The COVID-19 pandemic has given rise to the need for changes in clinical practice, with new strategies to enable integrated care for patients with headache and neuralgia.
Material and methodsGiven the high spreadability of SARS-CoV-2, new safety measures are required in such procedures as onabotulinumtoxinA infiltration and nerve blocks.
ResultsWe present a series of recommendations based on the measures implemented to prevent infection in our healthcare system. We differentiate between measures related to patients and physicians, to technique, to infrastructure (waiting room and consultation), and to healthcare management.
La infección por SARS-CoV-2 y la situación de pandemia hacen necesario un cambio en nuestra práctica clínica, en relación con la adopción de nuevas estrategias que permitan la asistencia integral de los pacientes con cefalea y neuralgia.
Material y métodosAnte la elevada capacidad de transmisión del virus, determinados procedimientos, como la infiltración de onabotulinumtoxinA y la realización de bloqueos anestésicos, deben realizarse adoptando medidas que garanticen un nivel adecuado de seguridad.
ResultadosNuestro objetivo es presentar una serie de recomendaciones basadas en las medidas establecidas por nuestro sistema sanitario para evitar el contagio. Diferenciaremos entre aquellas medidas relacionadas con el paciente y el facultativo, con la técnica, con la infraestructura (sala de espera y consulta) y con la gestión asistencial.
The viral pneumonia outbreak that originated in Wuhan (China) in December 2019 has become a global pandemic. The World Health Organization declared the epidemic a public health emergency of international concern on 30 January 2020. In February 2020, the novel virus was officially denominated severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), with the associated disease being named COVID-19 (coronavirus disease 2019).1,2
The virus is transmitted through respiratory microdroplets, which are dispersed 1-2m when a person speaks or coughs. The virus is known to survive for an undetermined period of time on smooth surfaces, and as long as 72hours on plastic or stainless steel.3 In Spain, hospitals were forced to modify their healthcare practices with the publication of Royal Decree 463/2020 of 14 March,4 which declared a state of alarm for the management of the COVID-19 healthcare crisis.
According to data from the Spanish migraine action plan (PALM study), approximately 12% of the general population (one-year prevalence) have migraine (18% of women and 8% of men). Chronic migraine affects 2.4% of the population, with rates depending on the geographical area and the methods used. This study was used to draft a national migraine map with data for each Autonomous Community, which showed significant geographic variations, ranging from 7.6% in Navarre to 18% in the Canary Islands.5 Today, onabotulinumtoxinA (OnabotA) and anaesthetic nerve blocks are used to reduce the frequency of migraine attacks and number of headache days per month, and ultimately to improve patients’ quality of life.6
In this article, we present a series of recommendations to ensure adequate safety for both staff and patients, which are based on the measures implemented in the Spanish healthcare system to prevent the spread of SARS-CoV-2, adapted to our professional setting. These recommendations may be modified according to each centre's needs and characteristics.
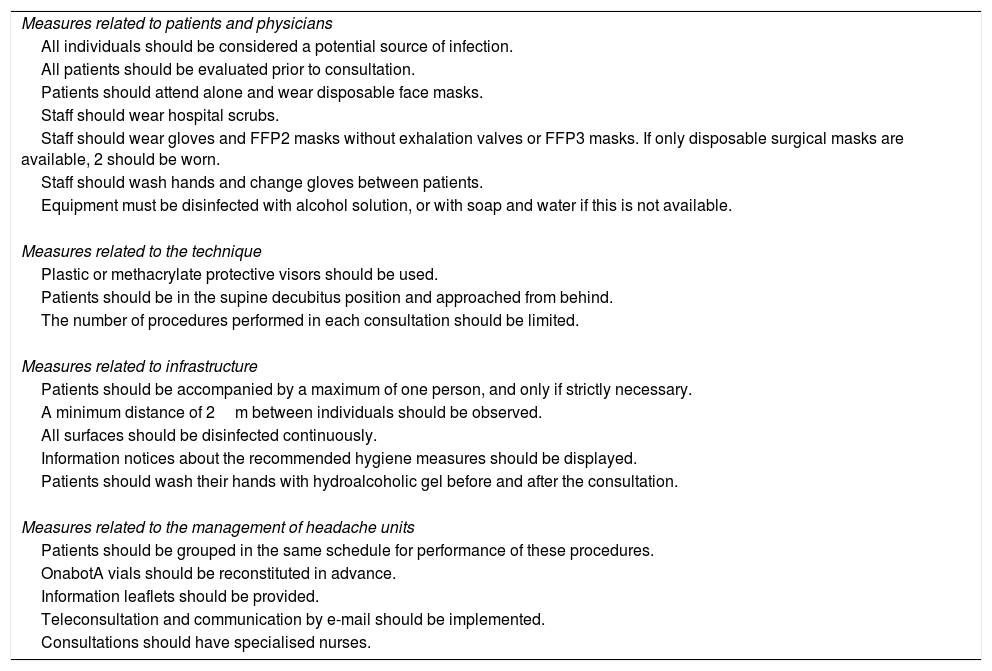
We differentiate between measures related to patients and physicians, to the technique, to infrastructure (waiting room and consultation), and to healthcare management (Table 1).
