Ischaemic stroke (IS) due to cervical and cerebral artery dissection (CAD) is a rare entity, and few data are available on the use of such reperfusion therapies as intravenous fibrinolysis and mechanical thrombectomy in these patients. We analysed the use of these treatments in patients with IS due to CAD and compared them against patients receiving reperfusion treatment for IS of other aetiologies.
MethodsWe conducted an observational, retrospective, multicentre study of patients with IS due to CAD recorded in the National Stroke Registry of the Spanish Society of Neurology during the period 2011−2019. Comparative analyses were performed between: a) patients with CAD treated and not treated with reperfusion therapies and b) patients treated with reperfusion for IS due to CAD and patients treated with reperfusion for IS due to other causes. Epidemiological data, stroke variables, and outcomes at discharge and at 3 months were included in the analysis.
ResultsThe study included 21,037 patients with IS: 223 (1%) had IS due to CAD, of whom 68 (30%) received reperfusion treatment. Reperfusion treatments were used less frequently in cases of vertebral artery dissection and more frequently in patients with carotid artery occlusion. Compared to patients with IS due to other causes, patients with CAD were younger, more frequently underwent mechanical thrombectomy, and less frequently received intravenous fibrinolysis. Rates of haemorrhagic complications, mortality, and independence at 3 months were similar in both groups.
ConclusionsReperfusion therapy is frequently used in patients with IS due to CAD. The outcomes of these patients demonstrate the efficacy and safety of reperfusion treatments, and are comparable to the outcomes of patients with IS due to other aetiologies.
El ictus isquémico (II) por disección arterial cervico-cerebral (DAC) es una entidad infrecuente y existen pocos datos sobre el uso de terapias de reperfusión como la fibrinolisis intravenosa y la trombectomía mecánica. Se analizó el uso de dichas terapias en pacientes con II por DAC y se comparó con aquellos pacientes reperfundidos con II por otras causas.
MétodoEstudio observacional retrospectivo multicéntrico de pacientes con II por DAC basado en el Registro Nacional de Ictus de la Sociedad Española de Neurología durante el periodo 2011−2019. Se realizaron análisis comparativos entre: a) pacientes con DAC tratados y no con terapias de reperfusión y b) pacientes reperfundidos con II por DAC y pacientes reperfundidos con II por otras causas. Se incluyeron variables epidemiológicas, del ictus y resultados al alta y a los 3 meses.
ResultadosUn total de 21.037 pacientes con II fueron incluidos. 223 (1%) fueron por DAC y 68 (30%) recibieron tratamiento de reperfusión. El uso de tratamientos de reperfusión fue menor en los casos de DAC de arteria vertebral y mayor en los casos de oclusión carotídea. Los pacientes con II por DAC reperfundidos respecto a aquellos con II reperfundidos por otras causas fueron más jóvenes, la TM se utilizó más y la FIV menos. Las complicaciones hemorrágicas, la mortalidad y la autonomía a los 3 meses fueron similares.
ConclusionesLas terapias de reperfusión se usan con frecuencia en los pacientes con II por DAC. Los resultados demuestran eficacia y seguridad y son equiparables a los pacientes tratados con terapias de reperfusión por II de otras causas.
Cervical and cerebral artery dissection (CAD) is an infrequent cause of ischaemic stroke in the general population, accounting for only 2% of all cases. However, it represents one of the most frequent causes in young adults, explaining up to 20% of all cases of ischaemic stroke in individuals younger than 50 years.1–4
In recent decades, the development of such reperfusion therapies as intravenous thrombolysis (IVT) and, more recently, mechanical thrombectomy (MT) has led to a paradigm shift in the treatment of acute ischaemic stroke, significantly reducing mortality and improving functional outcomes. However, few data from real clinical practice are available on the use of these therapies in patients with ischaemic stroke secondary to CAD.
