The term “pseudoperipheral palsy,” coined by Jean Lhermitte, refers to weakness predominantly affecting the hand (pseudoulnar, pseudomedian, or pseudoradial nerve palsy)1 associated with a central nervous system lesion, mimicking a lesion to the peripheral nervous system.2,3 Pseudoperipheral palsy is rarely caused by ischaemic stroke (< 1% of cases),2 and association with haemorrhagic stroke is even rarer.
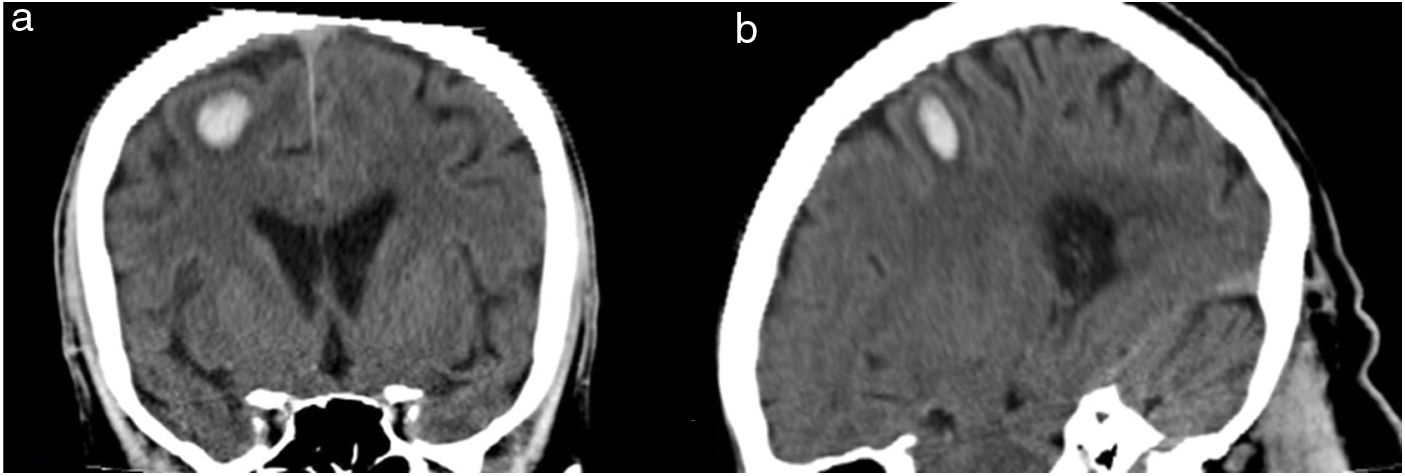
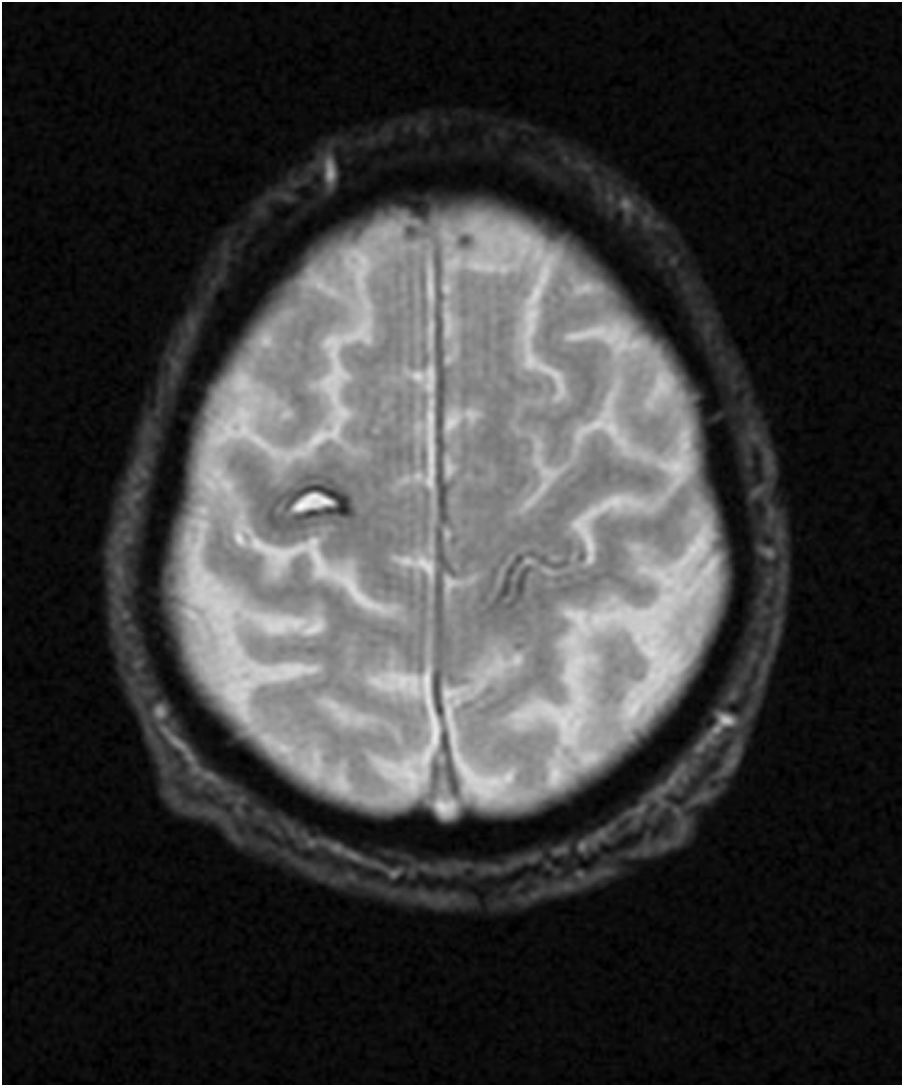
We present the case of an 82-year-old right-handed man with no known vascular risk factors. He went to bed with no symptoms and when he awoke at 03:00 to urinate, he presented lack of coordination in the left hand, with no headache, neurovegetative symptoms, or any other neurological symptoms. He reported no pain or sleeping on the left limb. Upon arrival at our centre, blood pressure was 150/90 mm Hg. The neurological examination revealed weakness (4/5) in extension of the left fingers, thumb, and wrist, and normal strength (5/5) in finger flexion. The biceps, brachioradialis, triceps, and wrist flexor muscles showed normal strength. The intrinsic muscles of the hand and the opponens pollicis, adductor pollicis, and flexor pollicis longus muscles showed normal strength; pronosupination and proximal muscles also showed normal strength. Sensitivity and all other areas of the neurological examination were normal. Although these findings are compatible with posterior interosseous nerve syndrome, we requested a head CT scan given the lack of evident nerve compression and the normal strength of the finger flexors; the study revealed a small haematoma in the right precentral gyrus (Fig. 1). A blood analysis yielded no relevant findings. A brain MRI scan performed 3 months after the event revealed subacute/chronic haematoma in the right precentral gyrus and no intracranial aneurysms, fistulas, or arteriovenous malformations (Fig. 2). The patient was prescribed rehabilitation treatment at discharge; a 3-month follow-up examination revealed improvements in mobility of the distal extensor muscles, with complete functional recovery.
According to the Penfield homunculus model, the cortical neurons that innervate the upper limbs are located in the lower third of the dorsolateral surface of the precentral gyrus, corresponding with Brodmann area 4.1,3–5 Advances in brain imaging have led to an improvement in the characterisation of the cortical representation of the hand. The hand motor cortex has an inverted omega shape in most cases (90%), with some individuals (10%) displaying a horizontal epsilon shape on the axial plane and a hook shape on the sagittal plane.3,4 However, finger movement is controlled by a profusely distributed neuronal network, rather than by spatially and functionally separated bundles of neurons.1
