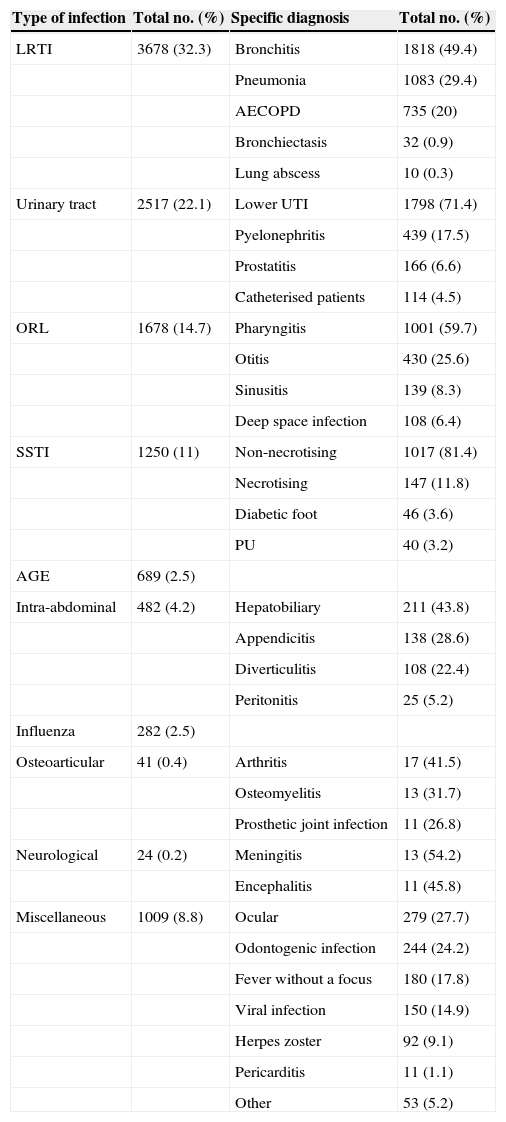
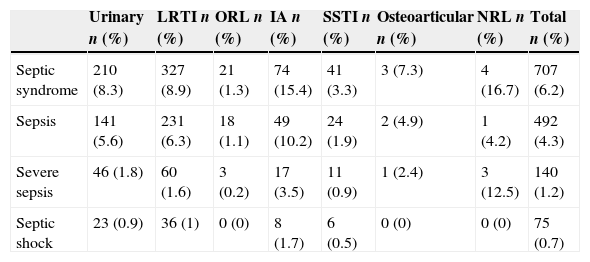
Infectious diseases of the central nervous system (CNS) are responsible for a sizeable portion of the morbidity and mortality associated with infectious disease in general. Hospital emergency departments (ED) usually serve as the first and fundamental link in the chain of care for severe infectious diseases, including neurological diseases that may require consultations with neurologists.1–3 Most studies published in Spain during the past three decades have shown that infectious diseases account for 5% to 17% of all hospital emergencies, and that they also constitute one of the main causes of hospitalisation and mortality.4–7 We completed a descriptive multi-centre study with a cross-sectional analysis of 49 EDs distributed all across Spain. The sampling procedure was to include all patients clinically diagnosed with an infectious disease in the ED between midnight and noon on the 10th day of every month, and between noon and midnight on the 20th day of every month, during the 12 consecutive months between October 2010 and September 2011. The sample excluded patients attended by the obstetrics and gynaecology department and children younger than 14. We recorded demographic variables, comorbidities, type of infection diagnosed, and presence or absence of clinical markers of sepsis.8,9 During the study period, doctors attended a total of 79654 patients in participating Spanish EDs and diagnosed 11399 cases of clinical infectious diseases (14.3%). A breakdown of the different disease types (Table 1) yielded 24 patients with infectious diseases of the CNS (0.2% of the total infections). Mean age (SD) of patients diagnosed with infection was 53.2 (23) years; 51.2% were women. The mean age for CNS infections only was 49.7 years. Analysis of the infections by the severity of clinical symptoms found that 707 patients (6.2%) presented clinical indicators of sepsis when they were examined; within this group, 140 patients (1.2%) presented indicators of severe sepsis, and 75 (0.7%) were in septic shock (Table 2). Of all types of infections, neurological infections were the most commonly associated with sepsis (16.7% vs 7.4% overall; P=.009). Of the 24 patients diagnosed with a neurological condition, 4 were considered to be in critical condition because they displayed sepsis or septic shock (sepsis in 1 case, septic shock in 3 cases). Only 1 patient died out of the 24 recorded cases of CNS infections in the ED. The breakdown of the 24 patients by diagnosis listed 13 cases of pure meningitis without encephalitis (45.8%) and 11 cases of meningoencephalitis (54.2%). There were 14 men (58.3%) and 10 women (43.7%).