Treatment guidelines recommend IVT in eligible patients with extracranial CAD of less than 3 hours progression (grade Ia) or less than 4.5 hours progression from symptom onset (grade IIa). However, the efficacy of this treatment and the associated haemorrhagic risk in patients with intracranial CAD is less well defined (grade IIb),5 although some studies suggest that the technique presents similar efficacy and safety in these patients and in patients with ischaemic stroke of other aetiology.6–8
Regarding MT, the experience with patients with CAD is even more limited, with few data comparing outcomes against patients with other causes of stroke. Some case series suggest that MT may be effective and safe for patients with proximal intracranial occlusions of the anterior circulation. These patients seem to present similar clinical progression to that of patients treated with IVT.9–11
The objective of this study is to analyse the use of reperfusion therapies in patients with CAD attended at Spanish hospitals. As a secondary objective, we compare progression and prognosis between these patients and those with ischaemic stroke of other aetiologies.
Material and methodsPatientsWe conducted an observational retrospective multicentre study including data from the Spanish Society of Neurology’s national stroke registry, with the participation of a total of 35 Spanish hospitals. The study included all patients diagnosed with ischaemic stroke due to CAD (either traumatic or spontaneous, and at any location [carotid, vertebral, intracranial arteries]) who were admitted to a stroke unit between 2011 and 2019. All cases of transient ischaemic attack were excluded.
We also included patients with ischaemic stroke due to other causes, including large-vessel atherosclerotic stroke, cardioembolic stroke, lacunar stroke, stroke of undetermined aetiology, and stroke of other infrequent aetiology (excluding CAD). Patients were treated according to each hospital’s management protocol.
VariablesWe gathered data on the following demographic and clinical variables: age; sex; history of arterial hypertension, diabetes mellitus, or dyslipidaemia; smoking; alcohol use; history of stroke; use of antiplatelet or anticoagulant drugs; and functional status before stroke (modified Rankin Scale [mRS]).
The following data were also gathered on stroke: code stroke activation, stroke severity (National Institutes of Health Stroke Scale [NIHSS]), localisation of CAD (radiological diagnosis with duplex ultrasound studies of transcranial arteries and supra-aortic trunks, CT, CT angiography, MRI, MRI angiography, or arteriography), type of acute treatment (IVT, MT, or IVT plus MT), occurrence and type of neurological complications (early recurrence, reocclusion, oedema with intracranial hypertension, symptomatic haemorrhagic transformation, other), duration of hospital stay, mortality, and functional independence (mRS < 3) at discharge and at 3 months.
Statistical analysisComparative analyses were performed between: 1) patients with CAD treated and not treated with reperfusion therapies, and 2) patients receiving reperfusion therapies who had ischaemic stroke due to CAD or due to other causes.
Qualitative variables are expressed as number of cases and percentage, and quantitative variables as mean and standard deviation (SD) (with the exception of NIHSS score, which was expressed as median and quartiles 1 and 3 [Q1-Q3]).
We also included patients with ischaemic stroke due to other causes, including large-vessel atherosclerotic stroke, cardioembolic stroke, lacunar stroke, stroke of undetermined aetiology, and stroke of other infrequent aetiology (excluding CAD).
For univariate comparisons between categorical variables, we used the chi-square test, or the Fisher exact test when necessary. Normally distributed quantitative variables were compared with the t test or ANOVA, whereas non-normally distributed quantitative variables were compared with the Mann-Whitney U test. Statistical analysis was performed with the IBM SPSS statistical software package, version 21; statistical significance in the univariate analysis was set at P < .05.
