Stroke is currently a major social health problem. For this reason, the Spanish Ministry of Health approved the Stroke National Strategy (SNS) in 2008 to improve the prevention, treatment and rehabilitation of stroke patients. This plan intends to guarantee 24-h, 365-days neurological assistance in the whole country by the end of 2010. Our aim was to analyze the situation of stroke assistance in Spain in 2009.
Material and methodsA committee of neurologists practicing in the different autonomous communities (AC), and who had not participated in the preparation of the SNS, was created. A national survey was performed including the number of stroke units (SU) and their characteristics (monitoring, 24-h/7-day on-call neurology service, nursing staff ratio and the use of protocols), bed ratio of SU/100,000 people, availability of intravenous thrombolysis therapy, neurovascular intervention (NI) and telemedicine.
ResultsWe included data from 145 hospitals. There are 39 SUs in Spain, unevenly distributed. The ratio between SU bed/number of people/AC varied from 1/75,000 to 1/1,037,000 inhabitants; Navarra and Cantabria met the goal. Intravenous thrombolysis therapy is used in 80 hospitals; the number of treatments per AC was between 7 and 536 in 2008. NI was performed in 63% of the AC, with a total of 28 qualified hospitals (although only 1 hospital performed it 24h, 7 days a week in 2009). There were 3 hospitals offering clinical telemedicine services.
ConclusionsAssistance for stroke patients has improved in Spain compared to previous years, but there are still some important differences between the AC that must be eliminated to achieve the objectives of the SNS.
El ictus constituye un importante problema sociosanitario. Por ese motivo, el Ministerio de Sanidad aprobó en 2008 la Estrategia Nacional en Ictus (ENI) con el objetivo de mejorar la prevención, tratamiento y rehabilitación del paciente con ictus. Se pretende garantizar una atención neurológica en todo el país y a cualquier hora del día para final del 2010. Nuestro objetivo fue analizar la situación de la atención al ictus en España en el año 2009.
Material y métodosSe constituyó un comité de neurólogos de las diferentes CC. AA. que no hubieran participado en la ENI. Se elaboró una encuesta nacional que recogió el número de unidades de ictus (UI) y la dotación (monitorización, guardia de neurología 24h/7 días, ratio de enfermería y existencia de protocolos), ratio cama UI/100.000 habitantes, presencia de trombólisis iv, intervencionismo neurovascular (INV) y telemedicina.
ResultadosSe incluyeron datos de 145 hospitales. Existen 39 UI distribuidas de un modo desigual. La relación cama de UI/número de habitantes/comunidad autónoma osciló entre 1/75.000 a 1/1.037.000 habitantes, cumpliendo el objetivo Navarra y Cantabria. Se realiza trombólisis iv en 80 hospitales, el número osciló entre 7-536 tratamientos/CC. AA. durante el año 2008. Se realiza INV en el 63% de las CC. AA., teniendo 28 centros capacitados, aunque sólo 1 la realizaba en 2009 las 24h/7 día. Existen 3 centros con telemedicina.
ConclusionesLa asistencia al ictus ha mejorado en España respecto a unos años atrás, pero todavía existen importantes desigualdades por CC. AA. que deberían superarse si se quiere cumplir el objetivo de la ENI.
Strokes currently constitute the second cause of death and the first cause of dependency in Spain. They give rise to a considerable burden on individuals and on relatives, as well as major social costs.1 Health care for stroke patients has changed with the emergence of stroke units (SUs), as these have demonstrated their efficacy in reducing mortality, the neurological sequelae and the need for institutionalization in various randomized clinical trials and in meta-analyses.2,3 SUs prevent 1 death in every 33 patients treated and 1 institutionalization for every 20 patients.2 This beneficial effect of the SUs is independent of age, gender, aetiological sub-type and severity of the stroke.2 Intravenous thrombolysis is the second therapeutic measure capable of improving the patient's functional prognosis.4–6 However, in order to be administered safely, this technique requires neurologists trained in handling acute stroke patients; this guarantees its safe use and appropriate indication.6,7 It has been suggested that the process should be subject to audits, so it has to have systems in place to record all care activities and the best place to do this in SUs.8,9
The Grupo de Estudio de Enfermedades Cerebrovasculares (Cerebrovascular Disease Study Group, GEECV) of the Sociedad Española de Neurología (Spanish Neurology Society, SEN) has issued some recommendations about how to organize a stroke care system.9–12 The Plan de atención sanitaria al ictus (Stroke Care Plan, PASI) and its subsequent updates established certain levels of stroke care in the light of the available resources, dividing the hospitals into 3 levels.11,12 In this way, we have hospitals with stroke teams, hospitals with SUs and stroke reference hospitals.10,11 The PASI document was the basis used by the Ministry of Health and Social Policy to draw up the National Health System's Stroke Strategy (SS),13 which was signed by all the Regional Governments and is currently in the development phase. The SS was drawn up as a consensus document striving to make stroke care in Spain the best possible, regardless of where the patient lives and the time of day the stroke occurs, and so ensure the right to fair treatment in health care.
