The reported prevalence of myasthenia gravis ranges between 5 and 24 cases per 100,000, and people over 65years account for less than 50% of all cases. The prevalence and clinical characteristics of myasthenia gravis in the county of Osona were studied in patients younger and older than 65.
MethodsThe study draws from the county-based prospective myasthenia gravis register implemented by the Neurology Department at Hospital General de Vic in 1991.
ResultsThe prevalence of myasthenia gravis was 32.89×105 inhabitants (95% CI, 23.86–41.91). The standardised prevalence (European population) was 35.47×105 inhabitants (95% CI, 26.10–44.84). The ratio of women to men was 1.3. Overall, the group of patients older than 65 accounted for 62.75% of all cases. The prevalence of myasthenia gravis increased considerably in older age groups. No cases were registered among patients under 25 years old, prevalence was 21.87×105 in the 25 to 64 age group, and prevalence in patients over 65 years increased to 122.35×105. The clinical characteristics prior to treatment and at the cut-off date are similar (P>.05) in patients younger than 65 and those aged 65 and older.
ConclusionsThese figures show the highest prevalence rate reported to date. This high prevalence is due to the rate observed among patients older than 65. These results provide a new warning that myasthenia gravis may be underdiagnosed in the elderly population.
La prevalencia descrita de miastenia gravis (MG) oscila entre 5 y 24 casos por 100.000, representando los mayores de 65 años menos del 50% del total. Se presenta la prevalencia de MG en la comarca de Osona (Barcelona, España). Se describen la prevalencia y las características clínicas por grupos de edad, diferenciando los menores y mayores de 65 años.
MétodosEl Servicio de Neurología del Hospital General de Vic puso en marcha en el año 1991 un registro comarcal sobre los casos de MG diagnosticados.
ResultadosLa prevalencia de MG fue de 32,89×105 habitantes (IC 95%, 23,86–41,91). La prevalencia estandarizada (población europea) fue del 35,47×105 habitantes (IC 95%, 26,10–44,84). La razón por sexo, mujeres/hombres, es de 1,3. De forma global, el grupo de más de 65 años representa el 62,75% de los casos. Las prevalencias de MG por grandes grupos de edad presentan un carácter marcadamente ascendente, pasando de ningún caso en el grupo de menos de 25 años, a 21,87×105 en el grupo de 25 a 64 años, alcanzando 122,35×105 en el grupo de 65 y más años. Las clínicas pretratamiento y a fecha de corte no presentan diferencias estadísticamente significativas (p>0,05) entre menores y mayores de 65años.
ConclusionesSe describe la prevalencia más alta comunicada hasta la actualidad. Esta alta prevalencia es a expensas del grupo de más de 65 años. Estos resultados son una nueva alerta para evitar el infradiagnóstico de la MG en el anciano.
Myasthenia gravis (MG) may be underdiagnosed in elderly patients since some of its initial symptoms, including diplopia, dysphagia, dysarthria, dyspnoea, limb weakness, and repeated falls, are usually attributed to other more frequent diseases in this age group.1 In the early 1990s, onset of MG in patients older than 70 was considered to be extremely rare. Surprisingly, most new cases in our hospital were elderly patients. For this reason, a specific database for cases of MG in the county of Osona (Catalonia) was created in 1991. The mean annual incidence of MG between 1991 and 2000 was found to be 21.3 cases per million people; this rate was higher than anticipated, especially due to the number of cases among the elderly.2 Between 2001 and 2010, the incidence rate was 28.0 cases per million people, with a median age of 74 years; the incidence increased each decade from the age of 65. MG should therefore be considered a disease of the elderly.3 Other studies have also shown a high incidence of this disease in elderly patients.4–6
The estimated prevalence of MG ranges between 5 and 24 cases per 100000 people; patients older than 65 represent less than 50% of the total.7,8 These studies have been conducted in large populations or are drawn from the health system's diagnostic records, this approach may not be conducive to correct identification of cases used to calculate the prevalence. The incidence rates found in Osona suggest an even higher prevalence of MG.
