Huntington disease (HD), the most frequent genetically determined type of chorea, is an autosomal dominant, progressive neurodegenerative disorder that causes physical, cognitive, and psychological impairment.1 Physical exercise is considered a useful rehabilitation therapy in HD, although it is yet to be determined what type provides the greatest potential benefits in slowing progression of the disease.2 Nordic walking may be an interesting physical therapy in HD due to the low level of fitness required, the simplicity of the exercise, and the reported effects on independence and motor symptoms in patients presenting neurodegenerative symptoms.3 We describe the case of a patient with early-intermediate stage HD who presented changes in functional status after participating in a Nordic walking programme.
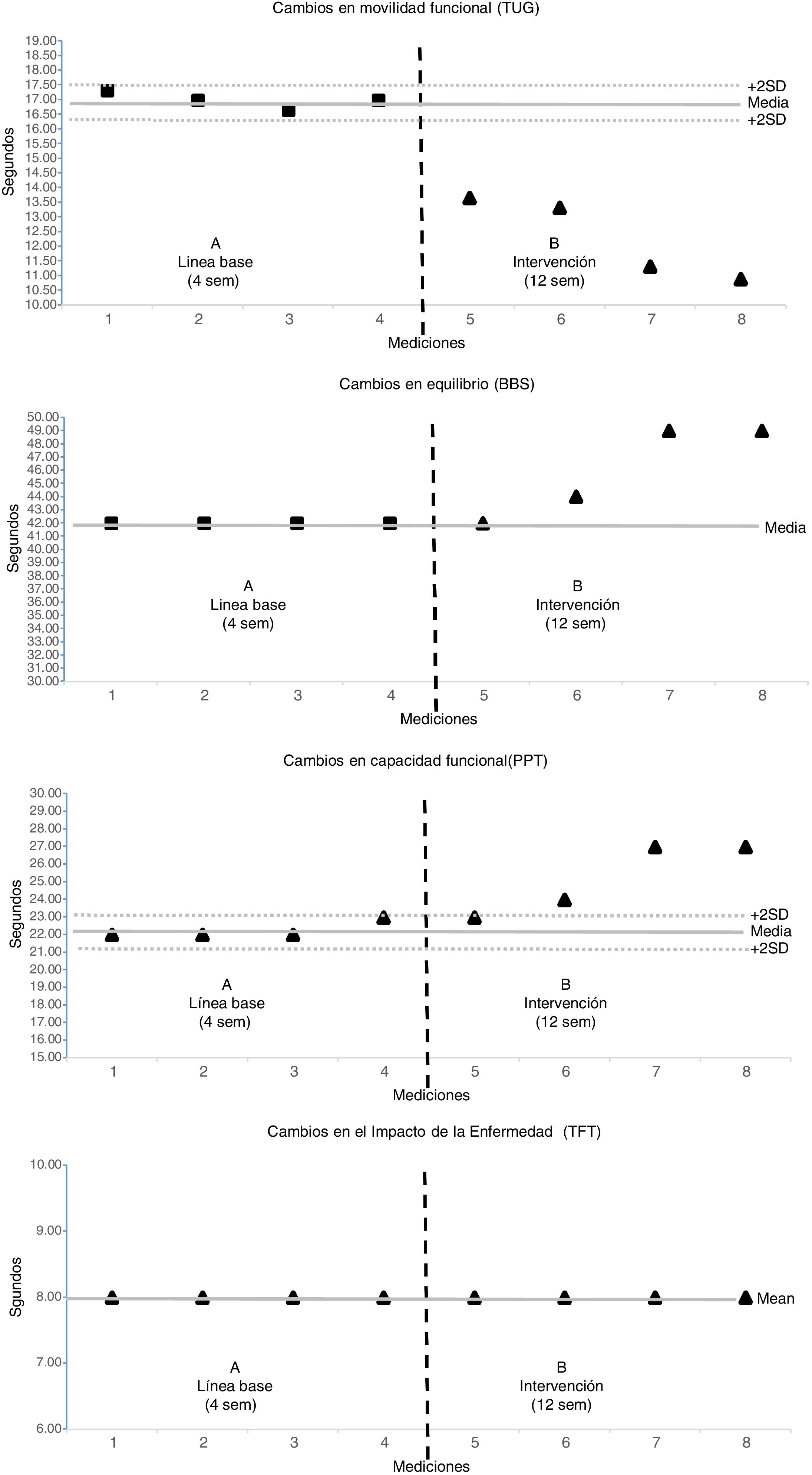
Our patient was a 59-year-old woman who consulted due to gait and balance alterations associated with rapid, involuntary dyskinetic movements. Diagnosis of early-intermediate stage HD was confirmed after a genetic study revealed an abnormal CAG trinucleotide repeat expansion in IT15. Symptomatic treatment was started, and improved motor control. Two months after the diagnosis, and after visiting the Faculty of Education and Sports Sciences at the University of Vigo for information on the types of physical therapy she could receive, the patient agreed to participate in a 12-week Nordic walking programme (3 sessions per week). We conducted a repeated measures single-case study following an A-B design.4 During the A phase, the patient was assessed once per week for 4 weeks. During the B phase, the patient completed the Nordic walking programme, with assessments performed weekly. The School's Ethics Committee approved the study, and the patient gave informed consent to participate. In the first sessions the patient was taught the Nordic walking technique and took 12-minute walks, which were gradually increased to 25minutes’ duration. The Timed Up and Go Test (TUG), Berg Balance Scale (BBS), and Physical Performance Test (PPT) were used to assess the effects of the programme on functional mobility, balance, and physical functioning, respectively.5 To identify possible changes in disease progression, we used the Total Functional Capacity Scale.6 The patient completed all the scheduled sessions (n=36) and presented no adverse effects. The distance covered per session increased from 700 to 1830m, and mean speed increased from 3.9 to 4.5km/h. Assessment results suggested an overall improvement in all variables, with the exception of disease progression (Fig. 1). The total time needed to complete the TUG decreased to 4.6seconds (an improvement of 27.6%). BBS and PPT scores increased by 4 and 3 points, respectively, which represented an improvement of 4% and 3% (Table 1). Our results are consistent with