Despite the evidence that exists about the benefits of SUs and thrombolysis, most strokes occurring in Spain do not benefit from them, frequently because of the lack of a well-organized stroke care system and appropriate care resources.13–15 The goal of this paper has been to analyze what is the situation of stroke care in Spain at the moment the SS was approved.
Material and methodsA national survey was conducted between January and June 2009, in all the Regions of Spain, except for the self-governing cities of Ceuta and Melilla, under the co-ordination of two representatives from each of the respective regions, all members of the GEECV, applying the premise that they had not taken part in the preparation of the SS. These in turn conveyed the questionnaire to the co-ordinators of the neurology department or cerebral vascular pathology in each hospital. Data from the National Catalogue of Hospitals were collected on 145 Spanish hospitals, without including privately owned hospitals that do not see patients registered with the National Health Service.
Note was taken of the number of SUs and the total number of SU beds so as to calculate the ratio of SUs to population and SU beds to population in terms of the number of inhabitants in each region. In order to verify whether the SUs met the minimum resource levels essential to guarantee their benefits, consideration was given to whether or not they had: a neurologist on duty and physically present 24-h/7 days, non-invasive multi-parameter monitoring, trained nursing personnel with a ratio of 1 to every 4–6 beds and the availability of their own protocols. For the corresponding SU to be considered to have minimum resources available, they had to meet at least 3 of the 4 criteria above, including the sine qua non presence of a duty neurologist.
The number of hospitals with an intravenous thrombolysis programme was recorded together with the number of patients treated at each centre and in each region during 2008. Neurovascular interventionism (NVI) is an alternative treatment for patients in whom intravenous thrombolysis cannot be applied or where it has failed, so the survey also reflected the number of centres with experience in NVI, as well as the timetable in which the administration of this treatment is available. Finally, a note was taken of the existence of telemedicine programmes for the treatment of acute ictus.
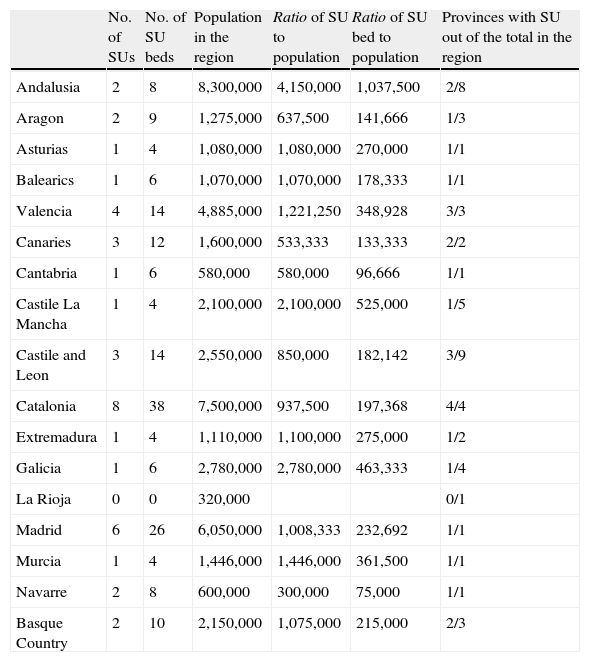
ResultsThe survey included details on 145 hospitals nationwide, with 39 of them identified as having an SU, of which 38 met at least 3 of the 4 criteria considered essential. The implementation of SUs is uneven across Spain as, despite being present in almost all the regions (94%), SUs are only located in 48% of the chief towns in each province (Table 1). This situation is particularly striking in such large regions as Andalusia, which has only one SU in 2 of its 8 provinces. The same could be said for the other large region of Castile La Mancha and for Galicia, where there is only one SU, or in La Rioja, a small region that has no SU at all. Analyzing the ratio of SU beds to the number of inhabitants in each region, we find that only Cantabria and Navarre comply with the target of having 1 SU bed per 100,000 inhabitants. Once more, Andalusia comes off worst (with a ratio of 1 SU bed per 1,037,500 inhabitants), as does La Rioja, which has no SU beds.
