Hereditary neuropathy with liability to pressure palsies (HNPP) is a rare, autosomal dominant disease affecting peripheral myelin, which manifests as recurrent, and usually transient, painless motor and/or sensory neuropathies.1–3 Neuropathies are triggered by minor trauma or repetitive movements with compression and traction of peripheral nerves. The most frequent forms of presentation affect the peroneal and the ulnar nerves. Brachial plexopathy occurs in 11%-20% of the cases over the natural course of the disease, but it is an unusual clinical manifestation; bilateral presentation is even rarer.1,2 We present the clinical case of a patient with HNPP presenting as a bilateral brachial plexopathy.
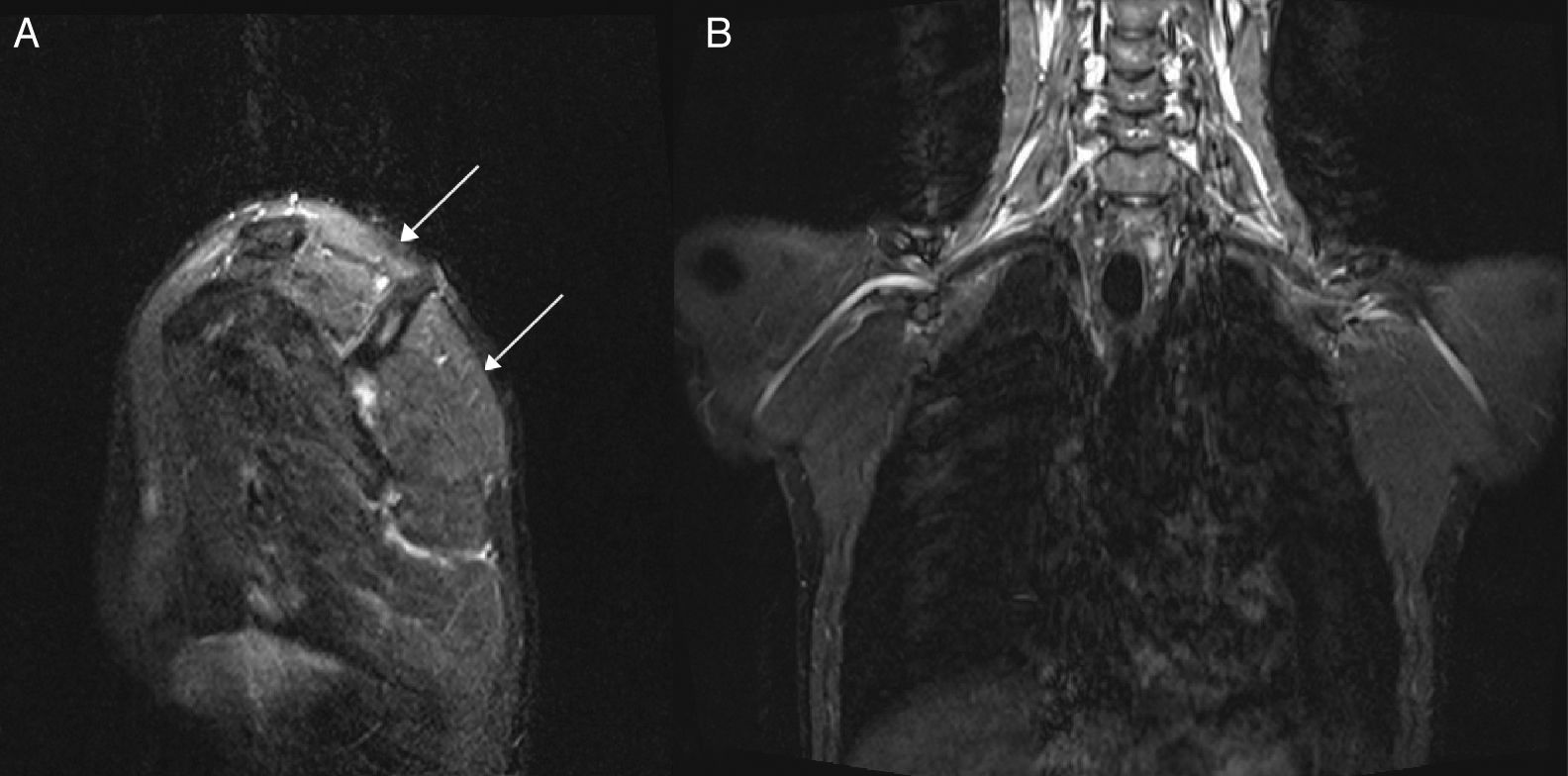
Our patient was a 22-year-old man with no relevant personal or family history who was transferred to our department due to proximal weakness of the left arm which had persisted for 3 weeks. The patient noticed weakness upon waking but experienced no pain; he had no history of trauma, surgery, or infection. Curiously, he presented similar symptoms in the right arm 4 months earlier, with proximal, painless weakness and paraesthesia in the hand, from which he was still recovering. Again, our patient noticed all these symptoms upon waking. During the first event, an electroneuromyography (EMG) study (Tables 1 and 2) revealed right brachial plexopathy, extending throughout the upper trunk, and a slightly prolonged distal latency in the right