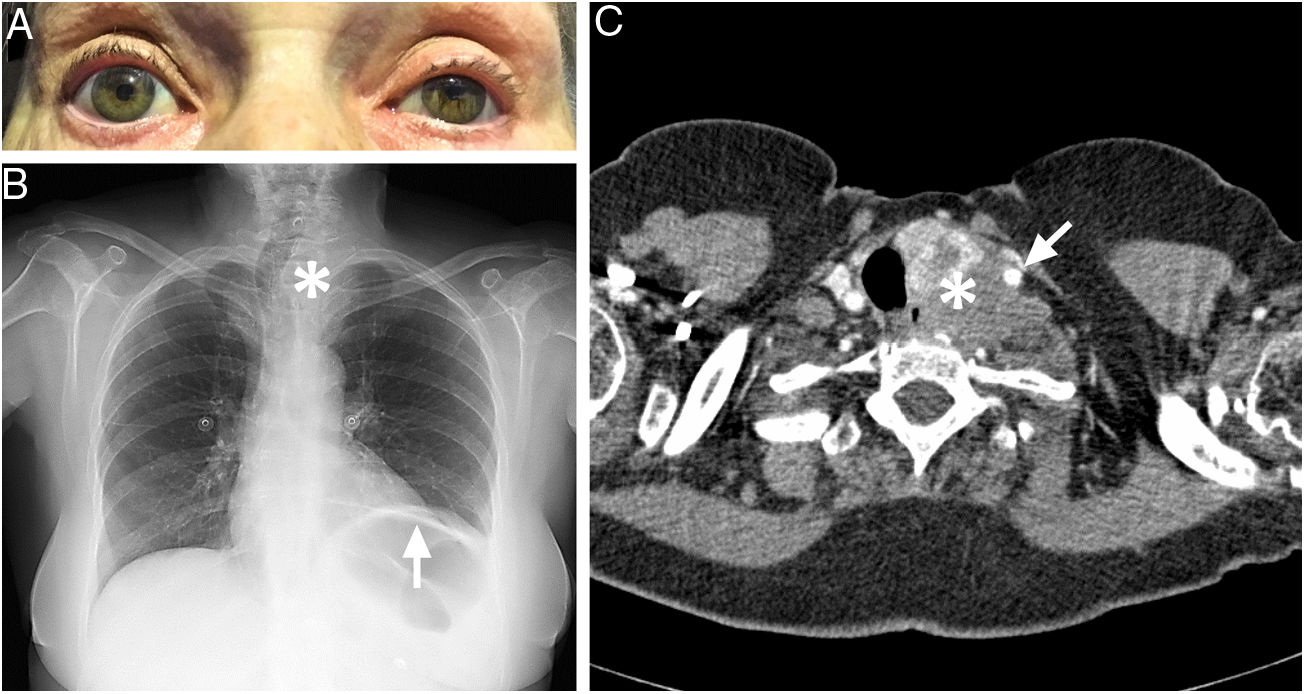
We present the case of a 71-year-old woman with history of arterial hypertension and type 2 diabetes mellitus who visited the emergency department due to left-sided ptosis of 2 weeks’ progression. She also reported constant dull pain in the left shoulder, located on the belly of the trapezius muscle, which was not altered with postural changes or Valsalva manoeuvres. The patient reported no other focal neurological signs or other symptoms. Three weeks earlier, she had undergone laparoscopic cholecystectomy and was discharged with no neurological symptoms. The neurological examination revealed narrowing of the left palpebral fissure and anisocoria with relative miosis in the left eye, observable only in semi-darkness; these findings are compatible with Horner syndrome (Fig. 1A). Examination of the cranial nerves, motor system, sensitivity, reflexes, coordination, and balance revealed no other alterations.
