Cardiac myxoma is the most frequent primary cardiac tumour, accounting for as many as 80% of all cases; it originates in the mesenchymal cells of the endocardium. Neurological involvement accompanies cardiac myxoma in 25% to 45% of all cases and may constitute the initial manifestation. The most frequent presentation is ischaemic stroke due to emboli composed of tumoural tissue or dislodged surface thrombi.1–3 Little scientific evidence is currently available regarding thrombolytic therapy during the acute phase of stroke. We report the case of a woman with acute ischaemic stroke of embolic aetiology associated with a left atrial myxoma treated with intravenous fibrinolytic treatment.
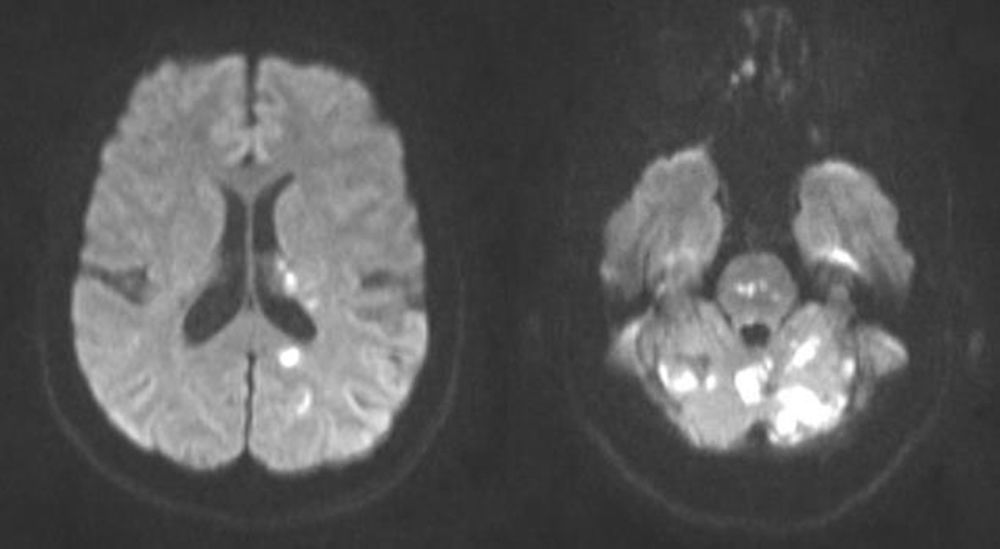
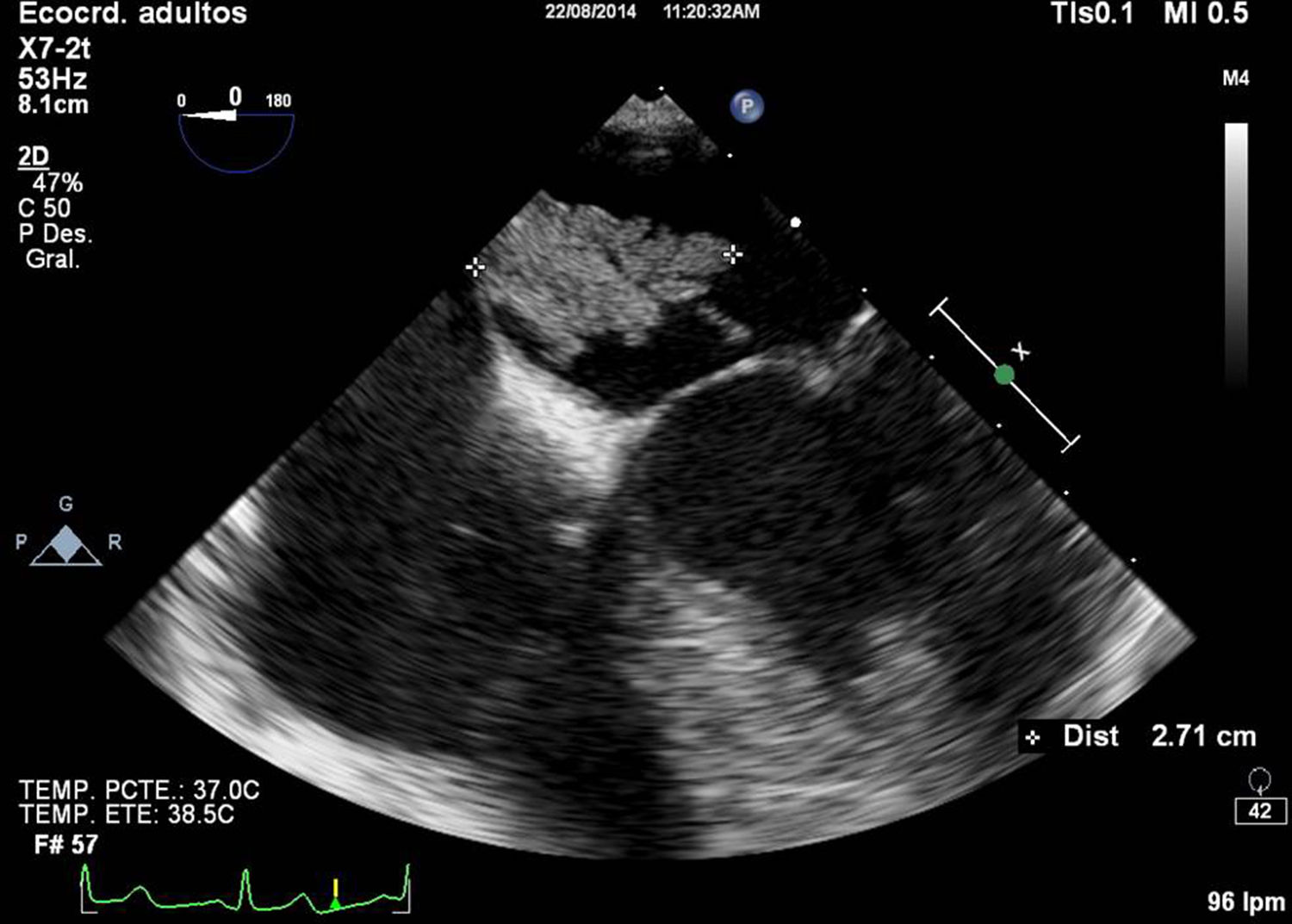
The patient was a smoker of 60 years old with a history of type 2 diabetes mellitus, dyslipidaemia, and chronic obstructive pulmonary disease, who suddenly experienced dizziness, blurred vision, and vomiting. General examination revealed a diastolic murmur at the cardiac apex, which became more intense when the patient was seated. Neurological examination revealed somnolence, moderate dysarthria, right internuclear ophthalmoplegia, left-limb dysmetria, and ataxic gait. A computed tomography (CT) scan showed chronic lacunar ischaemic lesions in both cerebellar hemispheres, with no signs of acute ischaemia; the neurosonological study ruled out large-vessel occlusion. Given the suspicion of acute ischaemic stroke in the vertebrobasilar territory, intravenous fibrinolysis (alteplase 0.9mg/kg) was started 3hours after symptom onset, since no contraindication was present. The patient was admitted to the stroke unit, where she progressed favourably with no systemic or neurological complications; mild dysmetria persisted when performing the left heel-to-knee test, as did gait ataxia. A brain magnetic resonance imaging (MRI) scan performed during hospitalisation revealed multiple acute ischaemic lesions in different cerebral vascular territories (Fig. 1). Radiological suspicion of embolic aetiology led us to request a transoesophageal