We analyse the prevalence of MG in a county in the province of Barcelona more than 20 years after the creation of an MG register; during this period, the highest incidence to date was reported on 2 occasions.2,3 We also describe the prevalence and clinical characteristics of our patient sample broken down by age group (younger than vs older than 65). From a demographic viewpoint, the county of Osona has an elderly population: in 2013, 16.87% of the total inhabitants were at least 65.9 In 2014, life expectancy in Catalonia reached 79.5 years for men and 85.3 years for women.9
Patients and methodsHospital General de Vic is located in Osona, a county in the north of the Catalan province of Barcelona, in Spain. It provides care to a population of 155069 inhabitants according to the 2013 census.9 Ours is the only public system reference hospital in this county.
The group of patients older than 65 includes those aged 65 exactly.
In 1991, the neurology department of Hospital General de Vic created a register for the cases diagnosed with MG. All neurologists in the county of Osona, whether or not they work at our hospital, contribute to updating the register. The reference hospitals outside Osona have also been contacted to gather data on any patients with MG who may not have been treated in any public or private hospitals in that county. This register provides valuable data for cohort studies, whether clinical (treatments provided to these patients) or epidemiological (incidence, prevalence, and survival). The diagnosis of MG is established based on clinical signs and findings in the neurological examination, and confirmed by the presence of acetylcholine receptor (AChR) or muscle-specific receptor tyrosine kinase (MuSK) antibodies in serum. When serology tests yield negative results, the Tensilon test and a neurophysiological study (repetitive stimulation or single-fibre study) can corroborate the diagnosis.
The variables used in this study were the following: diagnosis of MG, sex, age (at the time of prevalence estimation), symptom onset, mean progression time of MG, clinical presentation according to the criteria of the Myasthenia Gravis Foundation of America,10 presence of antibodies, EMG results, response to cholinesterase inhibitors, immunological comorbidities, and presence of thymoma.
To calculate the prevalence of MG in 2013, we used the number of patients diagnosed with MG who were alive as of 1 July 2013 and living in any of the 51 towns in the county of Osona, compared to the total population (de facto) of the county in 2013. We used the European standard population to calculate the adjusted prevalence.11 To calculate prevalence by sex we used the number of living men/women with MG who were residing in Osona as of 1 July 2013 and the total male/female population of Osona. To calculate prevalence by age, we used the number of patients with MG in each age group and the total population for each age group.
We conducted an epidemiological study using a sample drawn from an active register of patients with MG. The statistical analysis included the chi-square test, Yates correction, and the Fisher exact test. We estimated the 95% CI for prevalence rates and mean progression times. Significance was established at P=.05. Statistical analysis was performed using Microsoft Office Excel 2007 and PASW version 18.
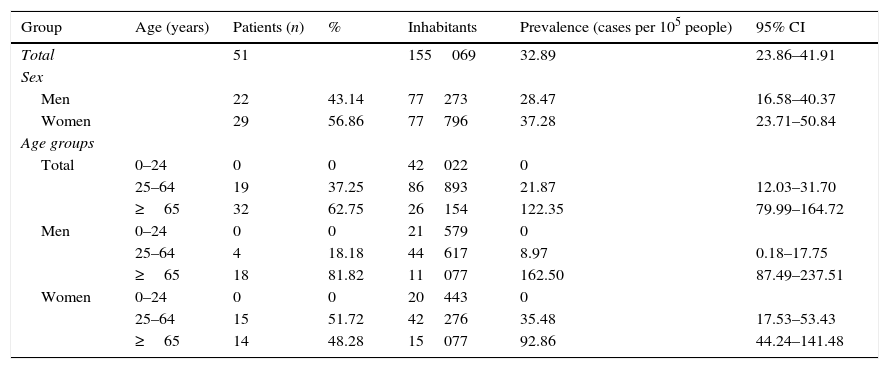
ResultsWe found 51 patients with a diagnosis of MG and alive as of 1 July 2013. Based on the total population of Osona in 2013 (155069 inhabitants), the prevalence of MG in this county in 2013 was 32.89 cases per 100000 people (95% CI, 23.86–41.91). The standardised prevalence (based on the European standard population) was 35.47 cases per 100000 people (95% CI, 26.10–44.84). Twenty-nine patients were women and 22 were men; the prevalence rate for each sex was 37.28 cases per 100000 people in women (95% CI, 23.71–50.84) and 28.47 cases per 100000 people in men (95% CI, 16.58–40.37). The female-to-male ratio was 1.3; by age group, it was 3.75 in patients younger than 65 and 0.78 in those older than 65. The median age at the time when prevalence was estimated was 74.86 years (64.63 in women, 83.04 in men). Mean progression time of the disease was 9.11 years (95% CI, 0.05–18.17). Prevalence of MG increased significantly with age: whereas no cases were found in residents younger than 25, prevalence was 21.87 cases per 100000 people (95% CI, 12.03–31.70) in the group aged 25–64 and 122.35 cases per 100000 people (95% CI, 79.99–164.72) in patients older than 65 (Table 1).
