We present the case of a 79-year-old man with personal history of arterial hypertension and well-controlled diabetes mellitus. The patient was independent in basic and complex activities of daily living. He attended an outpatient consultation due to a 6-month history of cognitive impairment, as well as gait impairment in the last 2 months. As an associated factor, he reported mild head trauma due to a fall at home, without loss of consciousness or other symptoms. Neurological examination revealed normal speech, disorientation in time (2/5 on the Mini–Mental State Examination [MMSE] subtest), and good spatial orientation (5/5 on the MMSE subtest). Attention was normal (6/5 on the Digit Span test), and the patient presented verbal episodic memory alteration (4/8 on the Memory Impairment Screen). Visuospatial skills were also affected, with clear constructive apraxia (3/10 on the command condition of the clock-drawing test). The rest of the neurological examination revealed unstable, apraxic gait with short strides, preventing the patient from walking without a cane or support.
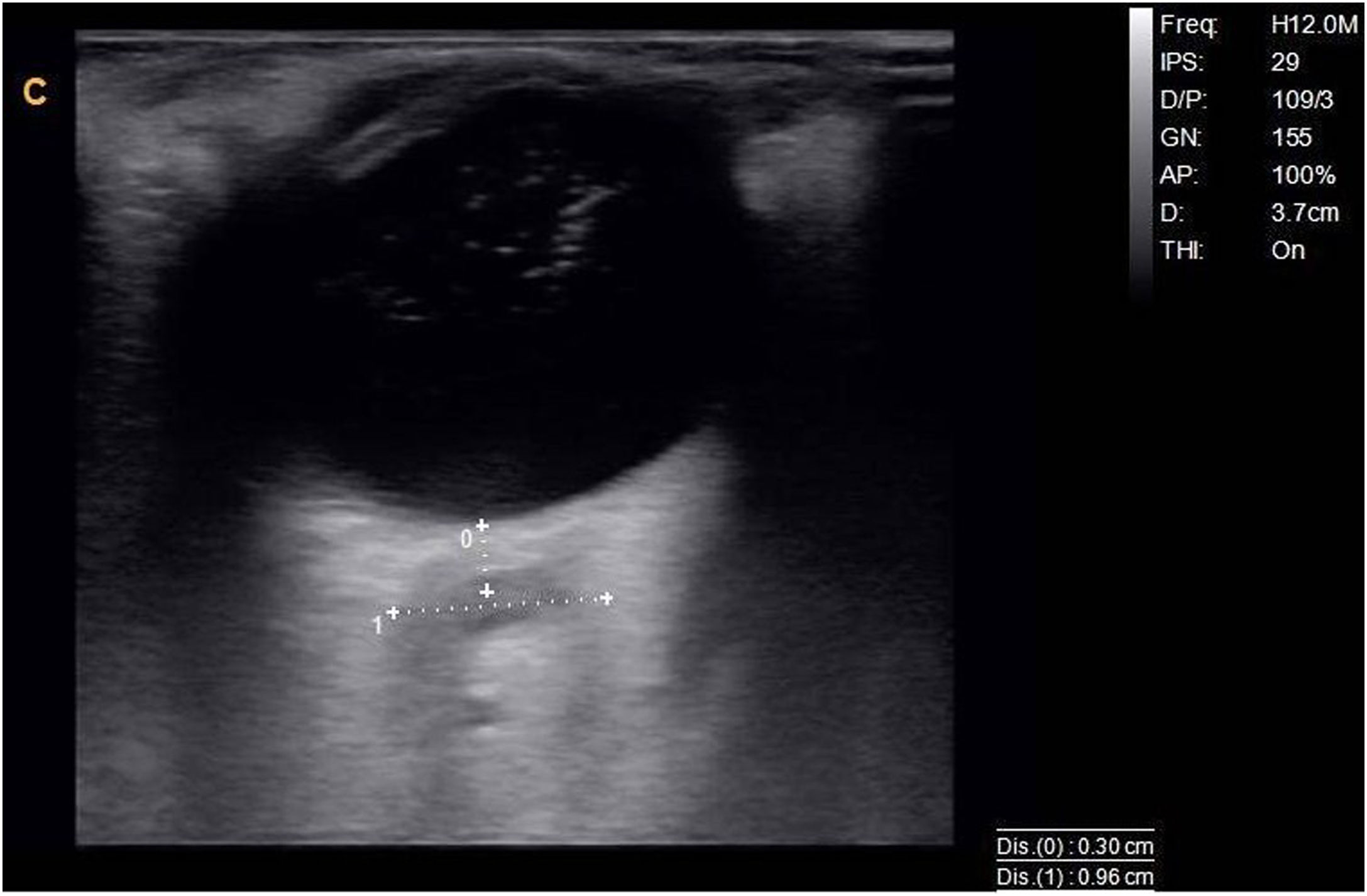
A portable ultrasound system (Chison Q9 with a 7 MHz linear probe) was used to perform a B-mode orbital ultrasound study; optic nerve diameter was 9.6 mm on the right side (Fig. 1) and 6.4 mm on the left.
