Herpes zoster is a condition caused by reactivation of the varicella-zoster virus (VZV), which remains latent in the dorsal root ganglia of the spinal cord, trigeminal ganglion, and other cranial nerves. It is characterised by a painful skin rash with blisters and affects one or more adjacent dermatomes. During this process, neurological complications may manifest, the most frequent being radiculopathies and cranial neuropathies; however, symptoms of myelitis, encephalitis, and central nervous system vasculitis may also be present.1 Myelitis, and especially extensive myelitis, is an infrequent and severe complication. It usually manifests days after the skin rash, although this may be absent (zoster sine herpete)2 or appear after several weeks. Myelitis may be infectious, parainfectious, or ischaemic in origin; each type requires different management.1
We present the case of a 70-year-old man with no relevant medical history who, 6 weeks after manifesting herpes zoster skin rash on the right T10 dermatome, presented subacute symptoms of urinary retention and difficulty walking due to weakness in the lower limbs. General examination revealed crusted lesions at the level of T10 dermatome and the neurological examination showed asymmetrical paraparesis of the lower limbs (right 3/5 and left 0/5 psoas, right and left quadriceps 3–/5, right 4/5 and left 3/5 tibialis anterior, and right 4/5 and left 3/5 gastrocnemius muscles) with intact deep tendon reflexes, bilateral Babinski sign, and sensory level at T7.
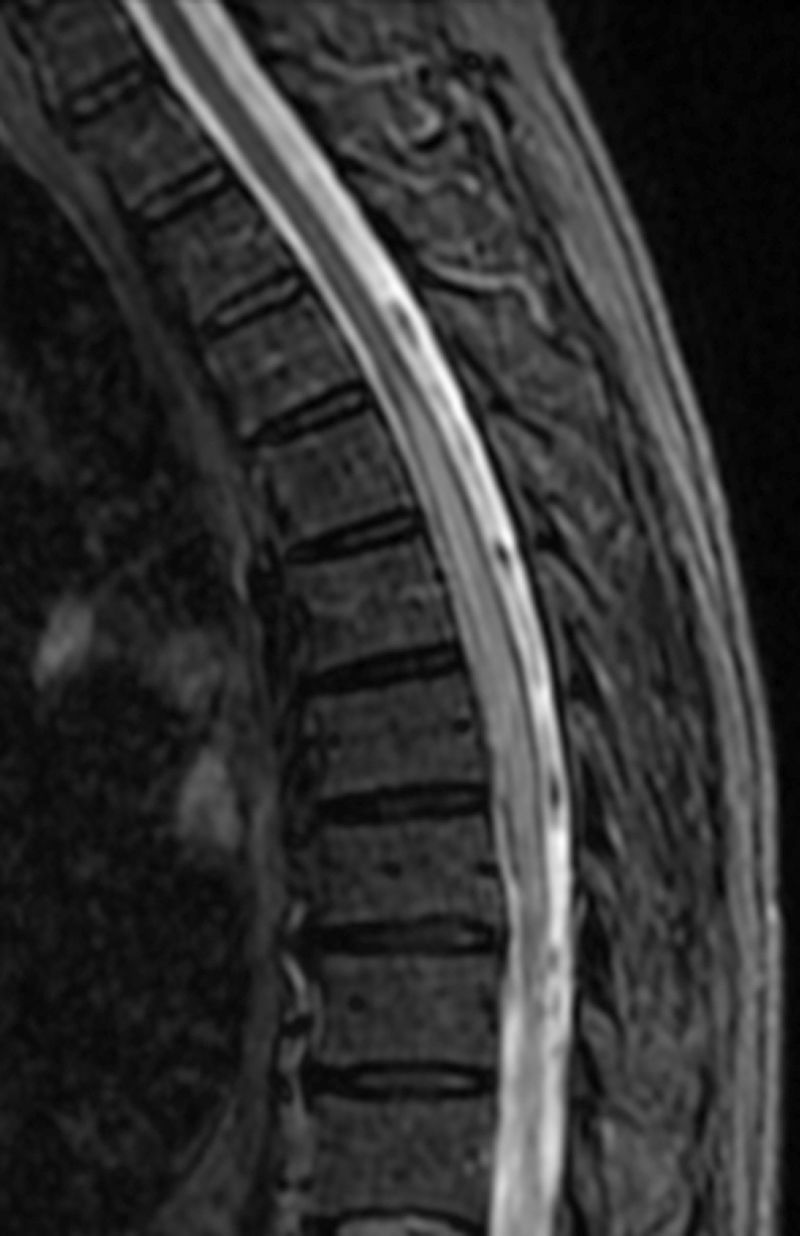
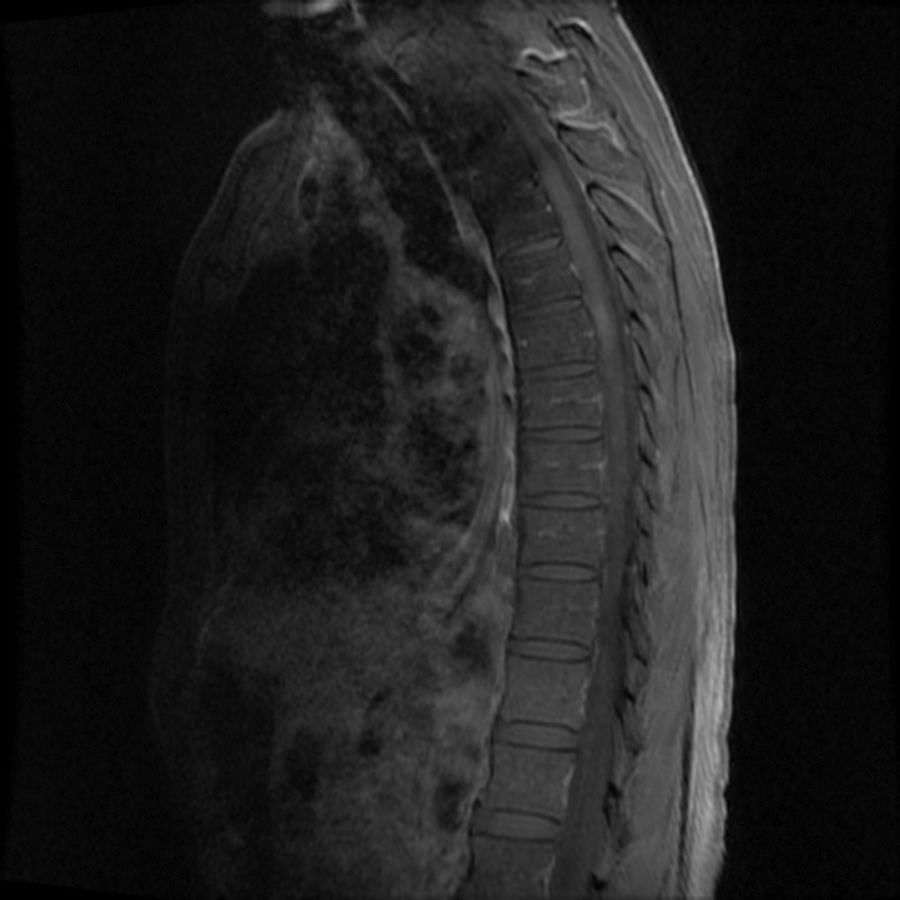
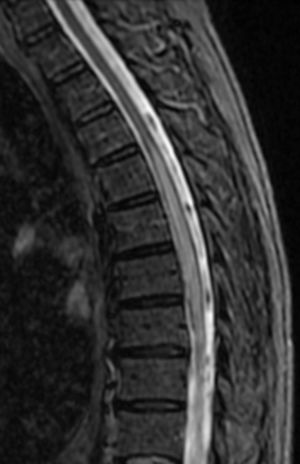
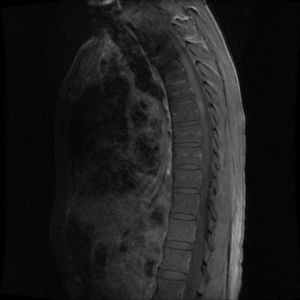
