To update the recommendations of the Spanish Society of Neurology regarding lifestyle interventions for stroke prevention.
DevelopmentWe reviewed the most recent studies related to lifestyle and stroke risk, including randomised clinical trials, population studies, and meta-analyses. The risk of stroke associated with such lifestyle habits as smoking, alcohol consumption, stress, diet, obesity, and sedentary lifestyles was analysed, and the potential benefits for stroke prevention of modifying these habits were reviewed. We also reviewed stroke risk associated with exposure to air pollution. Based on the results obtained, we drafted recommendations addressing each of the lifestyle habits analysed.
ConclusionsLifestyle modification constitutes a cornerstone in the primary and secondary prevention of stroke. Abstinence or cessation of smoking, cessation of excessive alcohol consumption, avoidance of exposure to chronic stress, avoidance of overweight or obesity, a Mediterranean diet supplemented with olive oil and nuts, and regular exercise are essential measures in reducing the risk of stroke. We also recommend implementing policies to reduce air pollution.
Actualizar las recomendaciones de la Sociedad Española de Neurología relativas a la actuación sobre los hábitos de vida para la prevención del ictus.
DesarrolloSe ha realizado una revisión de los estudios más recientes relacionados con los hábitos de vida y el riesgo de ictus, incluyendo ensayos clínicos aleatorizados, estudios poblacionales y meta-análisis. Se ha analizado el riesgo de ictus asociado con determinados hábitos de vida como el tabaquismo, el consumo de alcohol, el estrés, la dieta, la obesidad y el sedentarismo, y se ha revisado el potencial beneficio que la modificación de esos hábitos de vida puede aportar en la prevención del ictus. Asimismo, se ha revisado el riesgo de ictus asociado a la exposición a la contaminación atmosférica. A partir de los resultados obtenidos se han redactado unas recomendaciones sobre cada uno de los hábitos de vida analizados.
ConclusionesLa actuación sobre los hábitos de vida constituye una piedra angular en la prevención primaria y secundaria del ictus. La abstinencia o cese del hábito tabáquico, el cese del consumo excesivo de alcohol, evitar la exposición a estrés crónico, evitar el sobrepeso o la obesidad, seguir una dieta mediterránea suplementada con aceite de oliva y frutos secos, y la práctica regular de actividad física son medidas fundamentales para reducir el riesgo de sufrir un ictus. Además, se aconseja desarrollar políticas encaminadas a disminuir la contaminación atmosférica.
Promoting healthy lifestyles is a cornerstone of primary and secondary stroke prevention, as it can also help optimise the control of other established vascular risk factors. This study summarises the main recommendations on smoking, alcohol, stress, obesity, diet, and exercise. We also review the influence of air pollution on the risk of stroke.
To update our recommendations, we performed a literature search of PubMed between August and November 2019, using the following search strategy: lifestyle habits AND stroke, smoking AND stroke, alcohol AND stroke, stress AND stroke, obesity AND stroke, diet AND stroke, physical activity AND stroke, and air pollution AND stroke. We selected the most relevant articles addressing primary and secondary stroke prevention, giving priority to meta-analyses, systematic reviews, and population studies, particularly those published in the last 10 years. Levels of evidence are classified according to the 2016 recommendations of the American College of Cardiology and American Heart Association Task Force, as follows: level A (high-quality evidence from more than one randomised clinical trial [RCT], meta-analyses of high quality RCTs, or one or more RCTs corroborated by high-quality registry studies), level B (moderate-quality evidence from one or more RCTs or meta-analyses of moderate-quality RCTs; or one or more well-designed, well-executed nonrandomised studies, observational studies, or registry studies, or meta-analyses of such studies), or level C (limited-quality data from observational studies or registries with limitations of design or execution). Grades of recommendation were as follows: class I (strong recommendation: benefits far greater than risk), class IIa (moderate recommendation: benefit outweighs risk), class IIb (weak recommendation), and class III (no benefit: benefit is equal to risk).