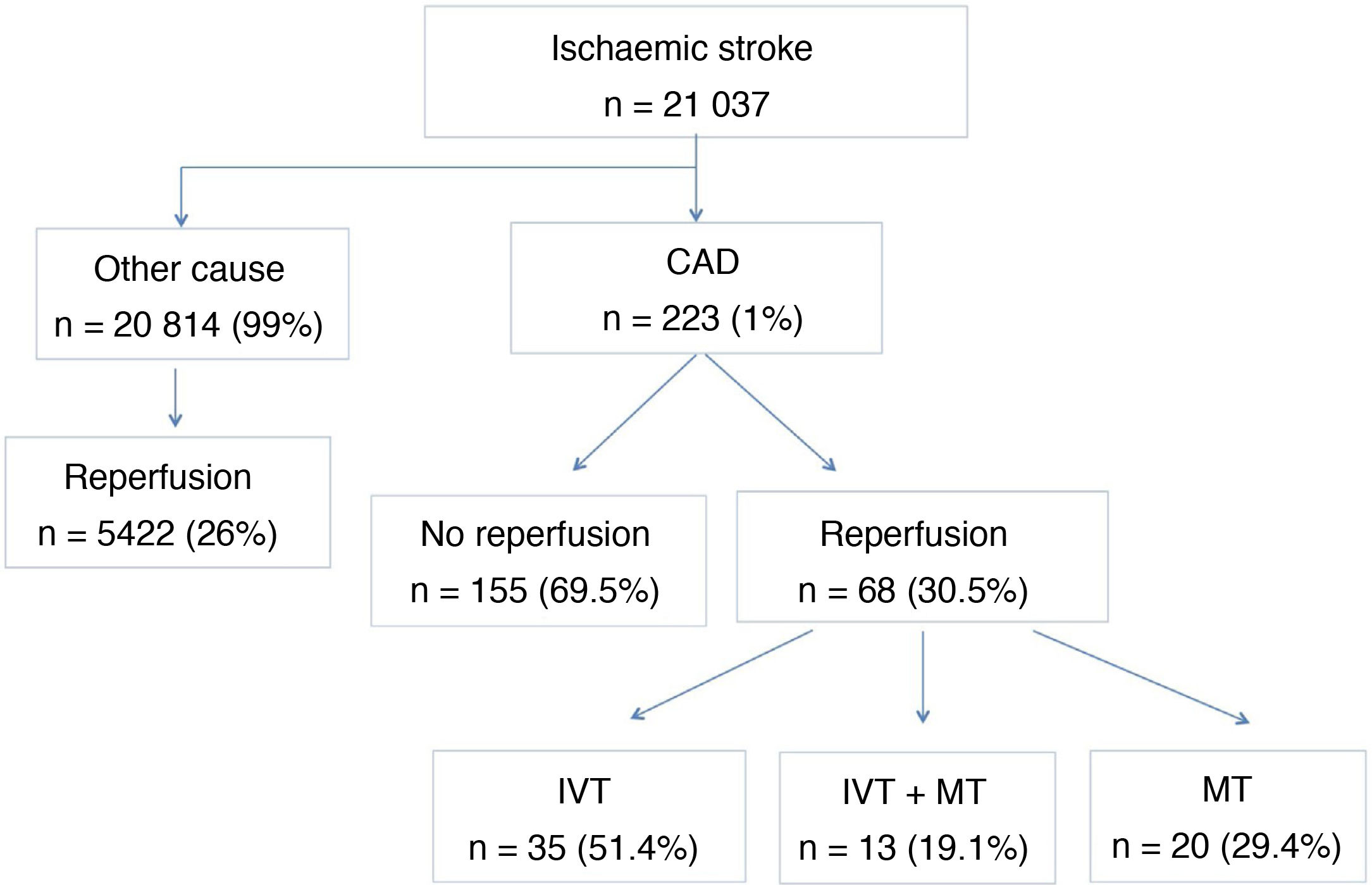
ResultsThe registry included a total of 21 037 cases of ischaemic stroke, of which 20 814 (99%) were due to causes other than CAD. Of these, 5422 (26%) were treated with reperfusion therapy. Of all cases of ischaemic stroke, 223 (1%) were due to CAD, 68 of which (32.5%) were treated with reperfusion therapy in the acute phase. IVT alone was by far the most frequently used reperfusion therapy, in 35 patients (51.4%), followed by MT in 20 patients (29.4%), and sequential treatment with both therapies in 13 patients (19.1%) (Fig. 1).
Regarding loss of follow-up, 3-month follow-up data were not available for 86 of the 223 patients with ischaemic stroke due to CAD; 28 of these had received reperfusion therapy and 58 had not.