A cervicothoracic magnetic resonance imaging (MRI) scan showed a hyperintense lesion (STIR sequence) between T4 and T8, with contrast uptake mainly at the level of T5 (Figs. 1 and 2). Brain MRI results were normal. Lumbar puncture yielded clear cerebrospinal fluid (CSF) with 10 leukocytes (90% mononuclear) and normal protein and glucose levels. We also analysed CSF using PCR to detect VZV, HSV-1, and HSV-2, and ordered serology tests (IgM and IgG) for VZV, HSV, enterovirus, syphilis, Borrelia, and cryptococcus; fungal and mycobacterial cultures; IgM and IgG oligoclonal band tests; and a cytological study of malignant cells. All analyses yielded negative results. The results of a complete blood count were within normal ranges, and serology tests (HIV, EBV, CMV, HSV, VZV, enterovirus, HTLV-1, hepatitis, syphilis, Borrelia, Brucella, TB) yielded negative results, with the exception of VZV IgG. Results from the hypercoagulability study were normal; the tumour marker analysis, total protein test, and immunofixation test also revealed no abnormalities. We performed a study of systemic diseases of autoimmune aetiology (angiotensin-converting enzyme, complement, rheumatoid factor, ANA, ANCA, IgA antitransglutaminase, and aquaporin-4 [AQP4] antibodies); all results were normal. Having diagnosed longitudinally extensive transverse myelitis3 associated with VZV, we started treatment with intravenous (IV) aciclovir and corticosteroids, which achieved good outcomes. Aciclovir was suspended after serology test results were obtained.
Myelitis caused by VZV infection, especially when extensive, is a rare complication. It is essential to identify the aetiology as soon as possible, preferably at the time of diagnosis, since treatment depends on the aetiology. Considering the insidious onset of symptoms and the characteristics of the lesion on MR images, showing contrast uptake, we ruled out ischaemic origin and considered infectious or parainfectious myelitis as the most probable diagnoses. Differential diagnosis of these entities is performed by laboratory