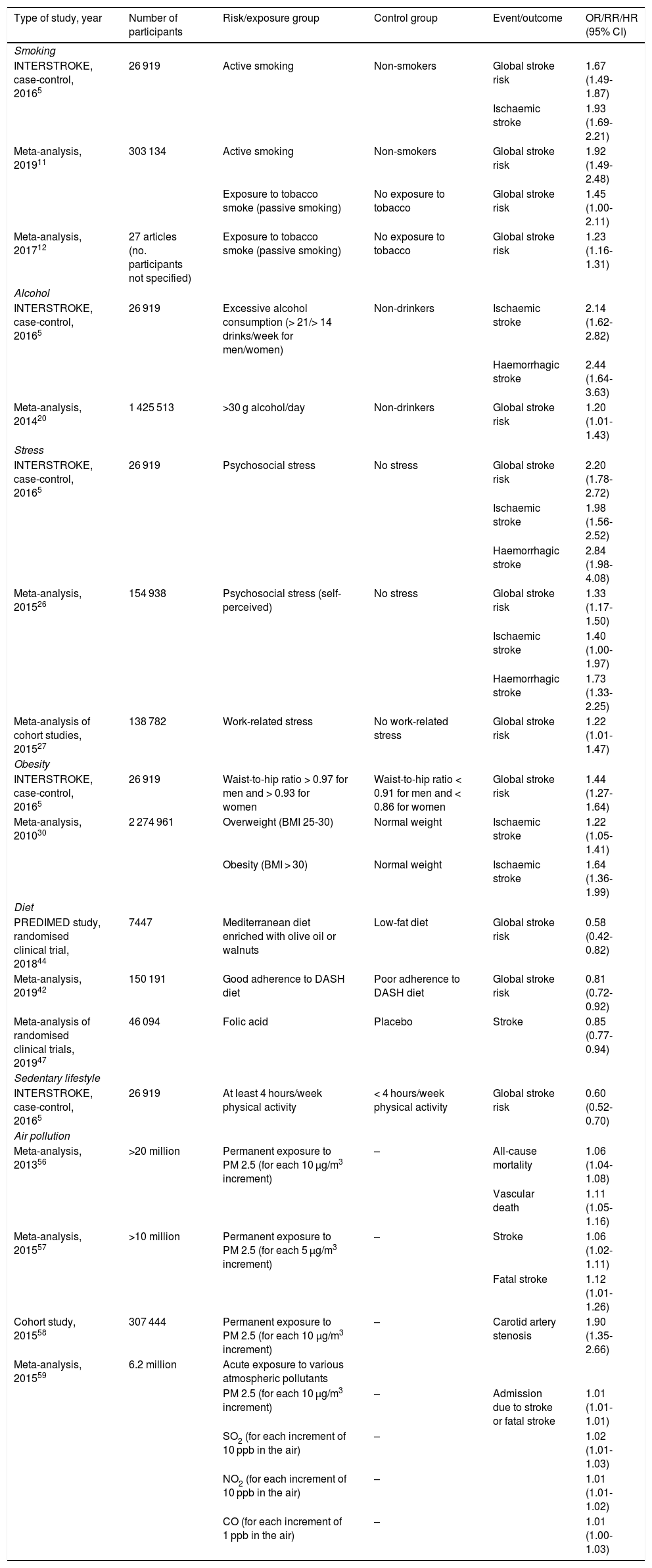
As this consensus statement addresses lifestyles and air pollution, most of the studies reviewed are observational, with few randomised clinical trials analysing interventions; as a result, the highest level of evidence for most of the recommendations is B. Table 1 summarises the most relevant articles for each lifestyle habit and its association with the risk of stroke.
Summary of the main studies analysing the effect of particular lifestyle habits and air pollution on the risk of stroke.
