Optic nerve drusen (OND) are globular hyaline bodies measuring 5 to 1000μm in diameter and located anterior to the lamina cribrosa. They contain amino acids, nucleic acids, iron, and calcium, and have a clinical incidence of 3.4 per 1000 adults; histological autopsy studies reflect higher incidence.1 Pathogenesis is not well understood, but the most widely accepted theories suggest an alteration in the axoplasmic transport of ganglion cells. They tend to be bilateral, asymmetrical, and more common in females; drusen formation is a dynamic process that generally begins in the second decade of life. Most cases are idiopathic in origin, although some show autosomal dominant transmission. Drusen are associated with such ocular vascular anomalies as cilioretinal arteries, pronounced vessel tortuosity, abnormal bifurcations, collateral retinochoroidal vessels, peripapillary neovascularisation, and occlusive vascular diseases.2
One type of OND is known as hidden or deep, with elevated papillae and poorly-defined edges; ultrasound images of this type do not reveal a nodular appearance. Visible or superficial OND, in turn, appear as yellowish nodules of different numbers and sizes within a papilla that is typically elevated and displays poorly-defined edges.3
We present a clinical case of OND with severe visual field alterations and marked atrophy of the retinal nerve fibre layer (RNFL).
Our patient was a 40-year-old man referred by the neuro-ophthalmology unit for an evaluation of pseudopapilloedema. The patient was asymptomatic and had no relevant personal or family history.
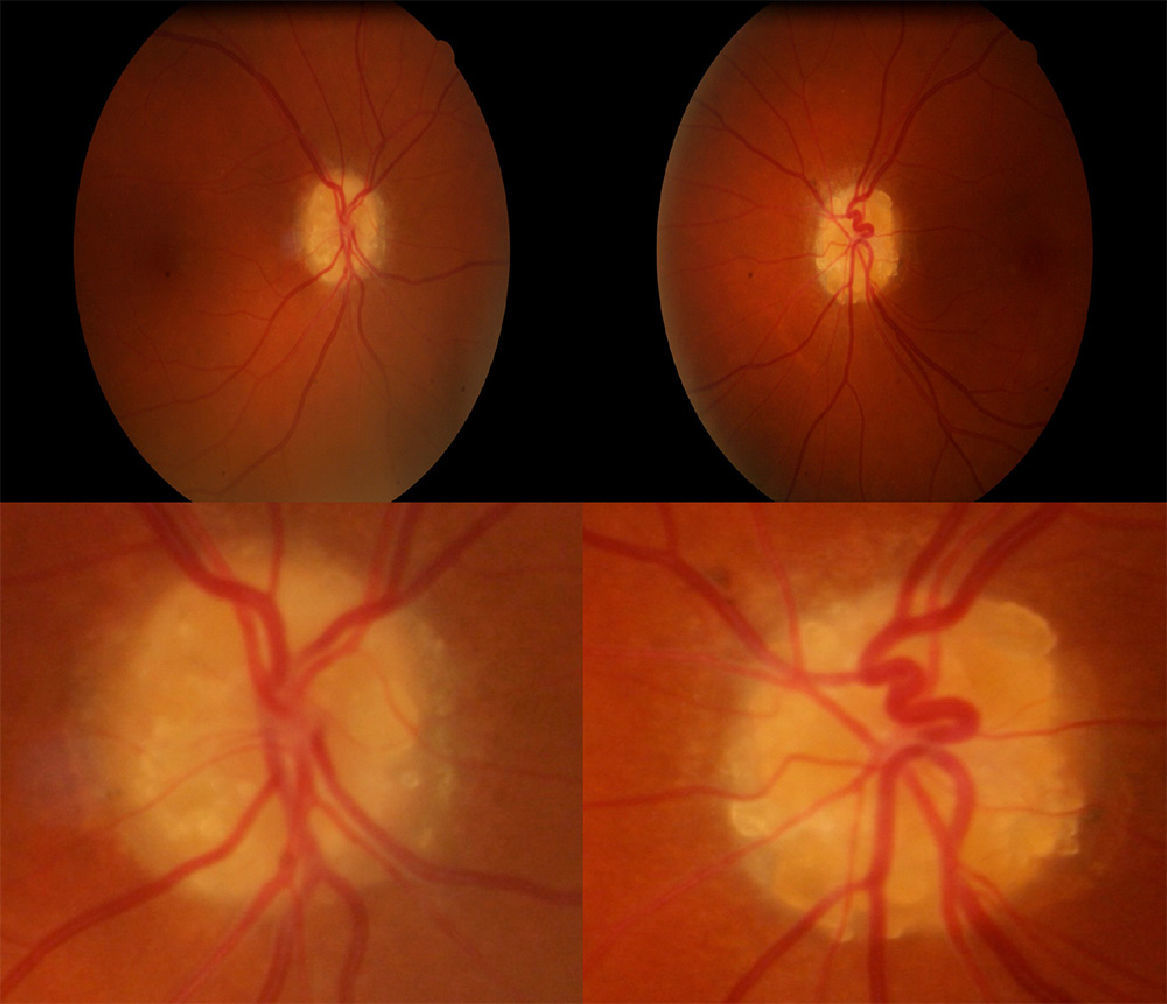
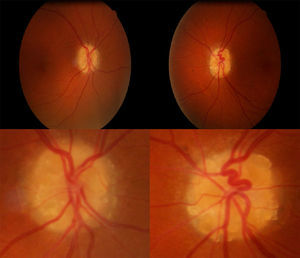