Characteristics of infections.
| Type of infection | Total no. (%) | Specific diagnosis | Total no. (%) |
|---|---|---|---|
| LRTI | 3678 (32.3) | Bronchitis | 1818 (49.4) |
| Pneumonia | 1083 (29.4) | ||
| AECOPD | 735 (20) | ||
| Bronchiectasis | 32 (0.9) | ||
| Lung abscess | 10 (0.3) | ||
| Urinary tract | 2517 (22.1) | Lower UTI | 1798 (71.4) |
| Pyelonephritis | 439 (17.5) | ||
| Prostatitis | 166 (6.6) | ||
| Catheterised patients | 114 (4.5) | ||
| ORL | 1678 (14.7) | Pharyngitis | 1001 (59.7) |
| Otitis | 430 (25.6) | ||
| Sinusitis | 139 (8.3) | ||
| Deep space infection | 108 (6.4) | ||
| SSTI | 1250 (11) | Non-necrotising | 1017 (81.4) |
| Necrotising | 147 (11.8) | ||
| Diabetic foot | 46 (3.6) | ||
| PU | 40 (3.2) | ||
| AGE | 689 (2.5) | ||
| Intra-abdominal | 482 (4.2) | Hepatobiliary | 211 (43.8) |
| Appendicitis | 138 (28.6) | ||
| Diverticulitis | 108 (22.4) | ||
| Peritonitis | 25 (5.2) | ||
| Influenza | 282 (2.5) | ||
| Osteoarticular | 41 (0.4) | Arthritis | 17 (41.5) |
| Osteomyelitis | 13 (31.7) | ||
| Prosthetic joint infection | 11 (26.8) | ||
| Neurological | 24 (0.2) | Meningitis | 13 (54.2) |
| Encephalitis | 11 (45.8) | ||
| Miscellaneous | 1009 (8.8) | Ocular | 279 (27.7) |
| Odontogenic infection | 244 (24.2) | ||
| Fever without a focus | 180 (17.8) | ||
| Viral infection | 150 (14.9) | ||
| Herpes zoster | 92 (9.1) | ||
| Pericarditis | 11 (1.1) | ||
| Other | 53 (5.2) |
AECOPD: acute exacerbation of chronic obstructive pulmonary disease; AGE: acute gastroenteritis; SSTI: skin and soft tissue infection; LRTI: lower respiratory tract infection; ORL: otorhinolaryngological infection; PU: pressure ulcers.
Type of infection and criteria for sepsis.
| Urinary n (%) | LRTI n (%) | ORL n (%) | IA n (%) | SSTI n (%) | Osteoarticular n (%) | NRL n (%) | Total n (%) | |
|---|---|---|---|---|---|---|---|---|
| Septic syndrome | 210 (8.3) | 327 (8.9) | 21 (1.3) | 74 (15.4) | 41 (3.3) | 3 (7.3) | 4 (16.7) | 707 (6.2) |
| Sepsis | 141 (5.6) | 231 (6.3) | 18 (1.1) | 49 (10.2) | 24 (1.9) | 2 (4.9) | 1 (4.2) | 492 (4.3) |
| Severe sepsis | 46 (1.8) | 60 (1.6) | 3 (0.2) | 17 (3.5) | 11 (0.9) | 1 (2.4) | 3 (12.5) | 140 (1.2) |
| Septic shock | 23 (0.9) | 36 (1) | 0 (0) | 8 (1.7) | 6 (0.5) | 0 (0) | 0 (0) | 75 (0.7) |
IA: intra-abdominal; SSTI: skin and soft tissue infection; LRTI: lower respiratory tract infection; NRL: neurological infection; ORL: otorhinolaryngological infection.
Infectious diseases of the CNS are associated with a higher severity index than the mean index for infections in general (16.7% vs 7.4%; P=.009), with a higher probability of sepsis and other systemic infectious complications. During the data gathering phase, we recorded the diagnosis pronounced and reported by the doctor who attended the patient. We assume margins of error for both pathogenesis and pathochronia and also recognise that some cases seen in the ED are not diagnosed as infections by that department, but rather at a later point as doctors continue to monitor the patient's clinical course.
Gathering a multicentre sample from hospitals all across Spain according to such strict time frames also places certain limits on diagnostic criteria. While the percentage of CNS infections treated in the ED may be considered relatively low, these infections were very severe according to the data collected in this study. EDs and consulting neurologists should employ the maximum diagnostic caution with these infections, which have a high risk of associated septic and systemic complications.
Please cite this article as: González Martínez F, Huete Hurtado A, Mercedes Kerlin L, Zamora Peña RE. Estudio prospectivo y multicéntrico de la epidemiología de las infecciones del sistema nervioso central (meningitis y encefalitis) en los servicios de urgencias hospitalarios: análisis de subgrupo del estudio INFURG-SEMES. Neurología. 2015;30:381–383.
Part of this study was presented as an oral communication in the 2013 SEN Annual Meeting in Barcelona.