According to the Spanish Stroke Health Care Plan and the Spanish Health National Service Stroke Strategy, thrombolysis should only be performed in hospitals with Stroke Units. However, the Andalusian Stroke Health Care Plan excludes, within the list of services of the Stroke Team, the need to have a neurologist present for the performing of thrombolysis in local hospitals. The objective of this study is to evaluate whether emergency doctors are able to achieve a reliable diagnosis of stroke in order to safely perform thrombolysis.
MethodsThe diagnoses on hospital admission and discharge of all patients admitted for neurological reasons in 2006 in the community Hospital Infanta Elena (Huelva, Andalusia) were collected. The reliability of diagnosis performed by emergency doctors was analysed.
ResultsA total of 655 patients were admitted to the hospital for neurological reasons, and 76% of them were diagnosed as strokes. The sensitivity of stroke diagnosis made by emergency doctors was very high (97%), but specificity and positive predictive value of that diagnosis was low (52% and 75%, respectively).
ConclusionsTo apply thrombolysis based of the diagnosis of a stroke by emergency doctors may subject a significant number of erroneously diagnosed patients to an unnecessary risk of brain haemorrhage. This risk makes performing thrombolysis in community hospitals ethically questionable in these circumstances. Although it is important to have thrombolytic treatment available to everyone, this treatment must be performed safely by neurologists Stroke Units.
Tanto en el Plan de atención sanitaria al ictus como en la Estrategia en ictus del Sistema Nacional de Salud se establece que solo se realizará fibrinólisis en los hospitales con unidad de ictus. Sin embargo, en Andalucía el Plan andaluz de atención al ictus incluye dentro de la cartera de servicios del equipo de ictus en los hospitales comarcales la realización de fibrinólisis prescindiendo de la figura del neurólogo en el tratamiento agudo del ictus. El objetivo de este estudio es evaluar si los médicos de urgencias realizan adecuadamente el diagnóstico de ictus.
MétodosSe recogieron los diagnósticos realizados en urgencias y al alta de hospitalización de todos los pacientes ingresados por motivos neurológicos en el hospital comarcal Infanta Elena durante el año 2006. Se analizó la validez del diagnóstico realizado en urgencias.
ResultadosEl número de ingresos por patología neurológica fue de 655 pacientes en 2006, representando el ictus un 76%. Aunque la sensibilidad del diagnóstico de ictus en urgencias resultó alta (95%), la especificidad del diagnóstico era muy baja (52%) y el valor predictivo positivo de un 75%.
ConclusionesAplicar la fibrinólisis sobre la base del diagnóstico de ictus en urgencias implica someter a un riesgo no justificado de hemorragia cerebral a un número importante de pacientes diagnosticados erróneamente. Este riesgo hace cuestionable éticamente la administración de dicho tratamiento en los hospitales comarcales en las condiciones actuales. No solo es importante que el tratamiento fibrinolítico sea accesible a la población sino que dicho tratamiento se realice de forma segura por neurólogos en unidades de ictus.
The American Stroke Association states, based on level 1 evidence, that thrombolysis with intravenous rtPA is beneficial in patients with acute ischaemic stroke within 4.5hours of symptom onset.1,2 The efficacy of this treatment means that it is necessary to organise a healthcare network capable of providing it to the entire population. With this in mind, some aim to make fibrinolytic treatment for brain infarcts more similar to that for acute myocardial infarction, in the sense of allowing treatment to be administered by doctors who are not cerebrovascular specialists (emergency department and intensive care doctors, etc.) in centres without an on-call neurologist.
However, there are two fundamental differences between the treatments mentioned above. On the one hand, the risk of symptomatic intracranial haemorrhaging with fibrinolytic treatment for cerebral infarct is much higher than with AMI (6.4%–15.7% of patients with cerebral infarct3–6 vs 0.65% of patients with AMI. On the other hand, correctly diagnosing a stroke, which is the foundation of the decision to administer fibrinolytic treatment to the patient, is difficult due to the wide variety of clinical manifestations. Strokes are often diagnosed incorrectly by non-experts.
