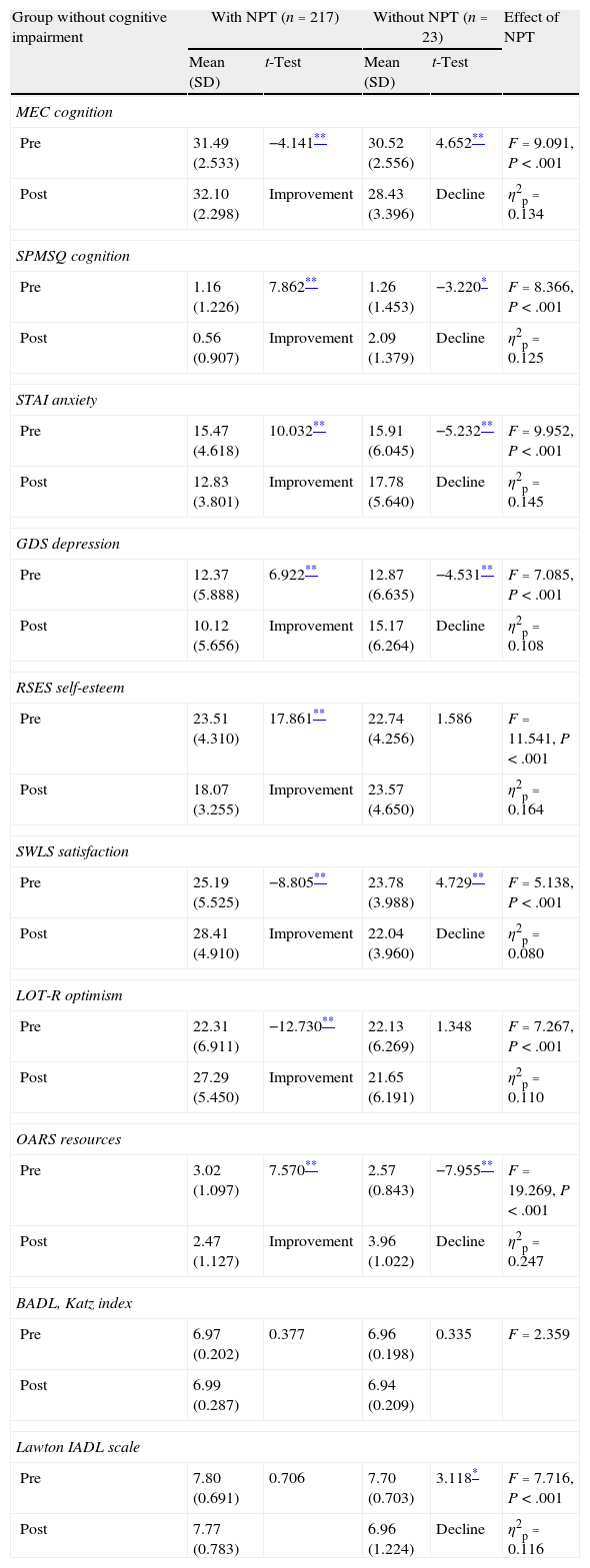
Table 2 shows how the NA-NPT group improved significantly on all the tests except those measuring both basic and instrumental activities of daily living (BADL, IADL). On the other hand, the NA-noNPT group performed more poorly on all tests except those measuring self-esteem, optimism, and BADL. It is interesting to note that this group, which had no therapeutic interventions, also showed a poorer performance on the IADL task after the study period, although this difference does not seem to be clinically significant.