motor median nerve, sensory median nerve, and sensory ulnar nerve. When the second event occurred, the patient was transferred to our department for observation. Examination revealed 4/5 muscle strength in abduction and external rotation of the right shoulder, and 3/5 muscle strength in abduction and 4/5 in external rotation of the left shoulder. No paresis was observed in the remaining muscle segments; deep tendon reflexes were weak in the upper limbs; no further abnormalities were observed. An EMG study (Tables 1 and 2) revealed left brachial plexopathy with a major lesion of the upper trunk and neuropathy of the left ulnar nerve at the elbow; no further alterations were observed. Cervical magnetic resonance imaging (MRI) results were normal. A high-resolution MRI of the brachial plexuses (Fig. 1) showed increased signal in the left supraspinatus, infraspinatus, and teres minor muscles, suggesting muscle denervation with no structural lesion of the left brachial plexus. Blood analyses, including an autoimmune profile, yielded normal results. Since the clinical symptoms and neurophysiological results suggested a diagnosis of HNPP, we requested genetic testing; this revealed a heterozygous deletion (17p11.2-12) in the peripheral myelin protein 22 gene (PMP22), which confirmed the diagnosis. Our patient recovered muscle strength in his arms with rehabilitation; preventive measures were adopted.
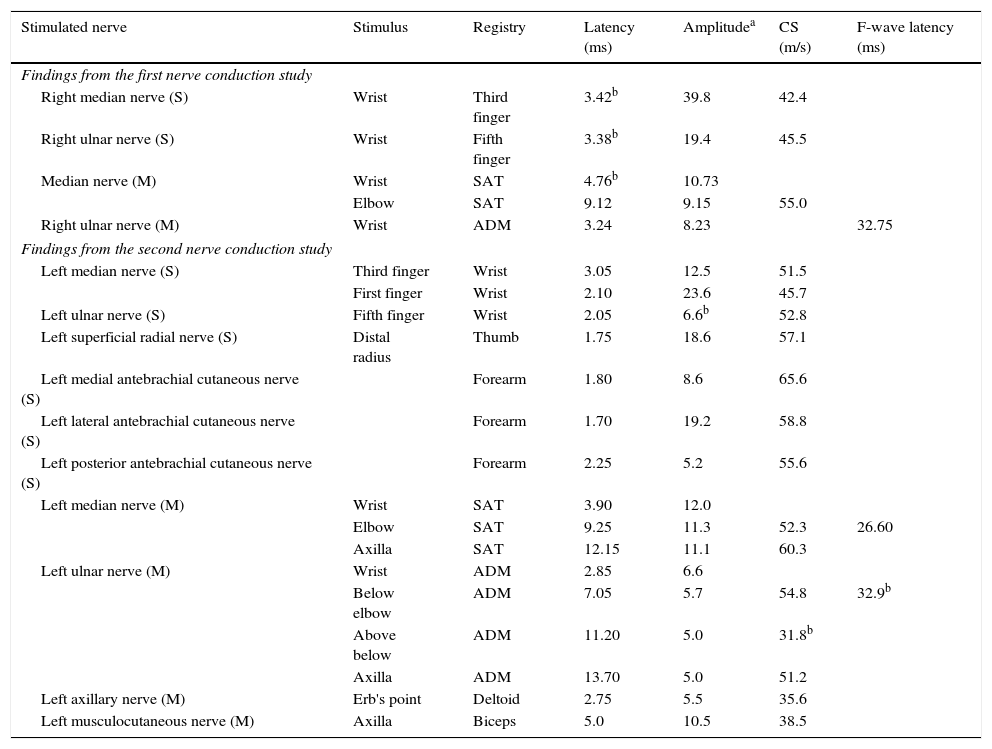
Results from the nerve conduction studies.
