Intracranial lipomas (IL) are rare congenital lesions composed of adipose tissue that result from anomalous persistence and altered differentiation of the embryonic meninx primitiva during the development of the subarachnoid cisterns. The most frequent type is interhemispheric IL, which is usually located on the corpus callosum. They are frequently associated with callosal hypogenesis or agenesis.1 ILs are rarely associated with cortical malformations or vascular anomalies, such as aneurysms or arteriovenous malformations. The azygos anterior cerebral artery (ACA) is a rare anatomical variant, with an incidence below 1%, in which the distal (A2) segments of both ACAs fuse into a single vessel that supplies the medial part of both hemispheres.2 We present the first case, as far as we are aware, of simultaneous presence of pericallosal lipoma and azygos ACA.
Our patient is a 57-year-old woman with history of emotionally unstable personality disorder and previous consumption of amphetamines and cocaine. She has no family history of neurological disease.
The patient reported episodes of dizziness, progressing for several years. Family members witnessing the episodes reported that she presented pallor and was unresponsive to verbal stimuli; they observed no anomalous movements. Episodes lasted 5 minutes and muscle tone was preserved.
Laboratory analysis and electroencephalography yielded normal results.
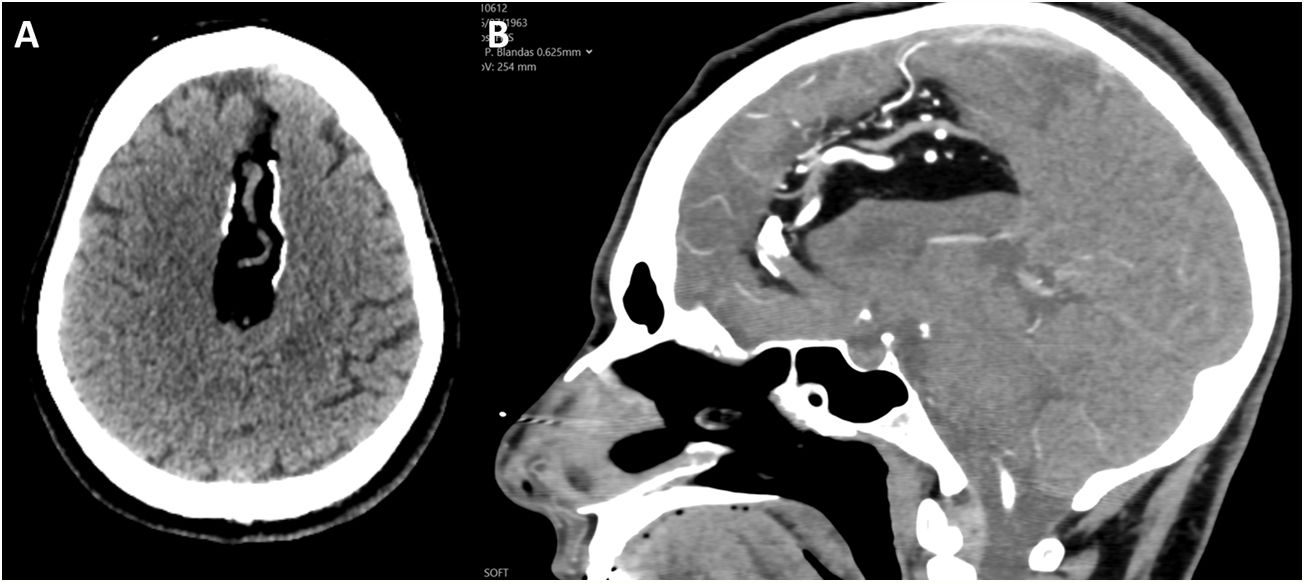
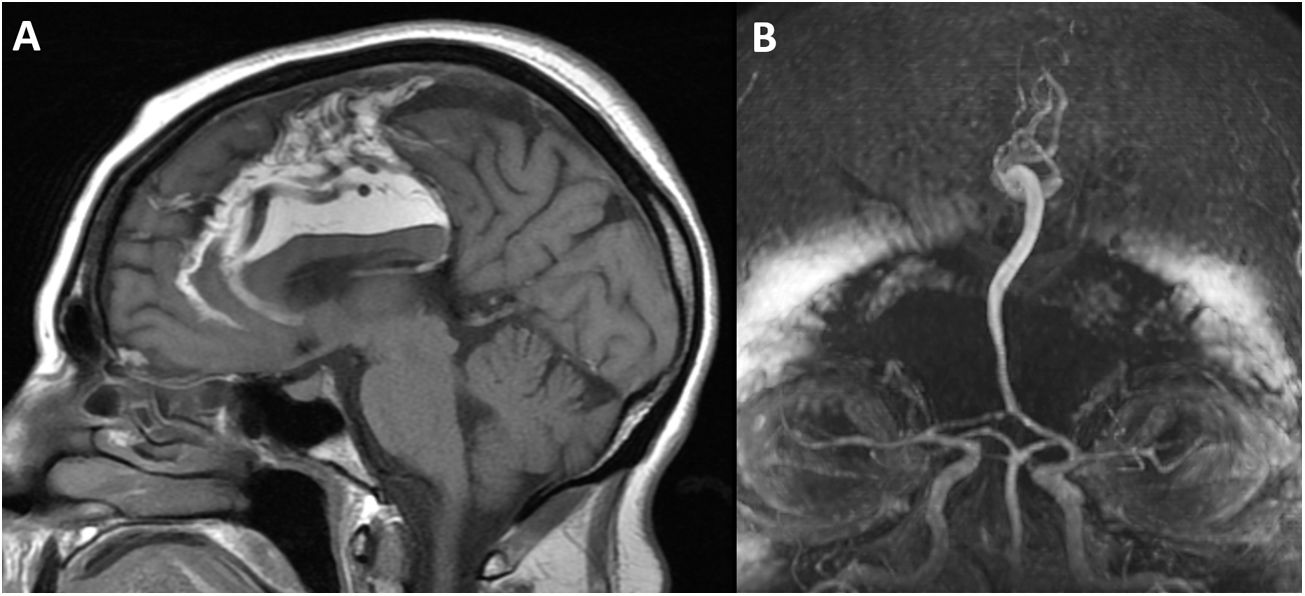
A contrast-enhanced computed tomography (CT) scan (Fig. 1) revealed a voluminous hypodense lesion compatible with interhemispheric IL, crossed by a single ACA, with partial peripheral calcifications. Brain MRI and MRI angiography (Fig. 2) showed the same lesion, with a signal similar to that of adipose tissue, closely related to the corpus callosum, with agenesis of the splenium. It was also associated with a vascular anomaly consisting of a prominent single ACA inside the lesion, with distal emergence of pericallosal and marginal callosal branches.
A) Non-contrast T1-weighted MRI sequence. The lesion shows hyperintensity compatible with fatty content; agenesis of the splenium of the corpus callosum and prominent venous drainage are also observed. B) Brain MRI angiography revealing a single arterial trunk distal to the anterior communicating artery, which is compatible with azygos anterior cerebral artery.
Given the patient’s clinical situation and the imaging findings, we adopted a conservative approach with radiological follow-up of the lesion.