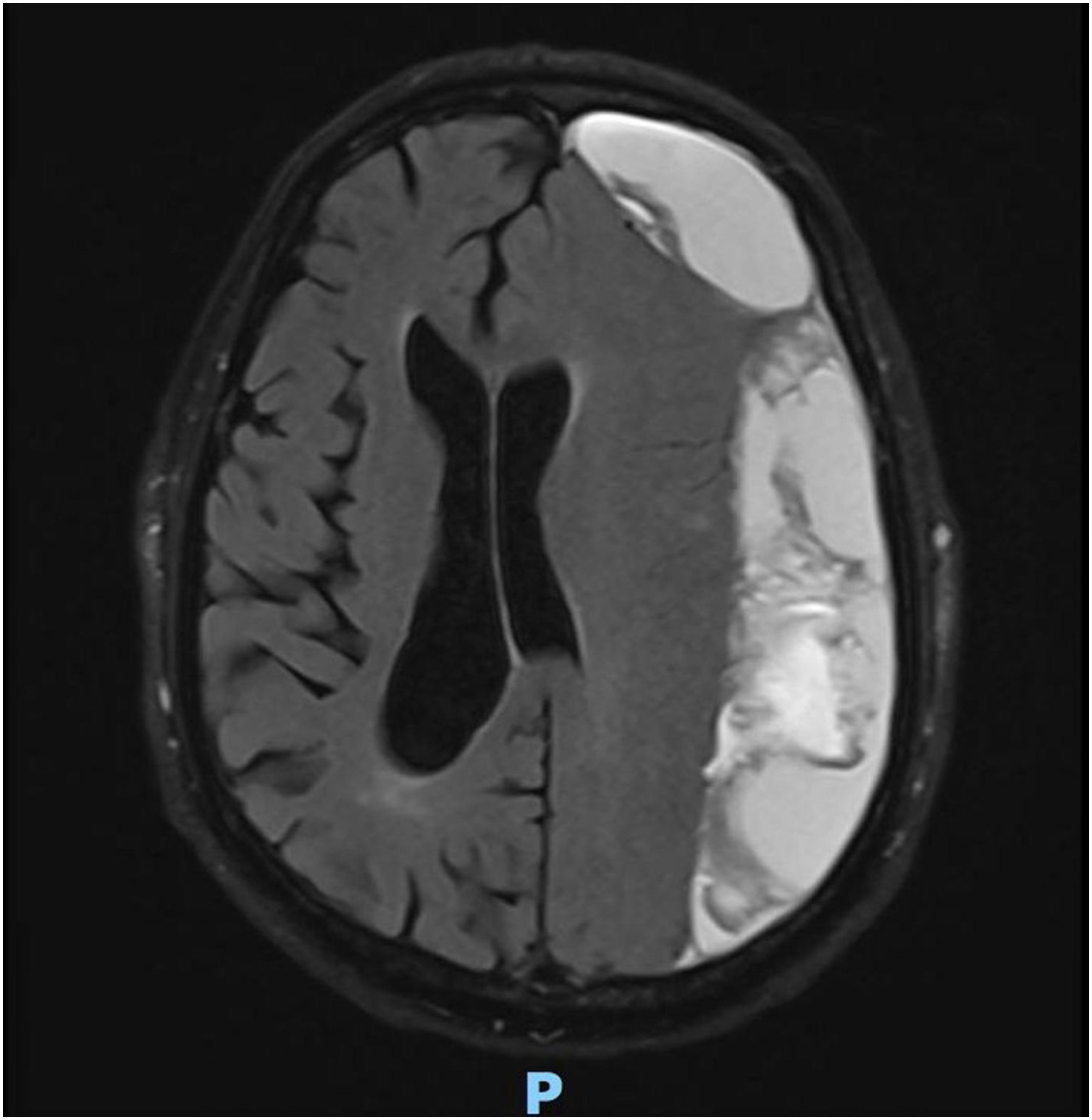
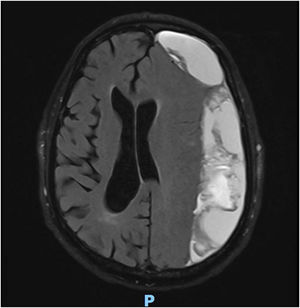
Given the diagnostic suspicion of rapidly progressive dementia with gait alterations, and the ultrasound findings suggesting intracranial hypertension, we requested an emergency brain MRI study (Fig. 2).