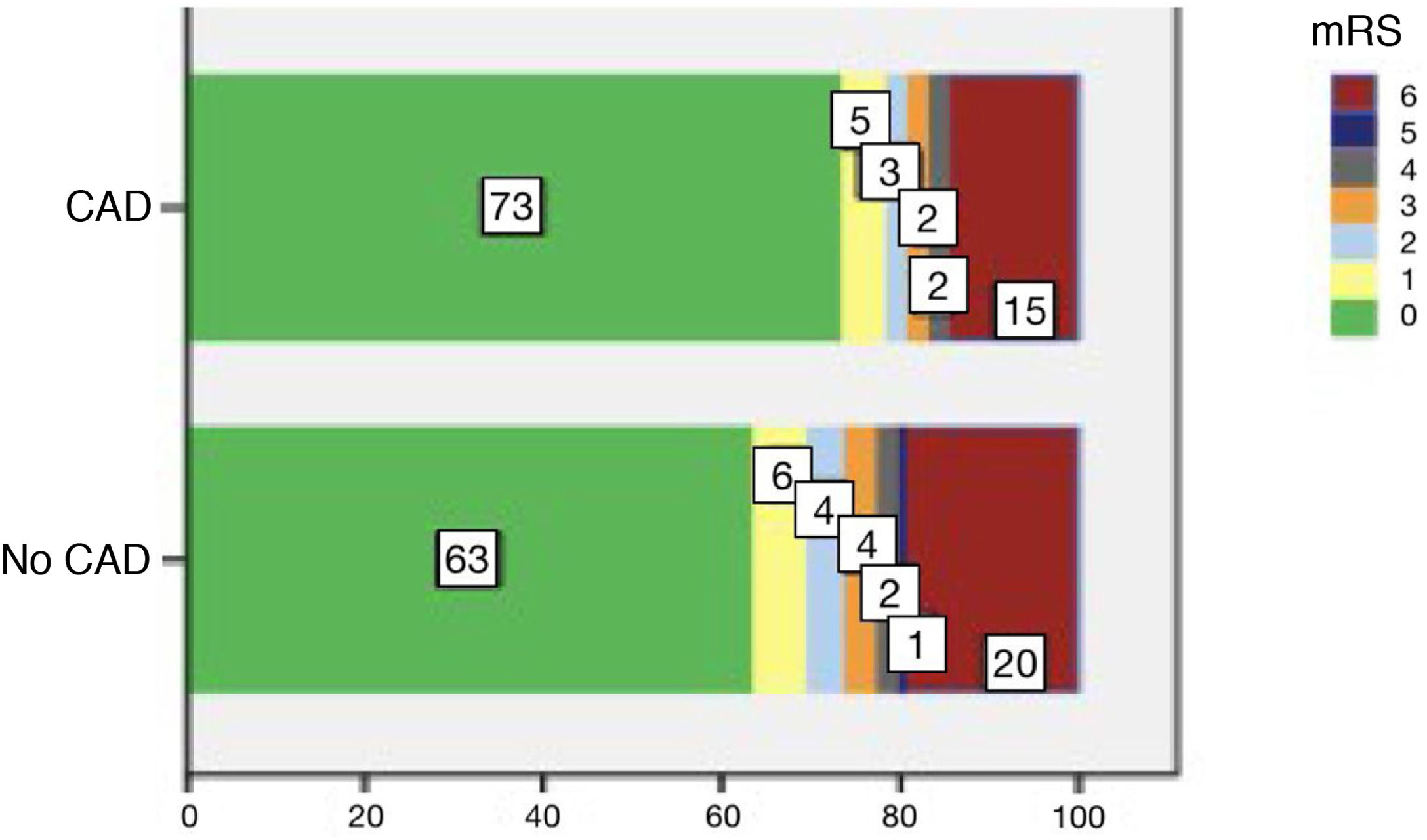
Mean age (SD) in the group of patients with CAD receiving reperfusion therapy (n = 68) was 47.9 (13.2) years, and only 17 (25%) were women (Table 1). Regarding personal history of risk factors, 28% of patients were smokers, 26.5% had dyslipidaemia, and 23.5% had arterial hypertension. All patients were functionally independent before the stroke. In most cases, code stroke was activated (92.6%) and in-hospital management times were below 6 hours from symptom onset (85.3%). Median NIHSS score at admission was 14 (Q1-Q3: 7-20), and the most frequent location of CAD was the carotid artery (58.8%), followed by intracranial arteries (19.1%) and the vertebral artery (11.7%). Twenty-two patients (32.3%) presented neurological complications, with the most frequent being oedema with intracranial hypertension (10.3%) and symptomatic haemorrhagic transformation (8.8%). The mean duration of hospital stay was 8.5 days (Q1-Q3: 6-14.7). Three patients died (4.4%) and 35 (51.5%) were functionally independent at discharge. At 3 months of follow-up (n = 40), 5 patients (12.5%) had died and 33 (82.5%) were functionally independent (Fig. 2).