| Type of study, year | Number of participants | Risk/exposure group | Control group | Event/outcome | OR/RR/HR (95% CI) |
|---|---|---|---|---|---|
| Smoking | |||||
| INTERSTROKE, case-control, 20165 | 26 919 | Active smoking | Non-smokers | Global stroke risk | 1.67 (1.49-1.87) |
| Ischaemic stroke | 1.93 (1.69-2.21) | ||||
| Meta-analysis, 201911 | 303 134 | Active smoking | Non-smokers | Global stroke risk | 1.92 (1.49-2.48) |
| Exposure to tobacco smoke (passive smoking) | No exposure to tobacco | Global stroke risk | 1.45 (1.00-2.11) | ||
| Meta-analysis, 201712 | 27 articles (no. participants not specified) | Exposure to tobacco smoke (passive smoking) | No exposure to tobacco | Global stroke risk | 1.23 (1.16-1.31) |
| Alcohol | |||||
| INTERSTROKE, case-control, 20165 | 26 919 | Excessive alcohol consumption (> 21/> 14 drinks/week for men/women) | Non-drinkers | Ischaemic stroke | 2.14 (1.62-2.82) |
| Haemorrhagic stroke | 2.44 (1.64-3.63) | ||||
| Meta-analysis, 201420 | 1 425 513 | >30 g alcohol/day | Non-drinkers | Global stroke risk | 1.20 (1.01-1.43) |
| Stress | |||||
| INTERSTROKE, case-control, 20165 | 26 919 | Psychosocial stress | No stress | Global stroke risk | 2.20 (1.78-2.72) |
| Ischaemic stroke | 1.98 (1.56-2.52) | ||||
| Haemorrhagic stroke | 2.84 (1.98-4.08) | ||||
| Meta-analysis, 201526 | 154 938 | Psychosocial stress (self-perceived) | No stress | Global stroke risk | 1.33 (1.17-1.50) |
| Ischaemic stroke | 1.40 (1.00-1.97) | ||||
| Haemorrhagic stroke | 1.73 (1.33-2.25) | ||||
| Meta-analysis of cohort studies, 201527 | 138 782 | Work-related stress | No work-related stress | Global stroke risk | 1.22 (1.01-1.47) |
| Obesity | |||||
| INTERSTROKE, case-control, 20165 | 26 919 | Waist-to-hip ratio > 0.97 for men and > 0.93 for women | Waist-to-hip ratio < 0.91 for men and < 0.86 for women | Global stroke risk | 1.44 (1.27-1.64) |
| Meta-analysis, 201030 | 2 274 961 | Overweight (BMI 25-30) | Normal weight | Ischaemic stroke | 1.22 (1.05-1.41) |
| Obesity (BMI > 30) | Normal weight | Ischaemic stroke | 1.64 (1.36-1.99) | ||
| Diet | |||||
| PREDIMED study, randomised clinical trial, 201844 | 7447 | Mediterranean diet enriched with olive oil or walnuts | Low-fat diet | Global stroke risk | 0.58 (0.42-0.82) |
| Meta-analysis, 201942 | 150 191 | Good adherence to DASH diet | Poor adherence to DASH diet | Global stroke risk | 0.81 (0.72-0.92) |
| Meta-analysis of randomised clinical trials, 201947 | 46 094 | Folic acid | Placebo | Stroke | 0.85 (0.77-0.94) |
| Sedentary lifestyle | |||||
| INTERSTROKE, case-control, 20165 | 26 919 | At least 4 hours/week physical activity | < 4 hours/week physical activity | Global stroke risk | 0.60 (0.52-0.70) |
| Air pollution | |||||
| Meta-analysis, 201356 | >20 million | Permanent exposure to PM 2.5 (for each 10 μg/m3 increment) | – | All-cause mortality | 1.06 (1.04-1.08) |
| Vascular death | 1.11 (1.05-1.16) | ||||
| Meta-analysis, 201557 | >10 million | Permanent exposure to PM 2.5 (for each 5 μg/m3 increment) | – | Stroke | 1.06 (1.02-1.11) |
| Fatal stroke | 1.12 (1.01-1.26) | ||||
| Cohort study, 201558 | 307 444 | Permanent exposure to PM 2.5 (for each 10 µg/m3 increment) | – | Carotid artery stenosis | 1.90 (1.35-2.66) |
| Meta-analysis, 201559 | 6.2 million | Acute exposure to various atmospheric pollutants | |||
| PM 2.5 (for each 10 µg/m3 increment) | – | Admission due to stroke or fatal stroke | 1.01 (1.01-1.01) | ||
| SO2 (for each increment of 10 ppb in the air) | – | 1.02 (1.01-1.03) | |||
| NO2 (for each increment of 10 ppb in the air) | – | 1.01 (1.01-1.02) | |||
| CO (for each increment of 1 ppb in the air) | – | 1.01 (1.00-1.03) |
BMI: body mass index; CI: confidence interval; DASH: Dietary Approaches to Stop Hypertension; HR: hazard ratio; OR: odds ratio; PM: particulate matter; ppb: parts per billion; RR: relative risk.