analysis.4,5 Infectious myelitis caused by direct invasion of the virus is characterised by the presence of VZV DNA and/or anti-VZV antibodies in the CSF. Virus DNA is undetectable after 7-14 days of rash onset; however, anti-VZV IgG antibodies increase their detection range from the first week, and persist indefinitely.4,5 Immune-mediated parainfectious myelitis is characterised by negative results in both tests. This interval between herpes zoster infection and the development of myelitis typically lasts days, and is similar in both cases. Each condition requires a different therapeutic approach. Whereas the treatment of choice for parainfectious myelitis is IV corticotherapy, treatment for infectious myelitis is IV aciclovir for 14-21 days. Likewise, we ruled out inflammatory, infectious, metabolic, and neoplastic systemic diseases which may cause myelitis. Furthermore, due to the extensive spinal involvement, we considered the possibility of it being an entity currently known as “neuromyelitis optica spectrum disorders”, with negative results for AQP4 antibodies; however, presence of these antibodies is not essential for diagnosis according to the latest criteria.6
VZV infection may cause several neurological complications, with myelitis being the most infrequent and severe. It may be infectious, parainfectious, or ischaemic in origin. Its differential diagnosis is fundamental for a correct therapeutic approach and treatment optimisation from symptom onset.
FundingThis study received no funding of any kind.
Please cite this article as: Arenaza-Basterrechea N, González Fernández J, Al Kassam Martínez D. Mielitis transversa longitudinal extensa parainfecciosa asociada a virus varicela zóster. Neurología. 2018;33:342–343.
This study was presented in poster format in the general neurology section at the 66th Annual Meeting of the Spanish Society of Neurology.