Visual acuity was 0.60 in both eyes (OU); intraocular pressure (IOP) was 14mmHg in OU. Biomicroscopy results were normal, and the fundus displayed elevated and asymmetrical papillae with round, yellowish deposits (Fig. 1).
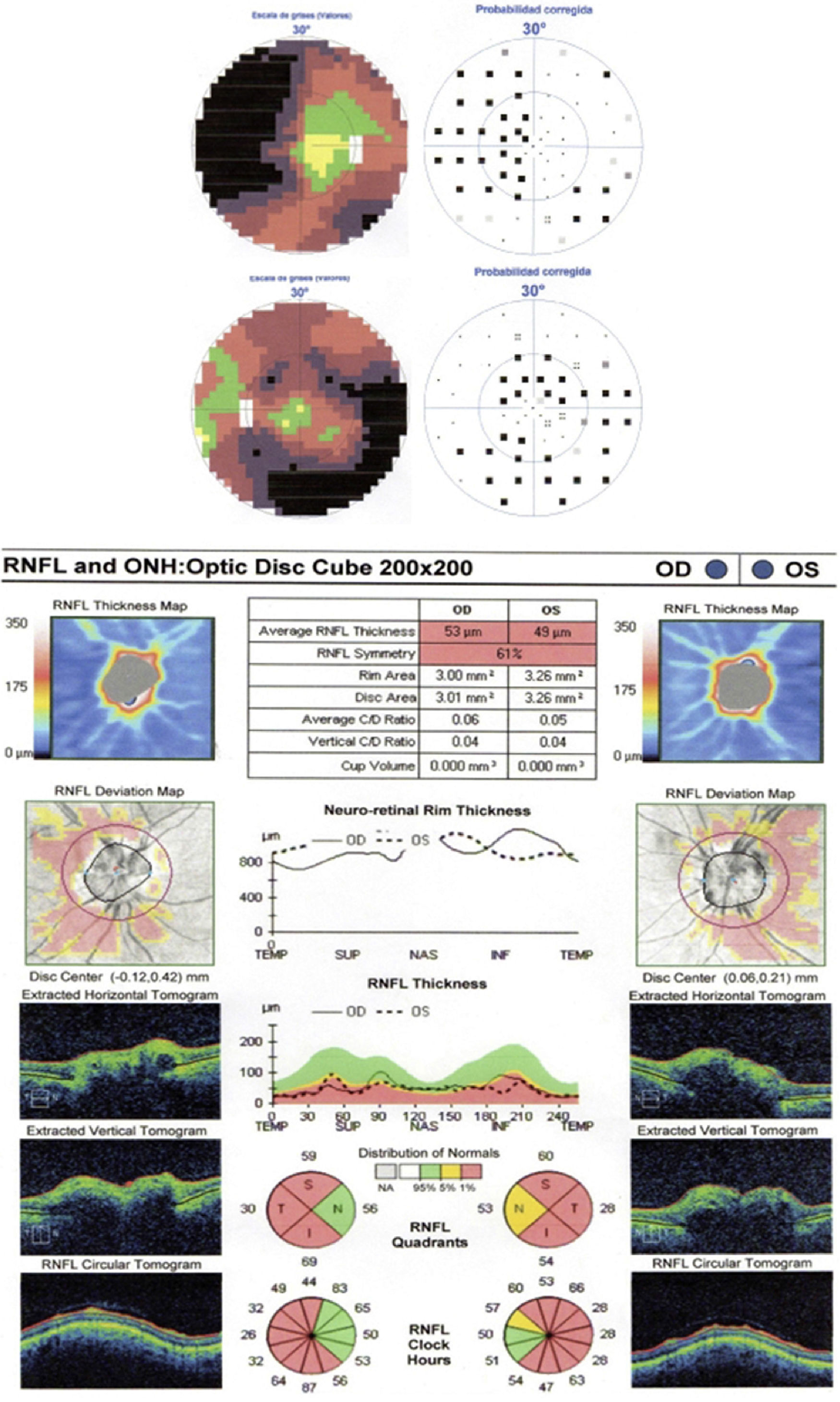
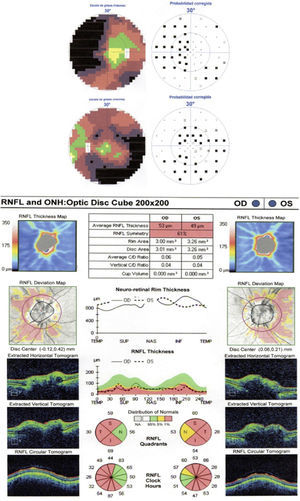
Visual field analysis, performed using Octopus 1-2-3® and the G1X program, detected a bilateral nasal arcuate defect (Fig. 2A). Optic nerve tomography (ONT) showed a decrease in the nerve fibre layer in the temporal, superior, and inferior regions of OU (Fig. 2B).
OND may result in loss of central visual acuity, although this is infrequent. They can also cause severe visual field deficits, some of which may mimic those seen in glaucoma.4 These deficits, added to the difficulty of examining the optic disc when OND are present, complicate diagnosis and follow-up in patients with possible glaucomatous lesions.
B-mode ultrasonography is the most reliable means of diagnosing OND. They may also be detected using fluorescein angiography (fundus autofluorescence), CT, and fundoscopy.5
The most frequently identified visual field changes are arcuate defects, generalised visual field constriction, and enlarged blind spot; all types are slowly progressive. The visual field defect may or may not correspond to the OND location.4
The pathophysiological mechanisms that give rise to functional changes are as follows: impaired axonal transport in an eye with a small scleral canal, gradual secondary wear on optic nerve fibres, direct compression of drusen on prelaminar nerve fibres, and ischaemia in the optic nerve head.4
Visual acuity may decrease in some cases due to associated complications, including haemorrhages, arterial and venous occlusion, neovascular membranes, etc.; associated disease, such as retinitis pigmentosa or angioid streaks; and other concomitant causes, whether unrelated to the drusen or caused exclusively by drusen.3