Normal ageing group: difference of means (t-test) between pre-treatment and post-treatment scores and ANOVA of the effect of treatment controlled for age, sex, and years of education.
| Group without cognitive impairment | With NPT (n=217) | Without NPT (n=23) | Effect of NPT | ||
| Mean (SD) | t-Test | Mean (SD) | t-Test | ||
| MEC cognition | |||||
| Pre | 31.49 (2.533) | −4.141** | 30.52 (2.556) | 4.652** | F=9.091, P<.001 |
| Post | 32.10 (2.298) | Improvement | 28.43 (3.396) | Decline | η2p=0.134 |
| SPMSQ cognition | |||||
| Pre | 1.16 (1.226) | 7.862** | 1.26 (1.453) | −3.220* | F=8.366, P<.001 |
| Post | 0.56 (0.907) | Improvement | 2.09 (1.379) | Decline | η2p=0.125 |
| STAI anxiety | |||||
| Pre | 15.47 (4.618) | 10.032** | 15.91 (6.045) | −5.232** | F=9.952, P<.001 |
| Post | 12.83 (3.801) | Improvement | 17.78 (5.640) | Decline | η2p=0.145 |
| GDS depression | |||||
| Pre | 12.37 (5.888) | 6.922** | 12.87 (6.635) | −4.531** | F=7.085, P<.001 |
| Post | 10.12 (5.656) | Improvement | 15.17 (6.264) | Decline | η2p=0.108 |
| RSES self-esteem | |||||
| Pre | 23.51 (4.310) | 17.861** | 22.74 (4.256) | 1.586 | F=11.541, P<.001 |
| Post | 18.07 (3.255) | Improvement | 23.57 (4.650) | η2p=0.164 | |
| SWLS satisfaction | |||||
| Pre | 25.19 (5.525) | −8.805** | 23.78 (3.988) | 4.729** | F=5.138, P<.001 |
| Post | 28.41 (4.910) | Improvement | 22.04 (3.960) | Decline | η2p=0.080 |
| LOT-R optimism | |||||
| Pre | 22.31 (6.911) | −12.730** | 22.13 (6.269) | 1.348 | F=7.267, P<.001 |
| Post | 27.29 (5.450) | Improvement | 21.65 (6.191) | η2p=0.110 | |
| OARS resources | |||||
| Pre | 3.02 (1.097) | 7.570** | 2.57 (0.843) | −7.955** | F=19.269, P<.001 |
| Post | 2.47 (1.127) | Improvement | 3.96 (1.022) | Decline | η2p=0.247 |
| BADL, Katz index | |||||
| Pre | 6.97 (0.202) | 0.377 | 6.96 (0.198) | 0.335 | F=2.359 |
| Post | 6.99 (0.287) | 6.94 (0.209) | |||
| Lawton IADL scale | |||||
| Pre | 7.80 (0.691) | 0.706 | 7.70 (0.703) | 3.118* | F=7.716, P<.001 |
| Post | 7.77 (0.783) | 6.96 (1.224) | Decline | η2p=0.116 | |
NPT was observed to have a significant effect on the NA group for all measurements except for BADL after adjusting for sociodemographic variables (Table 2). We observed no effects on the benefits of therapy for the following variables: sex (F=0.420, P=.936), educational level (F=0.769, P=.658), occupation (F=1.532, P=.129), marital status (F=1.022, P=.426), number of children (F=0.296, P=.982), or living arrangement (F=0.846, P=.585). However, we do observe a significant age effect (F=2.583, P<.05) in that younger subjects seem to benefit the most from NPT.
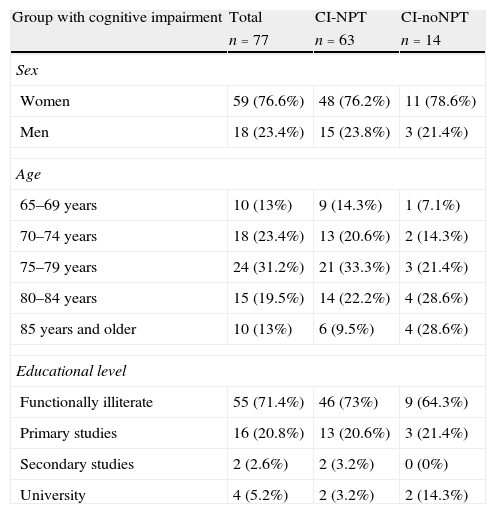
The subgroup that had been diagnosed with cognitive impairment (CI) contained 77 participants, of whom 63 underwent NPT (the CI-NPT group) and 14 participated in other leisure, social, or cultural activities (CI-noNPT). Analysis of the 2 groups showed no significant differences with regard to sociodemographic variables (P>.05 in all cases) or pre-treatment measurements (P>.05 in all cases, except for STAI, (F=9.214, P<.05, which revealed slightly higher levels of anxiety in the NPT group). Table 3 summarises the most important sociodemographic variables for each subgroup that was created.