ILs account for 0.1%-0.5% of all intracranial lesions. Their origin is most likely to be altered differentiation of meningeal tissue. They are made up of normal adipose tissue, and therefore are considered a congenital anomaly rather than a true neoplasm.1
Most ILs are located proximal to the midline, and 45% are interhemispheric lipomas. The remaining cases involve the quadrigeminal cistern (25%), the interpeduncular cistern (14%), the cerebellopontine angle (9%), and the Sylvian fissure (5%).3
More than half of ILs are associated with brain malformations, especially midline anomalies. The most frequent is callosal agenesis or dysgenesis. Absence of the septum pellucidum, spina bifida, encephalocele and myelomeningocele, and other cortical malformations have also been reported. Vascular anomalies such as aneurysms, arteriovenous malformations, or anomalous venous drainage may be present. Because growth of the IL and arterial development both occur during the first weeks of gestation, it has been suggested that they may be associated.4
Azygos ACA is a vessel resulting from the fusion of both pericallosal arteries. Anatomical series report its presence in fewer than 5% of patients. It occurs as a transient stage during embryonic development and is present in some mammals. It is frequently associated with other malformations of the CNS, such as porencephalic cysts, callosal agenesis, hydranencephaly, and arteriovenous malformations. The approximate incidence of aneurysms in these cases ranges from 13% to 71%.2
LIs are frequently asymptomatic and are usually incidental findings in imaging studies. However, headache, seizures, psychomotor developmental delays, and cranial nerve involvement have also been reported.5
Diagnosis is established by CT and MRI, which reveal a well-delimited, extra-axial, lobulated lesion, displaying the characteristics of adipose tissue. In the CT scan, density usually ranges from −50 to −100 HU, with peripheral calcifications especially in case of interhemispheric lipomas. In the MRI study, lesions are homogeneous, showing hyperintensity on T1- and T2-weighted sequences and hypointensity on fat-suppression sequences. Differential diagnosis usually includes dermoid cysts, teratoma, lipomatous transformation of a neoplasm, and subacute haemorrhage.3
Surgical resection of ILs is usually contraindicated as these are stable lesions with no mass effect on the parenchyma, and display a tendency to adhere to adjacent structures and present prominent vasculature, which involves a high surgical risk.5
Please cite this article as: Castro Castro J, Yáñez Baña RM, Lipoma pericalloso asociado a arteria cerebral anterior tipo ácigos. Neurología. 2021;36:731–732.