Smoking constitutes a healthcare problem worldwide. In Spain, 23.3% of the population is thought to smoke, with nearly half of smokers being younger than 30 years.1 The association between smoking and stroke has been demonstrated in nearly all the population studies conducted in recent decades.2–5 Compared to non-smokers, smokers present twice the risk of stroke and 2-4 times the risk of subarachnoid haemorrhage.6
The mechanisms by which exposure to tobacco smoke can increase the risk of ischaemic stroke and other vascular diseases are numerous, and include increased platelet aggregation, increased fibrinogen levels, reduced HDL cholesterol levels, direct toxicity of such compounds as 1,3-butadiene, and carboxyhaemoglobinaemia.7,8 Tobacco smoke has also been associated with progression of atherosclerosis and early vascular damage.9 Furthermore, smoking has been shown to predispose to atrial fibrillation.10 In smokers, the risk of subarachnoid haemorrhage is associated with an increase in the incidence of brain aneurysms. Smoking can also damage the walls of small arteries, favouring intraparenchymal haemorrhage.7
The INTERSTROKE study, a case-control study conducted across 32 countries on 5 continents and including nearly 30 000 participants, showed that smoking is associated with increased risk of stroke of any type, with an odds ratio (OR) of 1.67 (95% confidence interval [CI], 1.49-1.87), rising to 1.93 (95% CI, 1.69-2.21) for ischaemic stroke. This effect was observed in all populations studied, but is more pronounced in populations from Western Europe, North America, and Australia, with an OR of 2.97. Furthermore, the risk associated with smoking was found to be dose-dependent, with an OR close to 4 in the group of individuals who smoked > 20 cigarettes per day.5 A recent meta-analysis including more than 300 000 participants calculated an OR of 1.92 (95% CI, 1.49-2.48) for stroke in the group of active smokers, and confirmed the linear relationship between number of cigarettes smoked per day and stroke risk, with the risk increasing by 12% for every 5 cigarettes smoked.11 This dose-dependent relationship is less clear, but may also exist, for haemorrhagic stroke.5
Numerous studies have also associated exposure to tobacco smoke in non-smokers (“passive smoking”) with an increase in the risk of stroke, with an OR of 1.45 compared to individuals not exposed to tobacco smoke.11 The effect of passive smoking is also dose-dependent, with the OR reaching 1.56 in the individuals with the highest exposure.12
Smoking cessation reduces the risk of stroke. Active smokers present greater risk of stroke than former smokers (OR: 1.54); this difference is more marked in women (OR: 1.88).11 Risk of stroke has been calculated to reduce by half at one year after quitting, and to reach the same level as non-smokers after 5 years.13 Smoking cessation has been shown to be beneficial for secondary prevention following a stroke or vascular event. A study including nearly 4000 patients with stroke or transient ischaemic attack (TIA) found that the group of patients who quit smoking after the index event presented lower incidence of stroke, myocardial infarction, and death, compared with those who continued smoking (15.7% vs 22.6%; adjusted hazard ratio [HR]: 0.66).14 Furthermore, a recent study conducted in the Netherlands observed that individuals who quit smoking after a first vascular event, in addition to presenting reduced risk of further events and of death (adjusted HR: 0.66 and 0.63, respectively), lived 5 years longer on average, with further vascular events occurring 10 years later.15
Behavioural therapy, psychological counselling, and the use of such treatments as nicotine patches, bupropion, varenicline, and cytisine may be helpful in smoking cessation.16 Varenicline and cytisine seem to be the most effective drugs. The Spanish National Health System has funded treatment with varenicline (partial agonist and, in the presence of nicotine, antagonist of neuronal α4β2 nicotinic acetylcholine receptors) and bupropion (selective inhibitor of neuronal uptake of catecholamines and sympathomimetic analogue) since January 2020 for smoking cessation in high-dependence smokers expressing the desire to quit the habit. The treatment lasts 9-12 weeks and may be prescribed once per year. While the summary of product characteristics includes no explicit contraindication for patients with history of stroke, bupropion is not recommended in patients with history of seizures.