| Stimulated nerve | Stimulus | Registry | Latency (ms) | Amplitudea | CS (m/s) | F-wave latency (ms) |
|---|---|---|---|---|---|---|
| Findings from the first nerve conduction study | ||||||
| Right median nerve (S) | Wrist | Third finger | 3.42b | 39.8 | 42.4 | |
| Right ulnar nerve (S) | Wrist | Fifth finger | 3.38b | 19.4 | 45.5 | |
| Median nerve (M) | Wrist | SAT | 4.76b | 10.73 | ||
| Elbow | SAT | 9.12 | 9.15 | 55.0 | ||
| Right ulnar nerve (M) | Wrist | ADM | 3.24 | 8.23 | 32.75 | |
| Findings from the second nerve conduction study | ||||||
| Left median nerve (S) | Third finger | Wrist | 3.05 | 12.5 | 51.5 | |
| First finger | Wrist | 2.10 | 23.6 | 45.7 | ||
| Left ulnar nerve (S) | Fifth finger | Wrist | 2.05 | 6.6b | 52.8 | |
| Left superficial radial nerve (S) | Distal radius | Thumb | 1.75 | 18.6 | 57.1 | |
| Left medial antebrachial cutaneous nerve (S) | Forearm | 1.80 | 8.6 | 65.6 | ||
| Left lateral antebrachial cutaneous nerve (S) | Forearm | 1.70 | 19.2 | 58.8 | ||
| Left posterior antebrachial cutaneous nerve (S) | Forearm | 2.25 | 5.2 | 55.6 | ||
| Left median nerve (M) | Wrist | SAT | 3.90 | 12.0 | ||
| Elbow | SAT | 9.25 | 11.3 | 52.3 | 26.60 | |
| Axilla | SAT | 12.15 | 11.1 | 60.3 | ||
| Left ulnar nerve (M) | Wrist | ADM | 2.85 | 6.6 | ||
| Below elbow | ADM | 7.05 | 5.7 | 54.8 | 32.9b | |
| Above below | ADM | 11.20 | 5.0 | 31.8b | ||
| Axilla | ADM | 13.70 | 5.0 | 51.2 | ||
| Left axillary nerve (M) | Erb's point | Deltoid | 2.75 | 5.5 | 35.6 | |
| Left musculocutaneous nerve (M) | Axilla | Biceps | 5.0 | 10.5 | 38.5 | |
SAT, short abductor muscle of thumb; ADM, abductor digiti minimi muscle; M, motor; S, sensory; CS, conduction speed.
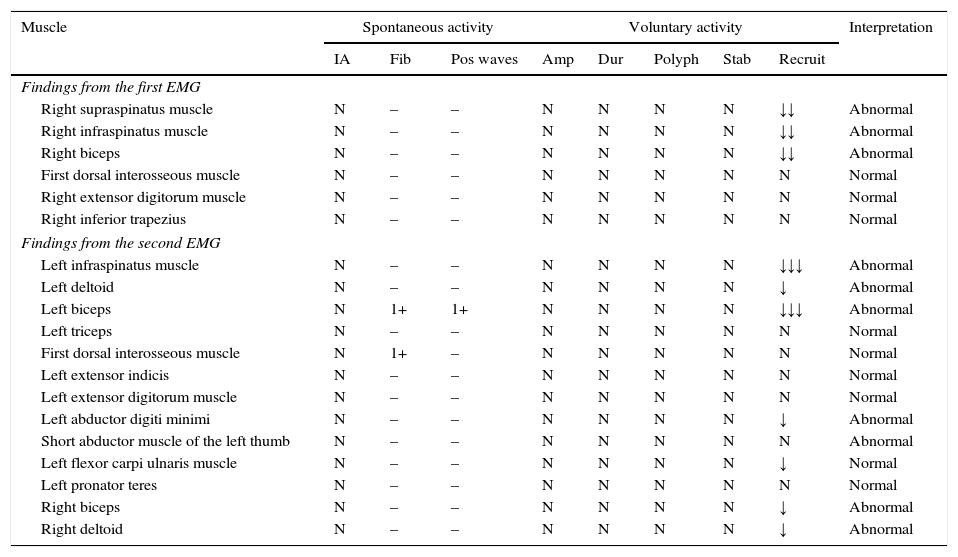
Results from the EMG evaluation.
