Lemierre syndrome progresses with septic thrombophlebitis of the internal jugular vein with distant septic thromboemboli. It was first described by A. Lemierre nearly a century ago in patients with sepsis due to Fusobacterium necrophorum, mainly associated with pharyngeal infections.1 The literature includes cases with a range of aetiological agents, foci of infection, and thrombus locations.2,3 Brain abscesses caused by anaerobic bacteria generally occur as a result of disruption of anatomical barriers, with bacterial invasion from adjacent or distant tissues. In the case of non-clostridial bacteria, the barriers in question tend to be mucosal membranes, where they are present as saprophytic flora. The single most important factor facilitating the growth of anaerobic bacteria is low oxygen tension, usually secondary to reduced tissue perfusion, although other factors may also influence this process.4
Clinical caseWe describe the case of a 79-year-old man with personal history of arterial hypertension, atrial fibrillation, aortic valve bioprosthesis implantation due to severe aortic insufficiency, and left parotid carcinoma treated with surgery and adjuvant radiotherapy at 68 years of age.
He presented left otalgia of 5 days’ progression, associated with fever, nausea, and general discomfort. Outpatient treatment with amoxicillin and clavulanic acid was prescribed due to suspicion of acute otitis media. He was subsequently referred to the emergency department due to subacute onset of left hemiparesis and persistence of fever.
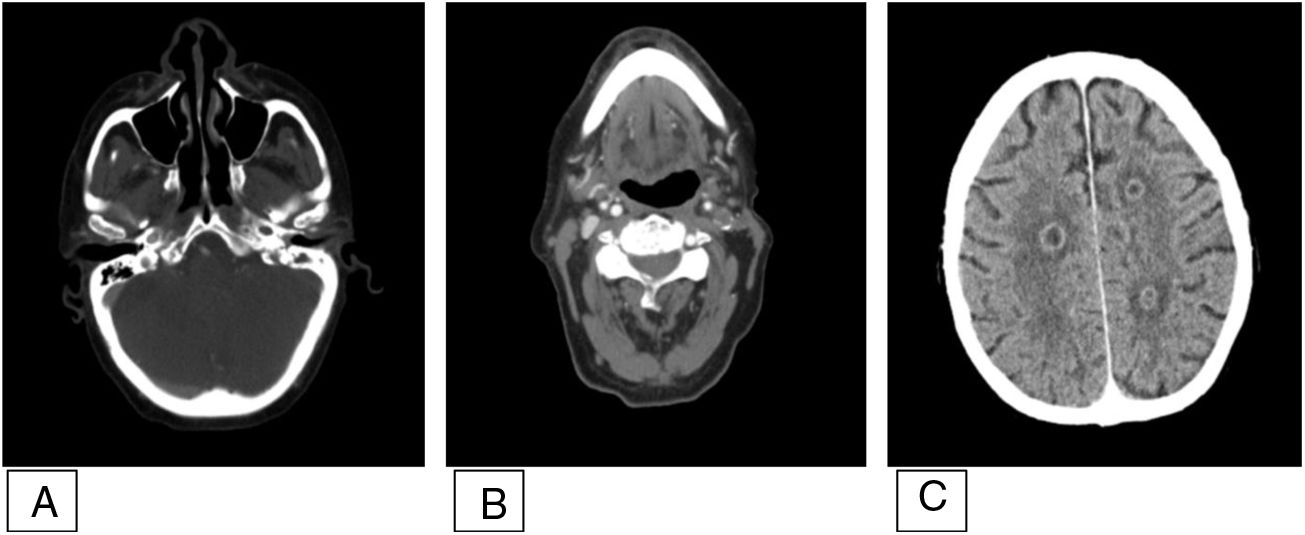
Laboratory tests showed leukocytosis (17 500 × 103 cells/μL; 94% neutrophils), C-reactive protein level of 176 mg/L (reference range, 0-5), and procalcitonin level of 1.1 ng/mL (reference range, 0-0.5). Emergency head and neck CT revealed signs of acute left otomastoiditis with destruction of the osseous septa, enlargement of pre- and retrostyloid soft tissue, and destruction of the bone of the occipital condyle and inferomedial region of the petrous bone. Contrast-enhanced imaging revealed lack of flow in the left jugular vein and in the internal carotid artery (ICA) after its bifurcation. Several intraparenchymal ring-enhancing lesions were observed in the left temporal lobe, right frontal lobe, periventricular regions, and right centrum semiovale (Fig. 1).
Contrast-enhanced head and neck CT study. A) Occupation of the left middle ear, compatible with otitis without pneumatisation of the ipsilateral mastoid cells. B) Occlusion of the left internal carotid artery and internal jugular vein. C) Hypodensities with ring enhancement in various territories, compatible with abscesses.