Because they contain nicotine, electronic cigarettes are also associated with increased risk of stroke, although the risk is probably less than that of conventional cigarettes. However, the effect of prolonged exposure to certain potentially toxic chemical components (eg, propylene glycol, aldehydes, aromas, and particulates) is not fully understood.17,18
RecommendationsAbstinence from smoking is recommended for primary and secondary prevention of stroke. Grade of recommendation I, level of evidence B.
Smoking cessation is recommended for all smokers with history of stroke or TIA. Grade of recommendation I, level of evidence B.
Avoiding passive exposure to tobacco smoke may be recommended for stroke prevention. Grade of recommendation IIa, level of evidence B.
AlcoholA clear relationship exists between excessive alcohol consumption and risk of stroke. Unlike in the case of tobacco, the relationship between quantity of alcohol consumed and risk of stroke is not linear. Several studies have confirmed that the relationship between alcohol and stroke risk can be represented graphically with a J-shaped curve, with individuals who drink small or moderate amounts presenting lower risk than non-drinkers, whereas those who drink in excess present significantly higher risk.19 The “protective” effect associated with low or moderate alcohol consumption may be related to the increase in HDL cholesterol levels and reductions in platelet aggregation and plasma fibrinogen concentration.20 Furthermore, consumption of moderate quantities of red wine seems to improve insulin resistance, lipid profile, and endothelial function, compared with other alcoholic drinks.21
Excessive alcohol intake is mainly associated with increased risk of intracerebral haemorrhage. This association may be explained by an increase in arterial blood pressure, a reduction in platelet aggregation, and an increase in the secretion of plasminogen activators by endothelial cells, observed in individuals who drink large amounts of alcohol.20 Consumption of large amounts of alcohol in short periods of time is also associated with the appearance of cardiac arrhythmias including atrial fibrillation, which can cause cardioembolic ischaemic stroke.22
A meta-analysis of 27 studies, including nearly 1.5 million participants, found that individuals who consumed small amounts of alcohol (< 15 g per day) had a lower relative risk (RR) of stroke (0.85 for global stroke risk and 0.81 for ischaemic stroke), and 33% less risk of fatal stroke, compared to non-drinkers. Moderate alcohol consumption (15-30 g per day) was associated with an RR similar to that of non-drinkers, while excessive consumption (> 30 g per day, and particularly > 45 g per day) was associated with increased risk of stroke (ischaemic and haemorrhagic, RR: 1.20). The effect of alcohol dose was greater in women than in men.20
The INTERSTROKE study corroborated these findings, reporting an increase in the risk of all types of stroke, ischaemic stroke, and haemorrhagic stroke (OR values of 2.09, 2.14, and 2.44, respectively) in individuals with excessive alcohol consumption (defined as > 14 drinks/week for women and 21 drinks/week for men, or > 5 drinks in a single day at least once per month) as compared to non-drinkers. However, the “protective” effect of small or moderate amounts of alcohol was only observed in the white population.5
RecommendationsCessation of excessive alcohol consumption (> 30 g per day) is recommended for stroke prevention. Grade of recommendation I, level of evidence B.
StressStress is a feeling of physical or emotional tension caused by situations or thoughts generating a feeling of frustration. Chronic stress is very prevalent in Western lifestyles. Exposure to chronic stress has been associated with increased risk of vascular disease.23–25
The mechanisms by which stress increases the risk of stroke and other vascular diseases are not well understood, although it has been suggested that the activation of the sympathetic nervous system and the hypothalamic-pituitary axis may play a role. Activation of the sympathetic nervous system in response to external stressors triggers the release of catecholamines into the blood, resulting in increased insulin resistance, elevated blood pressure and heart rate, and increased inflammatory response. In turn, the activation of the hypothalamic-pituitary axis leads to an increase in circulating cortisol levels, which also promotes insulin resistance, increases arterial blood pressure, and alters the immune response. All these phenomena would result in endothelial dysfunction, which plays a role in atherosclerosis.23
A meta-analysis of 14 studies including more than 150 000 participants found that individuals exposed to psychosocial stress presented greater risk of stroke, with an HR of 1.33 (similar to that of the effect of diabetes). Stress had a greater impact on the risk of ischaemic stroke than on the risk of haemorrhagic stroke (HR: 1.73 vs 1.40). Furthermore, stress was associated with a greater risk of stroke in women than in men (HR: 1.90 vs 1.24).26
The INTERSTROKE study also identified psychosocial stress as a factor independently associated with increased risk of all types of stroke (OR: 2.20) and ischaemic (OR: 1.98) and haemorrhagic stroke (OR: 2.84). The association between stress and stroke was particularly strong in the Asian population.5
Work-related stress has also been linked to increased risk of stroke. Individuals subjected to high levels of pressure at work (high demand and little control of responsibilities) present a higher risk of stroke than those working in non-stressful roles (RR: 1.22). The effect of work-related stress is greater in women (RR: 1.33), and is particularly associated with ischaemic stroke (RR: 1.58); no statistically significant association has been reported between work-related stress and haemorrhagic stroke.27
RecommendationsAvoiding chronic exposure to personal, family, and work-related stress may be recommended. Grade of recommendation IIa, level of evidence B.