Demographic characteristics, stroke characteristics, and clinical progression of patients with ischaemic stroke with cervical and cerebral artery dissection receiving and not receiving reperfusion therapy.
| CAD (total) | CAD (reperfusion) | CAD (no reperfusion) | P | |
|---|---|---|---|---|
| n (%) | 223 (100%) | 68 (30.5%) | 155 (69.5%) | |
| Demographic variables | ||||
| Age in years, mean (SD) | 48.8 (12.1) | 47.9 (13.2) | 49.2 (11.6) | .46 |
| Women, n (%) | 73 (32.7%) | 17 (25.0%) | 56 (36.1%) | .11 |
| Arterial hypertension, n (%) | 67 (30.1%) | 16 (23.5%) | 51 (33.0%) | .13 |
| Diabetes mellitus, n (%) | 10 (4.5%) | 5 (7.3%) | 5 (3.2%) | .21 |
| Dyslipidaemia, n (%) | 63 (28.2%) | 18 (26.5%) | 45 (29.0%) | .65 |
| Atrial fibrillation, n (%) | 6 (2.7%) | 3 (4.4%) | 3 (1.9%) | .376 |
| Smoking, n (%) | 63 (28.3%) | 19 (28.0%) | 44 (28.4%) | .94 |
| Alcohol consumption, n (%) | 31 (13.9%) | 25 (36.7%) | 6 (3.8%) | .22 |
| History of stroke, n (%) | 13 (5.8%) | 2 (3.0%) | 11 (7.0%) | .22 |
| Use of antiplatelets, n (%) | 14 (6.3%) | 5 (7.3%) | 9 (5.8%) | .66 |
| Use of anticoagulants, n (%) | 4 (1.8%) | 2 (3.0%) | 2 (1.3%) | .39 |
| Use of statins, n (%) | 24 (10.8%) | 6 (8.8%) | 18 (11.6%) | .53 |
| mRS prior to stroke, median (Q1-Q3) | 0 (0-1) | 0 (0-1) | 0 (0-1) | .3 |
| Stroke characteristics | ||||
| Code stroke activation, n (%) | 141 (63.2%) | 63 (92.6%) | 78 (50.3%) | < .001 |
| Onset-to-NRL time < 6 h, n (%) | 127 (57%) | 58 (85.3%) | 69 (44.5%) | < .001 |
| Onset-to-neuroimaging time < 6 h, n (%) | 128 (57.4%) | 55 (80.9%) | 73 (47.1%) | < .001 |
| NIHSS at admission, median (Q1-Q3) | 5 (2-14) | 14 (7-20) | 3 (1-6) | < .001 |
| NIHSS at 24 h, median (Q1-Q3) | 3 (1-9) | 6 (2-12) | 2 (0-4) | < .001 |
| Intracranial occlusion, n (%) | 55 (24.7%) | 22 (32.3%) | 33 (21.3%) | .06 |
| Localisation of dissection, n (%) | ||||
| Intracranial artery | 30 (13.4%) | 13 (19.1%) | 17 (10.9%) | .10 |
| Carotid artery | 120 (53.8%) | 40 (58.8%) | 80 (51.6%) | .32 |
| Occlusion | 79 (35.4%) | 31 (45.6%) | 48 (31%) | .036 |
| Stenosis | 41 (18.4%) | 9 (13.2%) | 32 (20.6%) | .18 |
| Vertebral artery | 60 (26.9%) | 8 (11.7%) | 52 (33.5%) | .001 |
| Progression | ||||
| Hospital stay (days), median (Q1-Q3) | 9 (6-14) | 8.5 (6-14.7) | 9 (6-13) | .55 |
| Neurological complications (total), n (%) | 48 (21.5%) | 22 (32.3%) | 26 (16.7%) | .072 |
| Symptomatic haemorrhagic transformation, n (%) | 7 (3.1%) | 6 (8.8%) | 1 (0.6%) | .004 |
| Early recurrence, n (%) | 9 (4.0%) | 2 (2.9%) | 7 (4.5%) | .73 |
| Reocclusion, n (%) | 5 (2.2%) | 2 (2.9%) | 3 (1.9%) | .64 |
| Oedema with ICHT, n (%) | 14 (6.3%) | 7 (10.3%) | 7 (4.5%) | .133 |
| Other, n (%) | 12 (5.4%) | 4 (5.9%) | 8 (5.2%) | .759 |
| NIHSS at discharge, median (Q1-Q3) | 1 (0-4) | 1.5 (0-8) | 1 (0-3) | .003 |
| mRS score at discharge, median (Q1-Q3) | 2 (0-4) | 2 (1-3) | 1 (0-3) | .027 |
| Independent (mRS < 3) at discharge, n (%) | 139 (62.3%) | 35 (51.5%) | 104 (67.1%) | .027 |
| In-hospital mortality, n (%) | 6 (2.7%) | 3 (4.4%) | 3 (1.9%) | .37 |
| Follow-up at 3 months | ||||
| Independent (mRS < 3) at 3 months, n (%) | 118 (86.1%) | 33 (82.5%) | 85 (87.6%) | .79 |
| n = 137 | n = 40 | n = 97 | ||