Prevalence of myasthenia gravis in the county of Osona in 2013.
| Group | Age (years) | Patients (n) | % | Inhabitants | Prevalence (cases per 105 people) | 95% CI |
|---|---|---|---|---|---|---|
| Total | 51 | 155069 | 32.89 | 23.86–41.91 | ||
| Sex | ||||||
| Men | 22 | 43.14 | 77273 | 28.47 | 16.58–40.37 | |
| Women | 29 | 56.86 | 77796 | 37.28 | 23.71–50.84 | |
| Age groups | ||||||
| Total | 0–24 | 0 | 0 | 42022 | 0 | |
| 25–64 | 19 | 37.25 | 86893 | 21.87 | 12.03–31.70 | |
| ≥65 | 32 | 62.75 | 26154 | 122.35 | 79.99–164.72 | |
| Men | 0–24 | 0 | 0 | 21579 | 0 | |
| 25–64 | 4 | 18.18 | 44617 | 8.97 | 0.18–17.75 | |
| ≥65 | 18 | 81.82 | 11077 | 162.50 | 87.49–237.51 | |
| Women | 0–24 | 0 | 0 | 20443 | 0 | |
| 25–64 | 15 | 51.72 | 42276 | 35.48 | 17.53–53.43 | |
| ≥65 | 14 | 48.28 | 15077 | 92.86 | 44.24–141.48 | |
CI: confidence interval.
Overall, the group of patients over 65 represents 62.75% of the total number of cases of MG (81.82% of men and 48.28% of women in our sample are over 65) (Table 1). Prevalence increases each decade in the group of patients aged over 65, from 60.95 cases per 100000 people in patients aged 65.74 to 144.61 cases in patients aged 75–84 and 232.72 cases in those over 85.
AChR antibodies were found in 78.4% of our sample; no significant differences were found between sexes and age groups (P>.05). According to the classification of the Myasthenia Gravis Foundation of America, pre-treatment disease severity in our sample was as follows: class I (n=18) 35.3%, class II (IIa, n=3; IIb, n=15) 35.3%, class III (IIIa, n=1; IIIb, n=10) 21.6%, class IV (IVa, n=2; IVb, n=2) 7.8%, and class V (n=0) 0%. Clinical status at the time when prevalence was estimated was as follows: asymptomatic (n=11) 21.6%, class I (n=14) 27.5%, class II (IIa, n=8; IIb, n=18) 51.0%, class III (n=0) 0%, class IV (n=0) 0%, and class V (n=0) 0%. No statistically significant differences (P>.05) were found in symptoms in the pre-treatment status and the clinical status at the time of prevalence estimation between patients younger and older than 65 or between sexes.
Other immunological phenomena were found in 21.57% of the patients. Six patients had vitamin B12 deficiency, 3 had Hashimoto thyroiditis, and 2 had vitiligo. Immunological comorbidities were more frequent among patients older than 65 (P<.05).
Thymoma was present in 11.8% of the patients; no significant differences (P>.05) were found between sexes or age groups (younger vs older than 65).