The study detected extensive subdural haematoma and intracranial hypertension, and the patient was referred to the neurosurgery department, where he underwent emergency craniectomy and haematoma evacuation. At 48 hours, the patient’s cognitive status had improved, with recovery of verbal episodic memory (7/8 on the Memory Impairment Screen) and orientation in time (4/5 on the MMSE subtest). Gait had improved, particularly in terms of stability, and the patient was able to walk short distances (10 m) unaided.
Optic nerve sheath diameter has been shown to be a useful non-invasive marker of intracranial hypertension; most studies have mainly focused on patients with idiopathic intracranial hypertension, which was subsequently confirmed with lumbar puncture.1 This technique is simple to perform and requires minimal training and theoretical knowledge of ultrasound. It requires an ultrasound system capable of delivering B-mode ultrasound, and a 3-9 MHz multifrequency linear probe. The eye is studied via the transorbital window. The patient is placed in a supine position with the head elevated by 20°-30°. With the patient’s eyes closed, gel is applied to the upper eyelid. The probe is applied with an axial orientation to visualise the optic disc and the retrobulbar region of the optic nerve; at a depth of approximately 3 mm beyond this location, following the trajectory of the optic nerve, the measurement is taken from the external edges of the hyperechogenic rim of the optic nerve, which corresponds to the optic nerve sheath (Fig. 1). The studies evaluated show adequate inter-rater reliability; the normal range has been established at 5.4 ± 0.6 mm.1–3
Among the current indications, besides idiopathic intracranial hypertension, other studies have provided information on intracranial pressure in the neurocritical care of patients in a coma due to head trauma or intracranial haemorrhage, reporting sensitivity of 90% and specificity of 85%.4
The advantages of the technique are obvious: it is non-invasive, reproducible, economical, and quick and simple to perform by staff with the appropriate training. Its disadvantages include the fact that 10% of patients with intracranial hypertension do not present these changes in the optic nerve, probably due to individual anatomical variability. It is also unable to detect cases of intracranial hypertension with acute progression. This should be considered a complementary technique, and the results must be confirmed with definitive diagnostic studies, such as neuroimaging or CSF pressure testing, in cases of strong diagnostic suspicion.5
This case demonstrates how orbital ultrasound may be useful in clinical practice in patients with rapidly progressive dementia and history of trauma. Proper training and experience, as well as the availability of an ultrasound system at the consultation, were essential in performing the study. Used by experienced professionals, it can be highly effective for diagnosing suspected intracranial hypertension and for indicating more efficient diagnostic or therapeutic measures in various areas of neurology.
This ultrasound technique may provide highly valuable information in the initial assessment of the following conditions: a) headache with signs or symptoms of intracranial hypertension; b) headache associated with obesity; c) differential diagnosis of bilateral papilloedema/pseudopapilloedema; d) non-invasive monitoring of intracranial pressure in critical patients with extensive stroke, meningitis, or trauma; and e) rapidly progressive dementia associated with focal neurological signs or history of falls or trauma, as in the case of our patient. Scientific data are currently limited, and further clinical research may be beneficial.
Please cite this article as: Delgado López F. Medición del diámetro del nervio óptico por ecografía modo B como signo indirecto de hipertensión endocraneal. Neurología. 2021;36:733–734.