| Mortality at 3 months, n (%) | 14 (10.2%) | 5 (12.5%) | 9 (9.3%) | .54 |
| n = 137 | n = 40 | n = 97 | ||
CAD: cervical and cerebral artery dissection; ICHT: intracranial hypertension; mRS: modified Rankin Scale; NIHSS: National Institutes of Health Stroke Scale; NRL: neurological care; SD: standard deviation.
No differences in demographic characteristics were observed between patients with CAD receiving and not receiving reperfusion therapy (Table 1). However, in the group of patients receiving reperfusion therapy, stroke was more severe (median NIHSS 14 [7-20] vs 3 [1-6] in patients not receiving this treatment; P < .001), vertebral artery dissection was less frequent (11.7% vs 33.5%; P = .001), and carotid artery occlusion was more frequent (45.6% vs 31%; P = .03). Regarding neurological complications, although no statistically significant differences were observed between groups (32.3% vs 16.7%; P = .07), symptomatic haemorrhagic transformation was more frequent among patients receiving reperfusion therapies (8.8% vs 0.6%; P = .004). Although fewer patients in the reperfusion therapy group were functionally independent at discharge (51.5% vs 67.1%; P = .027; n = 68), this was not the case at 3 months of follow-up (82.5% vs 81.6%; P = .9; n = 40). No intergroup differences were found in in-hospital or 3-month mortality rates or at 3 months.
The group of patients undergoing reperfusion therapies due to CAD presented a younger mean age than those with stroke of other aetiology (48 [13.2] vs 72 [11.6] years; P < .001) and included fewer women (25% vs 44.7%; P = .001) (Table 2). Stroke severity (median NIHSS: 14 [7-20] vs 13 [7-19]; P = .37) and the rate of symptomatic haemorrhagic transformation (8.8% vs 7.4%; P = .65) were similar in both groups. Patients with CAD were less frequently treated with IVT (51.4% vs 67.5%; P = .005) and more frequently underwent MT (29.4% vs 18.4%; P = .021). Furthermore, mortality (12.5% vs 8.7%; P = .57) and functional independence at 3 months (82.5% vs 73.6%; P = .31) were also similar in both groups (Fig. 2).
Comparative analysis of patients receiving reperfusion therapy to treat ischaemic stroke due to cervical and cerebral artery dissection and due to other aetiology.
| CAD (reperfusion) | Other aetiology (reperfusion) | P | |
|---|---|---|---|
| n | 68 | 5422 | |
| Age in years, mean (SD) | 48 (13.2) | 72 (11.6) | < .001 |
| Women, n (%) | 17 (25%) | 2426 (44.7%) | .001 |
| NIHSS at admission, median (Q1-Q3) | 14 (7-20) | 13 (7-19) | .37 |
| Symptomatic haemorrhagic transformation, n (%) | 6 (8.8%) | 401 (7.4%) | .65 |
| Early recurrence, n (%) | 2 (2.9%) | 129 (2.4%) | .68 |
| IVT, n (%) | 35 (51.4%) | 3661 (67.5%) | .005 |
| MT, n (%) | 20 (29.4%) | 1000 (18.4%) | .021 |
| IVT + MT, n (%) | 13 (19.1%) | 761 (14%) | .231 |
| Mortality at 3 months, n (%) | 5 (12.5%) | 313 (8.7%) | .57 |
| n = 40 | n = 3588 | ||
| Independent (mRS < 3) at 3 months, n (%) | 33 (82.5%) | 2639 (73.6%) | .31 |
| n = 40 | n = 3588 |
CAD: cervical and cerebral artery dissection; IVT: intravenous thrombolysis; mRS: modified Rankin Scale; MT: mechanical thrombectomy; NIHSS: National Institutes of Health Stroke Scale; SD: standard deviation.