Our patient presented signs of posterior interosseous nerve syndrome associated with a small haematoma in the precentral gyrus. The literature includes several cases of ischaemic stroke associated with isolated hand palsy without sensory involvement6,7; however, the association with haemorrhagic stroke has not previously been reported. In addition to the precentral gyrus, pure motor involvement of the hand may be associated with lesions to the angular gyrus, the ventral posterolateral nucleus of the thalamus, the internal capsule, the corona radiata, and the base of the pons.8
Differential diagnosis should include C7 radiculopathy, radial nerve dysfunction, vasculitis associated with hyperacute mononeuropathy, spinal cord disease, hereditary neuropathy with liability to pressure palsy,7 and atypical lacunar syndromes.9 Diagnosis of this entity requires a high level of clinical suspicion due to its clinical and therapeutic implications and the non-specificity of examination findings. Sudden onset with no trauma or nerve compression, lack of pain, presence of cardiovascular risk factors, and normal neurophysiological study results may assist in diagnosis.3,6,7 Synkinetic wrist extension following fist closure is a useful exploratory sign for differentiating central from peripheral radial nerve palsy: a slight elevation of the clenching hand (with the arm held out and palm facing the floor) is observed in patients with central radial nerve palsy, whereas further wrist drop is observed in patients with peripheral radial nerve palsy.6 This is explained by the fact that in peripheral wrist drop, synkinetic contraction of the long forearm flexors is not counterbalanced by simultaneous activation of the long extensor muscles.
In summary, the extension of the hand motor cortex, located on the anterior wall of the central sulcus (Brodmann area 4), means that lesions to strategic areas can occasionally cause isolated hand paresis that may be mistaken for a peripheral syndrome. Given the therapeutic and prognostic implications of this association, acute stroke should be included in the differential diagnosis of sudden-onset peripheral motor deficits, particularly in patients not presenting pain or signs of nerve compression.
Please cite this article as: Sancho Saldaña A, Ciotti López M, Capablo Liesa JL. Cuando lo central parece periférico: síndrome del interóseo posterior como manifestación aislada de ictus hemorrágico. Nefrologia. 2020;35:659–660.