Recommendations for advanced treatment of patients with migraine.
| Measures related to patients and physicians |
| All individuals should be considered a potential source of infection. |
| All patients should be evaluated prior to consultation. |
| Patients should attend alone and wear disposable face masks. |
| Staff should wear hospital scrubs. |
| Staff should wear gloves and FFP2 masks without exhalation valves or FFP3 masks. If only disposable surgical masks are available, 2 should be worn. |
| Staff should wash hands and change gloves between patients. |
| Equipment must be disinfected with alcohol solution, or with soap and water if this is not available. |
| Measures related to the technique |
| Plastic or methacrylate protective visors should be used. |
| Patients should be in the supine decubitus position and approached from behind. |
| The number of procedures performed in each consultation should be limited. |
| Measures related to infrastructure |
| Patients should be accompanied by a maximum of one person, and only if strictly necessary. |
| A minimum distance of 2m between individuals should be observed. |
| All surfaces should be disinfected continuously. |
| Information notices about the recommended hygiene measures should be displayed. |
| Patients should wash their hands with hydroalcoholic gel before and after the consultation. |
| Measures related to the management of headache units |
| Patients should be grouped in the same schedule for performance of these procedures. |
| OnabotA vials should be reconstituted in advance. |
| Information leaflets should be provided. |
| Teleconsultation and communication by e-mail should be implemented. |
| Consultations should have specialised nurses. |
OnabotA: onabotulinumtoxinA.
Given the high transmissibility of SARS-CoV-2, a distance greater than 1.5m must be maintained to reduce the risk of infection. Examination of patients with headache requires a distance of less than 30cm, and even closer for certain procedures (direct ophthalmoscopy, palpation of cranial and cervical structures, etc.). As a result, these examinations present a risk and must be performed in accordance with the standard safety measures for these situations.7–9 Another key consideration is that the disease can be spread by healthcare professionals; therefore, prevention measures should be strictly observed.
- 1.
Given that the virus can be spread prior to symptom onset, and that many patients present few symptoms, all individuals should be considered as potential sources of infection.
- 2.
It is advisable for patients to be evaluated prior to entering the consultation to screen for possible exposure to the virus through questions about fever, general discomfort, respiratory symptoms (dry cough, dyspnoea), ageusia, anosmia, diarrhoea, and headache, and whether patients have had close contact or live with any individual recently diagnosed or under quarantine for COVID-19 in the last 14 days.
- 3.
Wherever possible, patients should attend consultations alone and wear disposable surgical face masks.
- 4.
Physicians should wear hospital scrubs.
- 5.
Gloves should be used in the examination of pericranial muscles, and the patient should be approached from the side. It is also essential to wear a face mask; the most recommended types are FFP2 masks without exhalation valves and FFP3 masks. If only disposable surgical masks are available, 2 should be worn. In high-risk patients, disposable gowns and protective plastic visors are also recommended. A personal protective suit and/or a surgical gown may be used.
- 6.
It is essential to wash hands and change gloves between patients. Professionals must be careful not to touch any equipment with gloves that have been used for the procedure/examination.
- 7.
All examination equipment must be disinfected with alcohol solution, or with soap and water if this is not available.
When administering OnabotA or performing anaesthetic nerve blocks or dry needling, professionals should also follow these additional recommendations:
- 1.
Plastic or methacrylate protective visors are recommended over goggles. As the virus is able to survive on plastic surfaces, these should be cleaned on both sides with disinfectant (e.g., alcohol) after each use.
- 2.
Patients should be in the supine decubitus position and be approached from behind. If this is not possible, they should remain seated. In the first case, the paper or sheet on the bed should be replaced following the procedure.
- 3.
The number of procedures performed in each consultation should be limited as far as possible, and those with the greatest level of evidence should be prioritised.
These recommendations may be generalised to all consultations and waiting rooms:
- 1.
Patients may be accompanied by a maximum of one person, where strictly necessary.
- 2.
Individuals should be separated by a distance of 2m. Overcrowding of waiting rooms should be avoided.
- 3.
All surfaces (doorknobs and handles, reception desks, telephones, computer equipment, pens, etc.) should be disinfected continuously.
- 4.
It is important to display information notices about the hygiene measures recommended by the health ministry and workplace health and safety services.
- 5.
Patients must enter the consultation alone and disinfect their hands with hydroalcoholic gel before and after the consultation. Gel dispensers should be placed in the waiting room for this purpose.
There can be no doubt that the pandemic will lead to significant delays in the provision of care for our patients.10 This makes it necessary to design strategies for the management of waiting lists, in accordance with care quality indicators for headache units11:
- 1.
In order to apply the measures described above, these patients should be grouped together in a single schedule.
- 2.
Reconstituting OnabotA vials ahead of time, depending on the number of patient appointments, will enable reduction of consultation times.
- 3.
Another highly practical consideration is the provision of information leaflets on the technique and the treatment for patients with de novo migraine to consult at home.
- 4.
Teleconsultation and electronic communication (telephone, e-mail) will become essential tools in everyday practice.12
- 5.
Specialist nurses with training in the assessment and care of patients with headache unquestionably play a key role in these consultations.13
The rapid spread of SARS-CoV-2 and the context of the pandemic will bring about a series of changes in the management of patients with migraine; fundamentally, this will involve the management of waiting lists and the implementation of new tools enabling integrated care within the framework of the safety regulations in force.
OnabotulinumtoxinA and anaesthetic nerve blocks constitute the cornerstone of migraine management. Performing these procedures with the utmost care in order to ensure our patients’ safety, in observance of the regulations in force, requires great responsibility on the part of physicians.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Santos-Lasaosa S, Porta-Etessam J. Infiltración con onabotulinumtoxinA y bloqueos en el paciente con cefalea y neuralgia: recomendaciones de seguridad frente a la infección por SARS-CoV-2. Neurología. 2020;35:291–294.