those of other authors reporting the effects of physical exercise on HD. For instance, Mirek et al.7 applied a programme based on balance and gait, and Piira et al.8 developed a multidisciplinary rehabilitation programme; both groups detected significant changes in participants’ TUG and BBS scores. Similarly, Ciancarelli et al.9 report improvements in patients’ functional capacity (PPT scores) after participating in a neurorehabilitation programme. Despite the potential benefits observed after the intervention, we should underscore 2 points. Firstly, the programme had no effect on disease progression. Secondly, only the reduction in the time needed to complete the TUG can be considered a clinically significant change derived from the Nordic walking programme.10 In view of these results, we conclude that Nordic walking represents an effective physical rehabilitation strategy for patients with early-intermediate stage HD. Its practice may lead to clinically relevant changes in functional mobility, as well as some improvements in balance and functional capacity. However, these changes have no impact on disease progression.
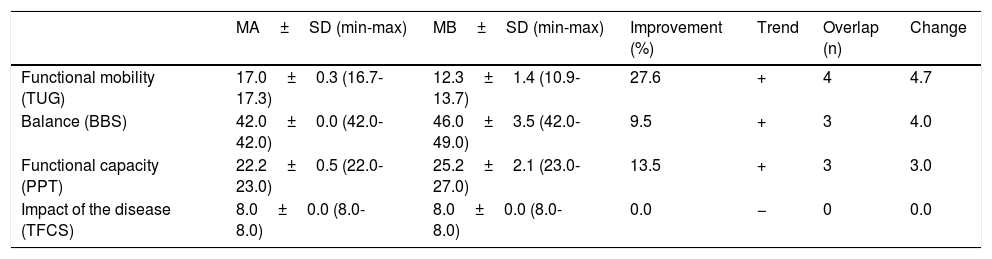
Comparison of functional status and independence before and after the intervention.
| MA±SD (min-max) | MB±SD (min-max) | Improvement (%) | Trend | Overlap (n) | Change | |
|---|---|---|---|---|---|---|
| Functional mobility (TUG) | 17.0±0.3 (16.7-17.3) | 12.3±1.4 (10.9-13.7) | 27.6 | + | 4 | 4.7 |
| Balance (BBS) | 42.0±0.0 (42.0-42.0) | 46.0±3.5 (42.0-49.0) | 9.5 | + | 3 | 4.0 |
| Functional capacity (PPT) | 22.2±0.5 (22.0-23.0) | 25.2±2.1 (23.0-27.0) | 13.5 | + | 3 | 3.0 |
| Impact of the disease (TFCS) | 8.0±0.0 (8.0-8.0) | 8.0±0.0 (8.0-8.0) | 0.0 | − | 0 | 0.0 |
BBS: Balance Berg Scale; MA: mean in phase A; MB: mean in phase B; PPT: Physical Performance Test; SD: standard deviation; TFCS: Total Functional Capacity Scale; TUG: Timed Up and Go Test.
To determine the effect of the intervention, we performed a visual analysis of single-case data during the 2 phases: initial assessment (A) and intervention (B); to do this, we analysed improvement, trend, overlap, and change between phases. Improvement: result of the comparison between means for the A and B phases. Trend: (+) positive differences between A and B phases; (−) no differences between A and B phases. Overlap: total number of assessments during the B phase that met 2 conditions: 1) different from and better than A, 2) the 3 latter measurements suggest improvements. Change: differences between the mean for the A phase and the last assessment (week 12).
Please cite this article as: Martínez-Lemos RI, Domínguez-Pérez C, Seijo-Martínez , Ayán-Pérez C. Mejoría de la capacidad funcional en la enfermedad de Huntington tras un programa de marcha nórdica. A propósito de un caso. 2020. https://doi.org/10.1016/j.nrl.2019.01.006