DiscussionOur study shows the highest prevalence of MG reported to date. This increased prevalence rate is due to the high prevalence of MG in the group of patients older than 65. The high prevalence in the elderly population was more marked in the study of MG incidence in Osona, in which 75% of the cases were in older patients. The difference may be explained by the fact that patients with earlier-onset MG have shorter survival times.
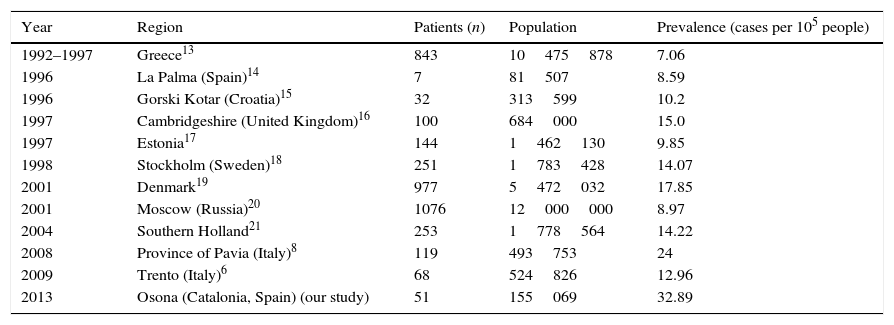
Table 2 shows prevalence rates of MG in different European regions. Most of these studies are based on the registers kept by hospitals or other health services. In contrast, our methodology ensures a better patient selection since we gathered data from an active register and a limited population, which allows for better detection of cases. Other factors contributing to better patient selection are the participation of all the neurologists of Osona and the role of general practitioners, who are now more familiar with MG thanks to the creation of a register more than 20 years ago.
Prevalence of myasthenia gravis in different European regions.
| Year | Region | Patients (n) | Population | Prevalence (cases per 105 people) |
|---|---|---|---|---|
| 1992–1997 | Greece13 | 843 | 10475878 | 7.06 |
| 1996 | La Palma (Spain)14 | 7 | 81507 | 8.59 |
| 1996 | Gorski Kotar (Croatia)15 | 32 | 313599 | 10.2 |
| 1997 | Cambridgeshire (United Kingdom)16 | 100 | 684000 | 15.0 |
| 1997 | Estonia17 | 144 | 1462130 | 9.85 |
| 1998 | Stockholm (Sweden)18 | 251 | 1783428 | 14.07 |
| 2001 | Denmark19 | 977 | 5472032 | 17.85 |
| 2001 | Moscow (Russia)20 | 1076 | 12000000 | 8.97 |
| 2004 | Southern Holland21 | 253 | 1778564 | 14.22 |
| 2008 | Province of Pavia (Italy)8 | 119 | 493753 | 24 |
| 2009 | Trento (Italy)6 | 68 | 524826 | 12.96 |
| 2013 | Osona (Catalonia, Spain) (our study) | 51 | 155069 | 32.89 |
The higher prevalence of MG in women is fundamentally due to rates in the group of patients younger than 65. At older ages, prevalence increases in both sexes although MG predominantly affects men, especially those over 85.
No significant differences were found between patients younger than and older than 65, or between men and women, in terms of pre-treatment disease severity, symptoms at the time prevalence was estimated, presence of AChR antibodies, or presence of thymomas. Immunological comorbidities are frequent and predominantly affect patients older than 65. Immune senescence may be responsible for MG and other immunological diseases in the elderly.12
Our results underline the importance of avoiding underdiagnosis of MG in elderly patients. MG is a potentially severe disease but one that usually responds well to treatment. Early diagnosis by general practitioners and greater access of elderly patients to specialised care are therefore essential.
Ethical disclosuresOur study of the prevalence of MG poses no legal or ethical conflicts since no interventions were performed and the statistical analysis respected the confidentiality of patient data.
FundingThis study has received no public or private funding.
Conflict of interestThe authors have no conflict of interest to declare.
We would like to thank Drs A. Arboix and J. Monells for their contributions.
Please cite this article as: Aragonès JM, Altimiras J, Roura P, Alonso F, Bufill E, Munmany A, et al. Prevalencia de miastenia gravis en la comarca de Osona (Barcelona, Cataluña). Neurología. 2017;32:1–5.