ObesityObesity, defined as body mass index (BMI) greater than 30 kg/m2, is a known risk factor for cardiovascular disease and stroke.28–30 Obesity is a global health problem, particularly in developed countries. According to the 2017 National Health Survey of Spain, 16.7% of women and 18.2% of men in Spain are obese, with 30% of women and 44% of men being overweight (BMI of 25-30 kg/m2). A meta-analysis including over 2 million individuals found that both overweight and obesity were associated with increased risk of ischaemic stroke; no statistically significant association was observed for haemorrhagic stroke.3 Obesity is directly related to such other risk factors as sedentary lifestyle, arterial hypertension, dyslipidaemia, insulin resistance, and diabetes. Central obesity (defined as waist circumference > 102 cm for men and > 88 cm for women) has a greater effect on vascular risk than does overall obesity (defined according to BMI),31 and is the type usually considered in definitions of metabolic syndrome. In the INTERSTROKE study,5 higher waist-to-hip ratios were significantly associated with greater risk of ischaemic and haemorrhagic stroke.
Regarding secondary prevention of stroke, some studies conducted in the last decade have identified a so-called obesity paradox, whereby overweight and obesity are associated with greater survival rates in stroke survivors.32–34 A recent systematic review concluded that the methodological differences between these studies make it difficult to establish a position on the matter, and that further, more robust studies are needed to confirm the association.35
Weight loss can be achieved through the following methods: 1) lifestyle changes (diet and exercise); 2) drugs, such as gastrointestinal lipase inhibitors (orlistat), naltrexone and bupropion combination therapy, or subcutaneous liraglutide; or 3) bariatric surgery, in patients with morbid obesity (BMI > 40 kg/m2).36
The Look AHEAD study assessed the effects of weight loss through an intensive lifestyle intervention (compared to a control group) on vascular risk in over 5000 diabetic patients with overweight/obesity. At 8 years, 50% of participants in the intervention arm achieved a significant reduction in body weight (≥ 5%).37 Individuals whose weight decreased by at least 10% presented a 21% reduction in the risk of a composite of cardiovascular death, non-fatal stroke, non-fatal myocardial infarction, and admission to hospital for angina.38 The authors did not conduct a separate analysis of the risk of stroke.
Subcutaneous liraglutide (an incretin mimetic or GLP-1 agonist used to treat diabetes) contributed to weight loss, compared to orlistat and placebo in patients without diabetes.39 Liraglutide has also been shown to protect against cardiovascular events (cardiovascular death, non-fatal stroke, and/or non-fatal myocardial infarction) in diabetic patients, although protection against stroke was not demonstrated independently.40
RecommendationsAvoidance of overweight and obesity is recommended to reduce the risk of stroke. Grade of recommendation I, level of evidence B.