Principal sociodemographic variables for the group with cognitive impairment.
| Group with cognitive impairment | Total | CI-NPT | CI-noNPT |
| n=77 | n=63 | n=14 | |
| Sex | |||
| Women | 59 (76.6%) | 48 (76.2%) | 11 (78.6%) |
| Men | 18 (23.4%) | 15 (23.8%) | 3 (21.4%) |
| Age | |||
| 65–69 years | 10 (13%) | 9 (14.3%) | 1 (7.1%) |
| 70–74 years | 18 (23.4%) | 13 (20.6%) | 2 (14.3%) |
| 75–79 years | 24 (31.2%) | 21 (33.3%) | 3 (21.4%) |
| 80–84 years | 15 (19.5%) | 14 (22.2%) | 4 (28.6%) |
| 85 years and older | 10 (13%) | 6 (9.5%) | 4 (28.6%) |
| Educational level | |||
| Functionally illiterate | 55 (71.4%) | 46 (73%) | 9 (64.3%) |
| Primary studies | 16 (20.8%) | 13 (20.6%) | 3 (21.4%) |
| Secondary studies | 2 (2.6%) | 2 (3.2%) | 0 (0%) |
| University | 4 (5.2%) | 2 (3.2%) | 2 (14.3%) |
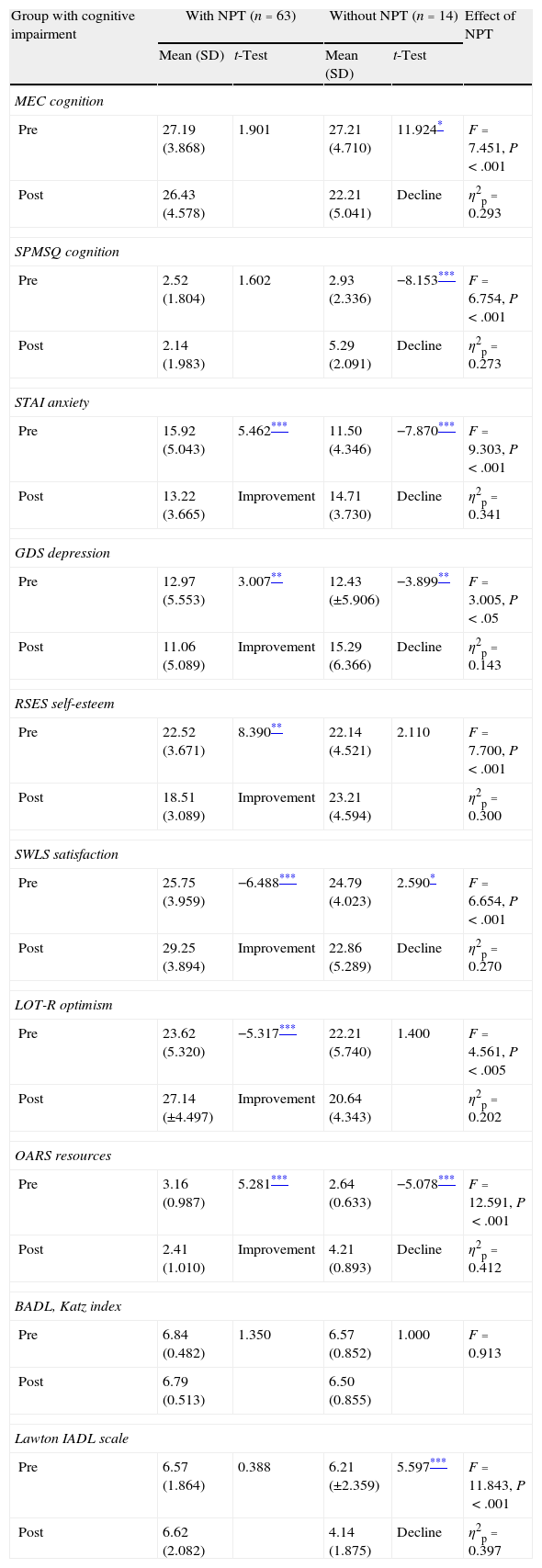
Table 4 displays how the scores for overall mental state, BADL, and IADL remained relatively stable in the CI-NPT group. Generally speaking, we observe significant improvements in all measurements of all other psychological variables. On the other hand, the CI-noNPT group displayed poorer scores for all measurements except those for self-esteem, optimism, and BADL. This also occurred in the group without cognitive impairment (NA).