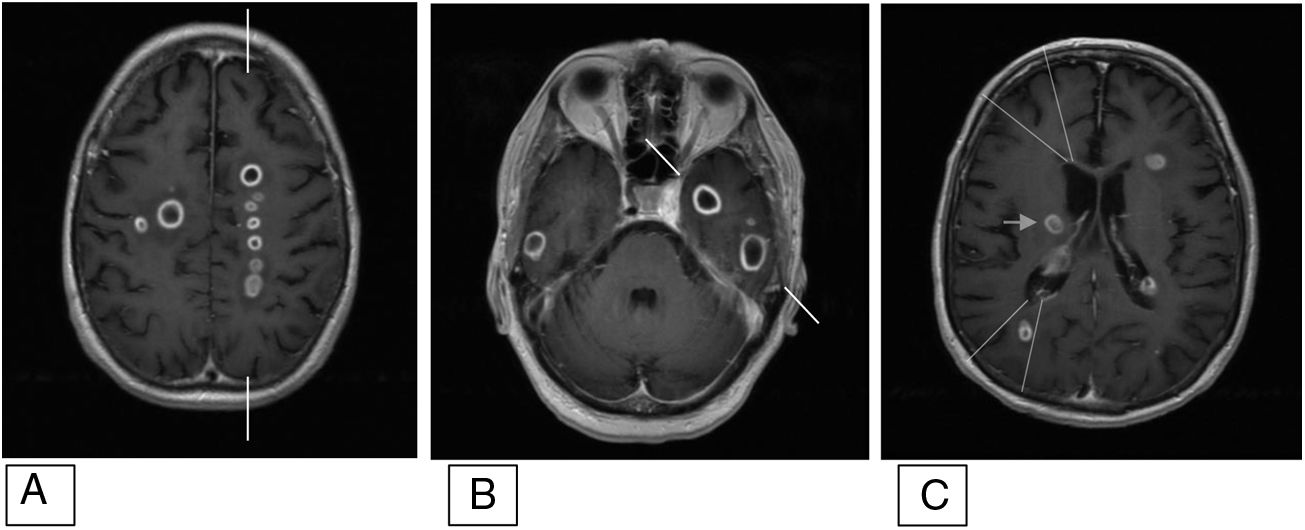
Brain MRI confirmed the diagnosis of left otomastoiditis and revealed thrombi in the left transverse and sigmoid sinuses and jugular vein, as well as occlusion of the cavernous segment of the left ICA with recanalisation due to collateral flow from the circle of Willis. The brain parenchyma displayed multiple round lesions with central T1 hypointensity and T2 hyperintensity, diffusion restriction, and thin ring enhancement after contrast administration; these findings are compatible with brain abscesses with predominant distribution in vascular watershed territories (Fig. 2).
Brain MRI. Contrast-enhanced T1-weighted volumetric sequences conducted for neuronavigation. Axial plane. Abscesses are distributed in watershed territories. A) Between the left MCA (lateral to marks) and the left ACA (medial to marks). B) Between the left MCA (rostral to marks) and the left PCA (caudal to marks). C) Anterior and posterior watershed territories (lines) and in the area of the perforating branches of the right MCA (arrow). Images based on the vascular territories described by Tatu et al.9 and watershed territories described by Caplan.10
ACA: anterior cerebral artery; MCA: middle cerebral artery; PCA: posterior cerebral artery.
No pathogen was isolated in the ear drainage culture. Blood cultures were positive for Fusobacterium nucleatum. We completed the study with a thoracic, abdominal, and pelvic CT scan and transoesophageal echocardiography study, which did not identify any other possible foci of infection.
The patient received antibiotics for a total of 38 days, initially with linezolid and piperacillin/tazobactam, which was subsequently switched to vancomycin, ceftriaxone, and metronidazole due to blood toxicity; this treatment was supplemented for 8 weeks with moxifloxacin and clindamycin. At 3 months of follow-up, the brain MRI lesions had resolved and the patient presented residual mild left hemiparesis.
DiscussionWe present a case of multiple brain abscesses distributed in watershed regions in a patient with acute left otomastoiditis and thrombi in cerebral venous sinuses and the left internal carotid artery, meeting the criteria for Lemierre syndrome.5
F. nucleatum is an anaerobic bacterium most frequently involved in infections of odontogenic and pulmonary origin.6,7 Our patient presented with otitis and mastoiditis. This bacterium has previously been reported as the causal agent in Lemierre syndrome.2 Although otitis and mastoiditis have previously been associated with single brain abscesses in contiguous areas, the distribution of abscesses in our patient suggests haematogenous spread. Other possible primary foci of infection were ruled out.
Complete occlusion of the left ICA caused hypoperfusion of that vessel’s territory of uncertain time of onset, requiring compensation by collateral circulation from the circle of Willis. This hypoperfusion, which mainly affects watershed territories8,9 and was somewhat more marked in the left hemisphere in our patient, increases vulnerability to insults in which oxygen tension in the tissue plays an important role, as is the case with anaerobic bacteria.
ConclusionThe interest of this case lies in the unusual aetiological agent for middle ear infection, the haematogenous spread of the infection, and the asymmetrical distribution of abscesses in watershed territories mainly in the left hemisphere, facilitated by hypoperfusion of the brain tissue due to the occlusion of the left ICA.
Conflicts of interestThe authors have no conflicts of interest to declare. This study has received no funding of any kind.
Please cite this article as: Gámez-Beltrán P, Vázquez-Sánchez F, López-Veloso M, Casas-Peña E. Síndrome de Lemierre con abscesos cerebrales distribuidos en territorios frontera vasculares. Caso clínico. Neurología. 2022;37:154–156.