Diet and nutritionSeveral diets have been studied in the context of primary prevention of ischaemic heart disease and stroke. A diet low in salt (less than 1.5 g/day) and saturated fats and rich in fruits and vegetables, known as the “dietary approaches to stop hypertension” or DASH diet, is considered an effective measure for controlling arterial hypertension.41 Furthermore, a recent systematic review and meta-analysis found that the DASH diet was associated not only with better control of blood pressure, body weight, cholesterol, and diabetes, but also with a reduction in vascular events, with an RR of 0.81 (95% CI, 0.72-0.92) for stroke.42 The Mediterranean diet follows a similar approach, with abundant intake of fruits, vegetables, legumes, and nuts, olive oil as the main source of fat, moderate/large quantities of fish, and reduced consumption of red meat and sweetened drinks. A recent review on the Mediterranean diet and stroke prevention, which included 9 systematic reviews and 6 meta-analyses, concluded that good adherence to the Mediterranean diet is inversely correlated with stroke risk.43 In Spain, the PREDIMED randomised clinical trial, which included 7447 patients with high vascular risk, is noteworthy. At 5 years of follow-up, participants who received a Mediterranean diet supplemented with walnuts and/or olive oil presented significantly fewer vascular events (vascular death, myocardial infarction, or stroke) than controls, who received low-fat diets. Stroke was assessed independently as a secondary outcome, with an HR of 0.58 (95% CI, 0.42-0.82) in participants receiving a Mediterranean diet.44 In a case-control study conducted in Barcelona, including 300 patients with ischaemic stroke and 300 healthy controls, significant differences were detected between groups in dietary patterns. Patients with stroke ate more protein, more cholesterol, more breaded foods, and fewer probiotics.45
A Cochrane review conducted in 2017 included various clinical trials performed in the last 20 years to evaluate supplementation with B vitamins (vitamins B6, B12, and B9 [folic acid]), which would play an intermediate role by lowering homocysteine levels; the study did not find a net benefit in the prevention of vascular events or vascular death.46 With respect to stroke prevention, a meta-analysis of 10 clinical trials (over 44 000 patients with history of vascular disease and not presenting kidney failure), with a mean follow-up period of 7 years, found these supplements (alone or in combination) to have a small net benefit compared to placebo, with an RR of 0.90 (95% CI, 0.82-0.99).46 However, the studies analysed presented significant methodological differences in terms of the doses and supplements used; the authors reported their results cautiously, and were unable to give explicit recommendations. A meta-analysis published in 2019 included 9 clinical trials studying folic acid supplementation, with a total of 46 094 patients with history of cardiovascular or cerebrovascular disease, and concluded that folic acid supplementation reduces the risk of stroke, with an RR of 0.85 (95% CI, 0.77-0.94), but not the risk of coronary heart disease or cardiovascular mortality.47 The meta-analysis only observed a benefit for stroke prevention with administration of folic acid in isolation, and not for combination treatment with other B vitamins. Regarding dose, this benefit was only observed in patients receiving < 2 mg per day. Furthermore, the benefit was only observed for follow-up periods longer than 40 months.
RecommendationsMediterranean diet supplemented with nuts and virgin olive oil is recommended to reduce the risk of stroke. Grade of recommendation I, level of evidence A.
Supplementation with low doses of folic acid may be beneficial to reduce the risk of stroke in patients with history of vascular disease. Grade of recommendation IIa, level of evidence B.
Sedentary lifestyleSedentary lifestyles, which are highly prevalent in Western societies, are associated with other risk factors including obesity, dyslipidaemia, arterial hypertension, and metabolic syndrome. According to the 2017 National Health Survey of Spain, 40.0% of Spanish women and 31.9% of men report having sedentary lifestyles. In the INTERSTROKE study, regular moderate or intense exercise (at least 4 hours per week) was associated with lower overall risk of stroke (OR: 0.60; 95% CI, 0.52-0.70), with a similar effect on ischaemic and haemorrhagic stroke.5 Multiple reviews and meta-analyses have demonstrated that regular exercise is associated with lower incidence of cardiovascular and cerebrovascular disease, and lower rates of cardiovascular death and all-cause mortality.48 Exercise can be measured in metabolic equivalents (MET). One MET is defined as the energy consumed while sitting, in the resting state. The MET value of an activity or exercise is calculated as a function of that value, and is usually multiplied by the number of minutes of activity per week. Moderate activity is defined as that using 3-6 MET minutes, causing sweating or increased heart rate (eg, brisk walking), and vigorous activity is equivalent to > 6 MET minutes (eg, running or aerobics). A meta-analysis found that physical activity of over 8000 MET/week was associated with lower risk of incident stroke (RR of 0.74 [95% CI, 0.66-0.81]) than activity of < 600 MET/week.48 Any activity is better than none, and it is recommended that the general population perform at least 150 minutes/week of moderate activity (eg, by walking for 30 minutes 5 days per week), 75 minutes/week vigorous exercise, or an equivalent combination; both aerobic and resistance activities are beneficial.49 In addition to its effect on stroke prevention, having performed exercise prior to stroke may act as a protective factor in brain ischaemia, improving prognosis.50
Few data are available on the impact of exercise on secondary stroke prevention, except regarding its benefits in controlling vascular risk factors and cardiorespiratory capacity. A sub-analysis conducted as part of the SAMMPRIS study (including patients with ischaemic stroke due to atherosclerosis of an intracranial artery and assigned to receive medical treatment, who responded to a telephone interview addressing modifiable risk factors, including physical activity) found that only patients who performed more than 30 minutes of moderate physical activity at least 3 days per week achieved a greater reduction in recurrent vascular events (stroke, myocardial infarction, or vascular death) at 3 years.51
Regarding interventions to encourage exercise (besides medical counselling), the PREDIMED-plus study demonstrated the efficacy of an educational programme, which increased participants’ physical activity levels at one year of follow-up52; similarly, the ICARUSS study confirmed the benefits of multidisciplinary control of modifiable risk factors, including the promotion of physical activity, in patients with history of stroke.53
RecommendationsModerate physical activity for 150 minutes/week or vigorous activity for 75 minutes/week is recommended for reducing the risk of stroke. Grade of recommendation I, level of evidence B.