Cognitive decline group: difference of means (t-test) between pre-treatment and post-treatment scores and ANOVA of the effect of treatment with adjustments for age, sex, and years of education.
| Group with cognitive impairment | With NPT (n=63) | Without NPT (n=14) | Effect of NPT | ||
| Mean (SD) | t-Test | Mean (SD) | t-Test | ||
| MEC cognition | |||||
| Pre | 27.19 (3.868) | 1.901 | 27.21 (4.710) | 11.924* | F=7.451, P<.001 |
| Post | 26.43 (4.578) | 22.21 (5.041) | Decline | η2p=0.293 | |
| SPMSQ cognition | |||||
| Pre | 2.52 (1.804) | 1.602 | 2.93 (2.336) | −8.153*** | F=6.754, P<.001 |
| Post | 2.14 (1.983) | 5.29 (2.091) | Decline | η2p=0.273 | |
| STAI anxiety | |||||
| Pre | 15.92 (5.043) | 5.462*** | 11.50 (4.346) | −7.870*** | F=9.303, P<.001 |
| Post | 13.22 (3.665) | Improvement | 14.71 (3.730) | Decline | η2p=0.341 |
| GDS depression | |||||
| Pre | 12.97 (5.553) | 3.007** | 12.43 (±5.906) | −3.899** | F=3.005, P<.05 |
| Post | 11.06 (5.089) | Improvement | 15.29 (6.366) | Decline | η2p=0.143 |
| RSES self-esteem | |||||
| Pre | 22.52 (3.671) | 8.390** | 22.14 (4.521) | 2.110 | F=7.700, P<.001 |
| Post | 18.51 (3.089) | Improvement | 23.21 (4.594) | η2p=0.300 | |
| SWLS satisfaction | |||||
| Pre | 25.75 (3.959) | −6.488*** | 24.79 (4.023) | 2.590* | F=6.654, P<.001 |
| Post | 29.25 (3.894) | Improvement | 22.86 (5.289) | Decline | η2p=0.270 |
| LOT-R optimism | |||||
| Pre | 23.62 (5.320) | −5.317*** | 22.21 (5.740) | 1.400 | F=4.561, P<.005 |
| Post | 27.14 (±4.497) | Improvement | 20.64 (4.343) | η2p=0.202 | |
| OARS resources | |||||
| Pre | 3.16 (0.987) | 5.281*** | 2.64 (0.633) | −5.078*** | F=12.591, P<.001 |
| Post | 2.41 (1.010) | Improvement | 4.21 (0.893) | Decline | η2p=0.412 |
| BADL, Katz index | |||||
| Pre | 6.84 (0.482) | 1.350 | 6.57 (0.852) | 1.000 | F=0.913 |
| Post | 6.79 (0.513) | 6.50 (0.855) | |||
| Lawton IADL scale | |||||
| Pre | 6.57 (1.864) | 0.388 | 6.21 (±2.359) | 5.597*** | F=11.843, P<.001 |
| Post | 6.62 (2.082) | 4.14 (1.875) | Decline | η2p=0.397 | |
The significant effects of NPT on the NA group were also observed in the CI group. Sociodemographic variables were controlled in the same way (Table 4). We observed no effects on the benefits of therapy for the following variables: sex (F=0.884, P=.553), educational level (F=1.546, P=.146), occupation (F=1.055, P=.411), marital status (F=0.791, P=.637), number of children (F=1.256, P=.276), or living arrangement (F=1.396, P=.205). In this case, we did not observe a significant age effect (F=1.820, P=.077) like the one found in the normal ageing (NA) group. We did detect, however, the same tendency for younger patients to benefit more from NPT.