CAD is an infrequent cause of ischaemic stroke, recorded in 1% of our sample of patients with ischaemic stroke and in up to 5.7% of patients with a first stroke of unusual cause in other case series.12 Although CAD is an unusual cause of ischaemic stroke, for which the effectiveness of recanalisation therapies is not yet well defined, our study shows that a high percentage of patients with ischaemic stroke due to CAD (32.5%) receive reperfusion therapy, whether IVT or MT; this percentage is even slightly higher than that observed in patients with other types of stroke (26%). In our study, patients with CAD who received reperfusion therapy were young (mean age of 47.9 years) and most were men (75%). These patients present severe stroke (median NIHSS score of 14), predominantly affecting the carotid artery (58.8%), which frequently presented occlusion (45.6%). Therefore, the frequent use of reperfusion therapies may be explained by the young age of these patients, the severity of ischaemic stroke due to CAD, and the fact that stroke frequently presents in the form of proximal occlusion of the anterior circulation.
In summary, demographic characteristics, stroke severity, and CAD localisation in our sample were similar to those described in other studies including patients undergoing reperfusion to treat ischaemic stroke due to CAD.6,8,9,13
Furthermore, in our study, IVT was the most frequently used reperfusion therapy for CAD (51.4%), although this percentage is still lower than in patients with ischaemic stroke of other aetiology (67.5%). This may be explained by the generalised tendency to follow a conservative approach due to the greater risk of intramural haematoma, symptomatic intracranial haemorrhage, or artery wall rupture associated with alteplase.
Although clinical practice guidelines do not specifically indicate MT for CAD, this was the second most frequent treatment in our sample (alone in 29.4% and in combination with IVT in 19.1%), performed at higher rates than in the group of patients with ischaemic stroke of other aetiology; other studies of MT in patients with CAD report similar results.9,10,14
Regarding clinical outcomes, the rate of functional independence (mRS < 3) at 3 months was similar in patients with CAD receiving (82.5%) and not receiving reperfusion therapy (87.6%) despite the significant difference in stroke severity at admission (median NIHSS: 14 vs 3). Our results for stroke severity, overall mortality, and functional independence in patients with CAD are similar to those of previous studies13,15 and to those observed in the group of patients with ischaemic stroke of other aetiology receiving reperfusion therapy. This suggests that IVT and MT may constitute effective treatments for selected cases of CAD. As reported by other study groups,6–8,15 our results show similar rates of neurological complications, and particularly of symptomatic intracranial haemorrhage, in patients with stroke due to CAD (8.8%) and in patients with stroke of other aetiology (7.4%), suggesting that reperfusion therapy is safe for the treatment of ischaemic stroke due to CAD.
Our study is not without limitations, including those inherent to its retrospective, multicentre design: multicentre registries often include heterogeneous data, but also enable larger samples of infrequent entities such as ischaemic stroke due to CAD.
Though this does not represent a limitation per se, the multicentre registry used in our study was not specifically designed to gather potentially interesting data on certain variables related to recanalisation therapy (reperfusion times, post-reperfusion angiography findings, stenting, etc).
Furthermore, some patients were lost to follow-up at 3 months. In any case, given that CAD is a rare cause of ischaemic stroke, the number of cases included in both groups was considerable, and sufficient to draw conclusions.
ConclusionsReperfusion therapies (IVT, MT, or a combination of both) are frequently used in patients with ischaemic stroke due to CAD, particularly in patients with carotid artery occlusions and more severe strokes.
In line with previous research, our data show that reperfusion therapy presents similar effectiveness and safety in patients with ischaemic stroke due to CAD and in patients with ischaemic stroke of other aetiology.
Conflicts of interestThe authors have no conflicts of interest to declare.