Air pollutionExposure to air pollution is a significant public health issue. In 2015, air pollution was one of the main causes of morbidity and mortality globally, causing 6.5 million deaths and 167.3 million disability-adjusted life years lost. Numerous epidemiological studies have demonstrated a direct association between air pollution and the incidence of atherosclerosis. Air pollution is estimated to be responsible for 19% of cardiovascular deaths and 21% of stroke deaths.54,55
The main pollutants that represent health risks are particulate matter and such gases as ozone (O3), sulphur dioxide (SO2), carbon monoxide (CO), and nitrogen dioxide (NO2). Particulate matter is categorised according to the size of the particles, as follows: coarse particles or PM 10 (diameter of 10 µm or less), fine particles or PM 2.5 (diameter of 2.5 µm or less), and ultrafine particles or nanoparticles (diameter below 0.1 µm). Nanoparticles and fine particles are most frequently involved in vascular disease. Several mechanisms have been proposed to explain the role of these pollutants in vascular disease, including inflammatory phenomena, altered endothelial function, changes in blood viscosity, altered vascular homeostasis, and epigenetic mechanisms.55
Exposure to air pollution can be classified as chronic or acute (pollution “peaks”).
Multiple studies have shown that individuals living in areas with permanently high pollution levels present greater risk of vascular events. A meta-analysis showed that for every 10 µg/m3 increase in atmospheric PM 2.5 levels, cumulative risk of all-cause mortality increased by 6% and risk of cardiovascular death increased by 11%.56 Another meta-analysis demonstrated that every 5 µg/m3 increase in atmospheric PM 2.5 levels was associated with an increase in the risk of stroke (HR: 1.064) and fatal stroke (HR: 1.125).57 Furthermore, a recent study found that chronic exposure to PM 2.5 is independently associated with carotid artery stenosis.58
In large urban centres, pollution peaks sometimes occur in which the levels of particulate matter and pollutant gases rise significantly for short periods of time. This acute exposure to pollutants has been linked to increasing incidence of vascular events, and particularly stroke. In a meta-analysis reviewing over 6 million strokes in 28 countries across the world, the rate of hospital admissions and mortality due to stroke increased on days when increased levels of air pollution were recorded. The association was particularly clear for increases in levels of PM 2.5, SO2, NO2, and CO.59
Besides air pollution, other environmental factors including noise pollution, limited access to green spaces, and global warming have also been found to be associated with increased stroke risk and/or severity.60,61
RecommendationsPublic health policies to reduce air pollution are recommended for their potential effect in stroke prevention. Grade of recommendation I, level of evidence B.
Conflicts of interestThe authors have no conflicts of interest to declare.
Both authors have contributed equally as first authors.
Please cite this article as: García Pastor A, López-Cancio Martínez E, Rodríguez-Yáñez M, Alonso de Leciñana M, Amaro S, Arenillas JF, et al. Recomendaciones de la Sociedad Española de Neurología para la prevención del ictus. Actuación sobre los hábitos de vida y la contaminación atmosférica. Neurología. 2021;36:377–387.