DiscussionThe purpose of this study is to assess the effects of group NPT on 4 areas of mental health: overall mental state; emotional well-being (anxiety, depression); other psychological variables (self-esteem, satisfaction, optimism, and quality of social resources); and functional level in daily life (for basic and instrumental activities of daily living). To this end, we analysed pre-treatment and post-treatment results from a group of subjects with normal ageing (NA) and another group with cognitive impairment (CI). Subjects were either assigned to an experimental group (NPT) or a group engaging in leisure, social, or cultural activities (noNPT).
Results show that the patients with normal ageing who underwent this type of NPT experienced significant improvements in general mental state, emotional well-being, and an array of psychological variables related to self-assessed quality of life. However, we did not observe any improvements in performance of activities of daily living. One major reason for this tendency is that this type of group therapy does not seem to have a noticeable impact on task performance by individuals in real situations. Additionally, a test ceiling effect may be present in the scores of subjects with no cognitive impairment. On the other hand, participation in other non-specific activities does not seem to be sufficient to maintain scores for either overall mental state or emotional well-being; both were significantly lower post-treatment. On the other hand, scores on other variables, such as self-esteem and optimism, do remain stable, provided that these types of activities provide satisfaction and stimulation. The decline in the NA-NPT group's performance of IADL is interesting, considering that no subjects in this group showed signs of progression to a clinical entity such as mild cognitive impairment. In any case, it is important to note that in the group with no cognitive impairment, the magnitudes of the effect of the intervention (η2p) are quite low, and the statistical differences found between scores are not clinically significant.
In the group with cognitive impairment, engaging subjects in group NPT seemed to deliver significant improvements in emotional well-being and psychological variables related to self-perceived quality of life. It also appeared to stabilise scores for general mental state and activities of daily living, which is even more interesting. This may in fact be the most relevant finding in our study, in that it suggests that one of the listed objectives for such interventions has been achieved: delaying the progression of cognitive impairment. Therefore, not undergoing this intervention could result in natural progression of cognitive impairment, and this tendency was reflected by the decline in scores for overall mental state and IADL in the CI-noNPT group. There seem to be no significant differences between BADL scores among CI and no-CI subjects, whether or not they participated in the intervention. The study excluded subjects with initial pathological BADL scores, which would have indicated more severe dementia. In this case, the magnitudes of the effect of the intervention (η2p) range from moderate to high, suggesting that subjects with cognitive decline stand to benefit more from NPT than those with normal ageing.
In summary, this study shows how the use of an NPT programme in elderly subjects with or without cognitive impairment may deliver favourable results. On this note, we should highlight that younger subjects and those with cognitive decline seem to benefit the most from this therapy, although the programme appears to constitute an optimal method of primary prevention of cognitive and emotional impairment in all subjects. The programme seems to meet the therapeutic objectives proposed for interventions of this type,6 with the exception of increasing personal independence in activities of daily living. It may be necessary to provide specific and personalised occupational therapy in order to make further progress in that area.
The study's methodological weaknesses are its sample selection process and size (especially once the sample is divided up into subgroups) and how participants were assigned to the experimental groups. It is possible that the individuals who participated in group NPT were intrinsically more likely to benefit from the experience, based on their motives for attending, than subjects who chose not to participate. In any case, this study provides data of interest from the clinical and social/public health perspectives and raises awareness of the beneficial effects of NPT. Furthermore, the possibility of providing NPT to groups remains, in many cases, the only viable option when we consider the large numbers of individuals needing treatment. We therefore recommend creating facilities and dedicating staff and monetary resources to making this type of therapy available to elderly individuals with or without cognitive impairment.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Carballo-García V, et al. Efectos de la terapia no farmacológica en el envejecimiento normal y el deterioro cognitivo: consideraciones sobre los objetivos terapéuticos. Neurología. 2013;28:160–8.