| Muscle | Spontaneous activity | Voluntary activity | Interpretation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| IA | Fib | Pos waves | Amp | Dur | Polyph | Stab | Recruit | ||
| Findings from the first EMG | |||||||||
| Right supraspinatus muscle | N | – | – | N | N | N | N | ↓↓ | Abnormal |
| Right infraspinatus muscle | N | – | – | N | N | N | N | ↓↓ | Abnormal |
| Right biceps | N | – | – | N | N | N | N | ↓↓ | Abnormal |
| First dorsal interosseous muscle | N | – | – | N | N | N | N | N | Normal |
| Right extensor digitorum muscle | N | – | – | N | N | N | N | N | Normal |
| Right inferior trapezius | N | – | – | N | N | N | N | N | Normal |
| Findings from the second EMG | |||||||||
| Left infraspinatus muscle | N | – | – | N | N | N | N | ↓↓↓ | Abnormal |
| Left deltoid | N | – | – | N | N | N | N | ↓ | Abnormal |
| Left biceps | N | 1+ | 1+ | N | N | N | N | ↓↓↓ | Abnormal |
| Left triceps | N | – | – | N | N | N | N | N | Normal |
| First dorsal interosseous muscle | N | 1+ | – | N | N | N | N | N | Normal |
| Left extensor indicis | N | – | – | N | N | N | N | N | Normal |
| Left extensor digitorum muscle | N | – | – | N | N | N | N | N | Normal |
| Left abductor digiti minimi | N | – | – | N | N | N | N | ↓ | Abnormal |
| Short abductor muscle of the left thumb | N | – | – | N | N | N | N | N | Abnormal |
| Left flexor carpi ulnaris muscle | N | – | – | N | N | N | N | ↓ | Normal |
| Left pronator teres | N | – | – | N | N | N | N | N | Normal |
| Right biceps | N | – | – | N | N | N | N | ↓ | Abnormal |
| Right deltoid | N | – | – | N | N | N | N | ↓ | Abnormal |
IA, insertion activity; Amp, amplitude; Dur, duration; EMG, electromyography; Stab, stability; Fib, fibrillation; Polyph, polyphase; Pos, positive; Recruit, recruitment.
High resolution (3-tesla) MRI neurography sequences: sagittal STIR (short inversion time inversion recovery) sequence (A) showing an increased signal (arrows) in the left supraspinatus, infraspinatus, and teres minor muscles; coronal STIR sequence (B) showing no morphological alterations of the brachial plexi.
HNPP normally manifests during the second or third decade of life, although age of onset varies greatly.3,4 Diagnosis requires a clinical history of recurrent neuropathies, a consistent family history of autosomal dominant inheritance, evidence of focal demyelinating sensorimotor neuropathies at entrapment sites and/or diffuse demyelinating sensorimotor polyneuropathy in nerve conduction studies, focal myelin thickening in nerve biopsy, when applicable, and lastly, confirmation from genetic testing.1–4 Most patients present a deletion in chromosome 17p11.2, including the PMP22 gene, and the remaining patients present a mutation of the gene itself.5,6
The phenotypic profile of HNPP is highly heterogeneous, even within a single family. Brachial plexopathy may manifest in some patients, but HNPP is generally associated with other recurrent mononeuropathies, presenting throughout the course of the disease.1,2 The short disease duration in our patient may explain the lack of symptoms caused by the action of another nerve, and the negative family history may be explained by an asymptomatic disease in one of his parents, or a de novo deletion in our patient. In the literature, only a small number of families with HNPP present recurrent brachial plexopathies as the sole clinical manifestation,7–12 and symptoms in the majority of those families started upon waking, which indicates a greater vulnerability of the brachial plexus to mechanical factors during sleep.11
Beyond HNPP, differential diagnosis of non-traumatic brachial plexopathy must consider compressive lesions, hereditary neuralgic amyotrophy, and idiopathic neuralgic amyotrophy (Parsonage–Turner syndrome). However, in these pathologies, pain is one of the main manifestations, and the latter 2 entities are characteristically associated with localised axonal damage to the plexus in neurophysiological studies.10,11
We should, then, consider HNPP when assessing patients with non-traumatic brachial plexopathies with no pain and mainly manifesting as demyelination. To our knowledge, this is the first case of HNPP manifesting as bilateral brachial plexopathy to be published.
FundingThis study received no public or private funding.
Conflicts of interestThe authors have no conflicts of interest to declare. We obtained the patient's informed consent to publish his case.
Please cite this article as: Morgado J, Sousa AP, Alves P, Medeiros L. Plexopatía braquial bilateral como forma de presentación de la neuropatía hereditaria con parálisis sensible a la presión. Neurología. 2017;32:626–629.