Distribution of stroke beds and stroke units in Spain.
| No. of SUs | No. of SU beds | Population in the region | Ratio of SU to population | Ratio of SU bed to population | Provinces with SU out of the total in the region | |
| Andalusia | 2 | 8 | 8,300,000 | 4,150,000 | 1,037,500 | 2/8 |
| Aragon | 2 | 9 | 1,275,000 | 637,500 | 141,666 | 1/3 |
| Asturias | 1 | 4 | 1,080,000 | 1,080,000 | 270,000 | 1/1 |
| Balearics | 1 | 6 | 1,070,000 | 1,070,000 | 178,333 | 1/1 |
| Valencia | 4 | 14 | 4,885,000 | 1,221,250 | 348,928 | 3/3 |
| Canaries | 3 | 12 | 1,600,000 | 533,333 | 133,333 | 2/2 |
| Cantabria | 1 | 6 | 580,000 | 580,000 | 96,666 | 1/1 |
| Castile La Mancha | 1 | 4 | 2,100,000 | 2,100,000 | 525,000 | 1/5 |
| Castile and Leon | 3 | 14 | 2,550,000 | 850,000 | 182,142 | 3/9 |
| Catalonia | 8 | 38 | 7,500,000 | 937,500 | 197,368 | 4/4 |
| Extremadura | 1 | 4 | 1,110,000 | 1,100,000 | 275,000 | 1/2 |
| Galicia | 1 | 6 | 2,780,000 | 2,780,000 | 463,333 | 1/4 |
| La Rioja | 0 | 0 | 320,000 | 0/1 | ||
| Madrid | 6 | 26 | 6,050,000 | 1,008,333 | 232,692 | 1/1 |
| Murcia | 1 | 4 | 1,446,000 | 1,446,000 | 361,500 | 1/1 |
| Navarre | 2 | 8 | 600,000 | 300,000 | 75,000 | 1/1 |
| Basque Country | 2 | 10 | 2,150,000 | 1,075,000 | 215,000 | 2/3 |
There is an intravenous thrombolysis programme co-ordinated by neurologists in 80 hospitals distributed across all the regions. However, 12.5% of these hospitals do not treat more than 5 stroke patients/year. The number of patients treated in 2008 varied widely between regions, from the 457 in Catalonia down to the 7 in La Rioja (Table 2).
Number of intravenous thrombolyses performed by region.
| Region | Number of IV thrombolyses | |
| 1 | Catalonia | 487 |
| 2 | Madrid | 275 |
| 3 | Andalusia | 227 |
| 4 | Castile and Leon | 150 |
| 5 | Basque Country | 126 |
| 6 | Galicia | 88 |
| 7 | Canaries | 87 |
| 8 | Navarre | 70 |
| 9 | Castile La Mancha | 65 |
| 10 | Cantabria | 61 |
| 11 | Valencia | 60 |
| 12 | Balearics | 54 |
| 13 | Asturias | 45 |
| 14 | Aragon | 30 |
| 15 | Extremadura | 30 |
| 16 | Murcia | 30 |
| 17 | La Rioja | 7 |
The results show that 65% of the regions have experience with NVI in at least one hospital. However, only 2 hospitals had this service available 24-h/day and 365 days a year; the rest only operate between 8:00 a.m. and 3:00 p.m.
In 2009, recourse to telemedicine was only available in 3 hospitals in Spain.
DiscussionThe approval of the SS in November 2008 constituted the formal recognition by all the Spanish Health Authorities (at both the State and regional levels) of the social and health-care importance of cerebrovascular disease. At that time, stroke care was very uneven, with some regions where the provision of SUs was good and others where the situation was meagre. The SS approved a series of measures with which to improve overall health care for stroke patients and the different regions were urged to implement them within the term of 2 years. The goal of the GEECV in conducting this survey was to identify the real status of the neurological care of acute stroke in the first half of 2009 and so evaluate whether the targets of the SS are met in the different regions over the years to come.