Decreased visual acuity associated with papillary drusen is uncommon. When this defect is present, it is usually moderate and almost always associated with peripheral field changes. Visual acuity is significantly linked to the presence and number of visible drusen. Loss of central visual acuity without a visual field defect should orient us towards other associated causes.3
Experts recommend using B-mode ultrasonography to confirm the presence of OND and monitoring patients with visual field analysis and ONT to check the level of impairment of the nerve fibre layer.6
ONT and scanning laser polarimetry (GDx) have shown thinning of the nerve fibre layer in patients with OND, with greater losses being associated with more numerous and visible drusen. ONT seems to be the more sensitive than perimetry for detecting nerve fibre loss in its early stages.7
There is no consensus regarding treatment. Some studies have shown radial neurotomy to be effective since it relieves the pressure that drusen exert on nerve fibres. Others recommend neuroprotective agents, but not enough studies have been carried out to demonstrate the efficacy of this treatment.8
In conclusion, although OND are asymptomatic, the visual field defects they cause can be severe. We recommend using visual field analysis and ONT to monitor the status of these patients, and if their findings indicate progression, consider treatment with neuroprotective agents.
Please cite this article as: Bermúdez Vallecilla MC, Santos Bueso E, Sáenz Frances F, García Feijoo J. Alteraciones campimétricas graves en pacientes con drusas de nervio óptico. Neurología. 2015;30:383–385.