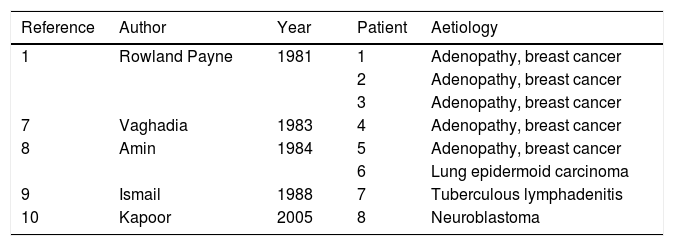
(A) Left ptosis and miosis in semi-darkness. (B) Anteroposterior chest radiography showing elevation of the left hemidiaphragm (arrow) and right-sided tracheal deviation in the superior mediastinum (asterisk). (C) Neck CT scan (axial plane) with intravenous contrast, revealing a mass originating from the left thyroid lobule (asterisk), with irregular density and involving the left common carotid artery (arrow).
Upon arrival at the hospital, a blood analysis ruled out relevant alterations in the blood count, coagulation, biochemical parameters, and C-reactive protein. A non-contrast head CT scan revealed normal results. A chest radiography showed a loss of volume of the left lung secondary to elevation of the ipsilateral hemidiaphragm (absent in the preanaesthetic assessment conducted 2 months earlier) and right-sided tracheal deviation in the superior mediastinum (Fig. 1B).
The combination of Horner syndrome, left phrenic nerve palsy, and tracheal deviation led us to suspect a cervical lesion in the left superior mediastinum. Neck CT scans performed before and after contrast administration confirmed the presence of a left paratracheal mass arising from the thyroid gland, showing irregular contrast uptake, partially involving the ipsilateral common carotid artery (Fig. 1C). An MRI study of the cervical spine revealed that the mass, located in the left prevertebral region between C6 and C7, did not infiltrate the vertebral bodies or intervertebral foramina. The anatomical pathology study of samples obtained by fine needle aspiration biopsy and subsequent core needle biopsy was not sufficient for diagnosis; therefore, we opted to perform open surgery for diagnostic and therapeutic purposes. The procedure revealed a left anterior cervical mass with poorly-defined edges, infiltrating the surrounding tissues; the mass was partially resected. The anatomical pathology diagnosis was anaplastic thyroid carcinoma. Treatment was started with radiotherapy, despite which we observed rapid progression of local pain and thrombosis of the left internal jugular vein. The patient was enrolled in a palliative care programme and was lost to follow-up 5 months after symptom onset.
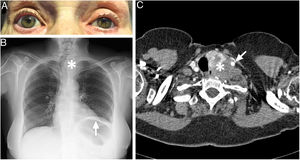
The ipsilateral presence of Horner syndrome, shoulder pain, phrenic nerve palsy, and vocal cord paralysis (absent in our patient at the time of diagnosis) was described by Rowland Payne1–3 as a manifestation of expansive lesions in the anterior and inferior region of the neck or in the thoracic inlet. These alterations have been described as complications of interscalene nerve blocks.4–6 Rowland Payne syndrome in the absence of this kind of anaesthetic block has been reported almost exclusively in association with malignant tumours, as in the case of our patient (Table 1).1,7–10 The lesion causing the syndrome is usually located at the level of the sixth cervical vertebra, although it may also be caused by expansive lesions with greater volume and more caudally located (in the thoracic inlet).1–3,7 This anatomical location is the only one where the cervical sympathetic plexus, the phrenic nerve, and the recurrent laryngeal nerve run in close proximity.
Cases of Rowland Payne syndrome reported in the literature.
| Reference | Author | Year | Patient | Aetiology |
|---|---|---|---|---|
| 1 | Rowland Payne | 1981 | 1 | Adenopathy, breast cancer |
| 2 | Adenopathy, breast cancer | |||
| 3 | Adenopathy, breast cancer | |||
| 7 | Vaghadia | 1983 | 4 | Adenopathy, breast cancer |
| 8 | Amin | 1984 | 5 | Adenopathy, breast cancer |
| 6 | Lung epidermoid carcinoma | |||
| 9 | Ismail | 1988 | 7 | Tuberculous lymphadenitis |
| 10 | Kapoor | 2005 | 8 | Neuroblastoma |
It is therefore important to be aware of and to recognise this rare syndrome, given its anatomical and clinical correlation and its strong association with neoplastic lesions.
FundingThis study has received no specific funding from any public, commercial, or non-profit organisation.
Please cite this article as: Sierra-Hidalgo F, Aragón Revilla E. Síndrome de Rowland Payne. Neurología. 2021;36:734–736.