echocardiogram, which revealed the presence of a left atrial mass compatible with myxoma (Fig. 2). After a risk/benefit analysis, we started treatment with anticoagulants 3 days after admission; this treatment was continued for 15 days, until surgical resection of the left atrial mass was possible. Finally, the anatomical pathology study confirmed the suspicion of cardiac myxoma.
Brain diffusion-weighted MR images showing multiple areas of abnormal diffusion restriction; these are mostly rounded or punctiform, located at the left paraventricular level and the ipsilateral temporal lobe. The remaining areas are located in the vertebrobasilar territory: the pons, left occipital lobe, and especially the vermis and both cerebellar hemispheres.
Treatment in the acute phase of ischaemic stroke secondary to myxoma is subject to debate. Several cases treated with intravenous fibrinolysis,3–10 intra-arterial fibrinolysis,11,12 and mechanical thrombectomy13 have been published. Reports describing thrombolytic treatment include a case of cerebral haemorrhage with mild neurological impairment4 and a case of microbleeding with no relevant clinical signs.14 The effectiveness of the different treatment options is variable; cases in which arterial recanalisation is not achieved may be secondary to tumoural and not thrombotic emboli.13 Our patient's clinical symptoms improved with no signs of haemorrhagic complications.
In conclusion, and despite the scarce evidence available, intravenous fibrinolysis seems to be a safe and effective option for treatment of acute ischaemic stroke secondary to left cardiac myxoma; mechanical extraction of the thrombus is an alternative to consider in the event of large vessel occlusion. In any case, it is difficult to establish specific guidelines for managing these patients since aetiology is typically unknown prior to treatment.
Please cite this article as: Díaz Díaz A, Muñoz García A, Pinar Sedeño G, García Rodríguez JR. Tratamiento fibrinolítico intravenoso en el manejo del ictus isquémico agudo asociado a mixoma auricular izquierdo: a propósito de un caso. Neurología. 2018;33:267–268.