SUs are the best way of treating strokes as they diminish the probability of death or disability in all the sub-groups of patients, except in patients with an altered level of consciousness, and the benefit is maintained in the long term.15,16 Early neurological evaluation, monitoring and multidisciplinary teamwork entail a better prognosis in terms of mortality or dependency.17,18 Our study shows that the immense majority of the Spanish SUs are well equipped in terms of the variables for nursing ratios, monitoring, continuous care and action protocols. Nonetheless, there are only 39 SUs in Spain, irregularly distributed, with the result that are concentrated in large urban centres, especially in Madrid and Barcelona. This number is clearly insufficient to ensure excellence in health care throughout the country. Only Navarre and Cantabria meet the target of having at least 1 SU bed per 100,000 inhabitants. Particularly worrying is the situation of Andalusia, Galicia, Castile La Mancha and La Rioja.
Intravenous thrombolysis is the treatment that has shown the greatest efficacy in acute cerebral infarction.4,5 However, its impact on stroke care is less than that provided by SUs as, due to the narrow therapeutic window, as well as other restrictions (age, certain prior treatments, possibility of haemorrhagic complications), thrombolytic treatment is only administered – in the best case scenario – to 10–15% of stroke cases, with the most common figures being only 3–5%.18–21 Our survey included data from the 80 centres administering thrombolytic treatment; however, there are only 39 SUs in Spain. It is well known that the percentage of complications with thrombolysis increases at centres performing fewer than 5 treatments a year21 and this happened in 12.5% of these hospitals in our series. The great variability in the number of treatments administered in each region is very striking. Although the number of treatments depends quite a lot on the number of SUs in place in each region, such a great difference from one region to another (7–487 patients/year) cannot be justified just by this fact. It is up to all of us to make an effort to have as many patients as possible treated with t-PA. SUs and centres with a low number of annual treatments must analyze to what extent the problem is in the care chain (recognition of stroke symptoms by the general population, extra-hospital or intra-hospital stroke code or time to action, and the taking of decisions by the neurology).
NVI is a real alternative to IV thrombolysis when this cannot be used or has not been effective. There are a number of techniques (mechanical extraction, intra-arterial thrombolysis or angioplasty) with different indications and therapeutic windows.22–24 Our paper reveals that 65% of the regions have centres with the technical qualifications and expertise to carry out the procedure. Nonetheless, experience in this technique is based almost exclusively on patients treated in a daytime schedule. There were only 2 centres offering this therapy 24h a day. The idea that a patient might or might not benefit from a particular treatment depending on the time of day at which the stroke presents is so unfair that we have no option but to continue working to provide this therapy to our citizens. To this end, organizational solutions must be found to adapt the technical resources in place in each geographical area.
The rechannelling treatment option is limited to patients who are far from the specialist centres and can only call on the district hospitals with professionals who are not neurologists and have no experience with this treatment. On the other hand, not all hospitals have to deal with stroke patients, as has been seen in studies conducted in different countries.21 An alternative facilitating early access to this treatment is telemedicine, which allows the number of stroke patients receiving urgent attention from specialists in neurology to be doubled, the number of thrombolytic treatments to be doubled, the time elapsing until the start of thrombolysis to be significantly reduced by about 50min, and an increase in the number of patients treated in the 0–3h window; moreover, this technique reduces the number of final inter-hospital transfers by a third.25,26 The expansion of this resource in our country is currently insufficient, despite the fact that there are numerous areas of Spain where the geographic conditions of insularity or hard-to-reach locations make it difficult to achieve transfer to the reference centre within the 60min time span considered recommendable.12 So far it has only been implemented in the areas of Barcelona, the Balearic Islands and Seville, with good results in terms of safety and efficacy.27
ConclusionThe purpose of this survey was to analyze the resources available for stroke care at the national level and their regional distribution. Although the situation has improved in recent years, we have been able to document the insufficient roll-out of Stroke Units across the country. In addition, there are major geographical inequalities, as the SUs are concentrated in the large urban centres and their promotion is marginal in some regions. Access to IV thrombolytic treatment is also scant and variable, as are the resources for NVI or telemedicine.
The Stroke Strategy approved by the representatives of the different regions may establish a watershed for stroke care, although it needs to be developed further and we must continue to fight for its improvement.
Conflict of interestThe authors declare that they have no conflict of interest to declare.
FundingThis paper has received partial funding from Laboratorios Ferrer and Sanofi-Aventis.
This paper was submitted for a partial communication to the 61st Annual Meeting of the Spanish Neurology Society.
Please cite this article as: López Fernández JC, et al. Recursos asistenciales en ictus en España 2010: análisis de una encuesta nacional del Grupo de Estudio de Enfermedades Cerebrovasculares. Neurología. 2011; 26: 449–54.