In 2006, Spain's stroke care plan (PASI in Spanish)6 was drawn up by the Spanish Society of Neurology's Study Group for Cerebrovascular Diseases, and this plan has recently been revised.7 The Spanish National Health System (SNS) used that plan to develop its stroke care strategy8 within the framework of the SNS quality plan. The strategy presents the main action plan for stroke care used throughout Spain. This strategy was approved by the Inter-regional Council of the SNS in 2008, and published and presented in March 2009. Both PASI7 and the SNS stroke care strategy9 establish 3 different categories for hospitals from the viewpoint of stroke patient care: hospitals with stroke care teams (SCT), those with stroke units, (SU) and those with units of reference for specialised techniques. The SCT is the basic care model in local hospitals and it should be coordinated by a neurologist specialising in ictus. According to the established model, hospitals with SCT cannot administer fibrinolysis for stroke during the acute phase; this is only done in hospitals with SU and on-call neurologists. However, the Andalusian stroke care plan,9 created for the purpose of implementing the SNS strategy, includes fibrinolysis for stroke among its SCT services. As a result, fibrinolysis may be performed in all hospitals, regardless of whether or not they have an SU. Additionally, the neurologist in the role of the SCT coordinator is replaced by a specialist in stroke management, and neurologists are not listed among the professionals making up the team. In short, the Andalusian stroke care plan does not require neurologists for the treatment of acute strokes.
The purpose of this study, carried out during the first year after a neurology department was added to a local hospital in Andalusia, is to determine whether or not emergency department doctors diagnose stroke correctly. This is relevant to the implementation of acute-phase treatments with a delicate risk/benefit ratio, including fibrinolysis. This study becomes all the more important when we consider that in Andalusia, unlike in all other Spanish autonomous communities, fibrinolysis is performed by emergency department doctors and intensive care specialists.
Patients and methodsAll diagnoses performed by the emergency department and upon discharge from a hospital ward were recorded between 1 January 2006 and 15 December 2006 for patients with neurological illnesses admitted to Hospital Infanta Elena (HIE), the local hospital serving Huelva province. Patients were admitted to either the neurology ward (NL) or the internal medicine ward (IM).
Diagnoses upon admission were taken from the emergency department treatment forms. Diagnoses upon discharge was taken from the discharge report written by the specialist who attended the patient in the hospital ward. Using those diagnoses, we completed a descriptive study of neurological disorders by order of their frequency.
We analysed the percentage of emergency department diagnoses that were changed. The validity of diagnoses of stroke declared by emergency doctors was calculated by comparing them to the “gold standard” diagnoses on the discharge reports. Following this method, we calculated sensitivity, specificity, percentage of false positives and negatives, and positive and negative predictive values (PPV and NPV). The same analysis was performed after excluding patients with intracranial haemorrhage (not candidates for fibrinolysis) and establishing subgroups (patients evaluated/not evaluated by NL during their stay).
In the descriptive study, we used the absolute and relative frequencies of each category of qualitative variable, and presented figures adjusted for missing values. This was done using Statistical Package for Social Sciences software (SPSS, Chicago, USA) version 14.0.
We calculated the validity of stroke diagnoses established by the emergency department using a Microsoft Excel 2003 spreadsheet. Results are expressed as percentages with 95% confidence intervals.
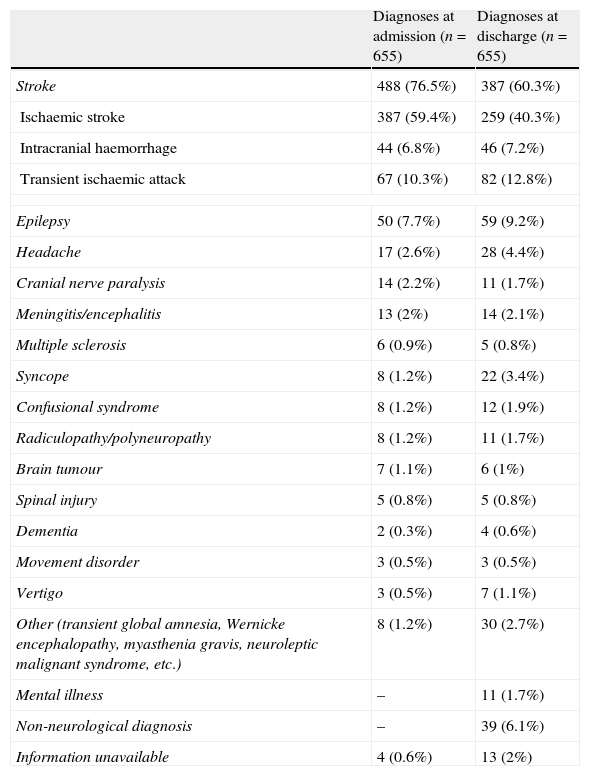
ResultsBetween 1 January and 15 December 2005, 655 patients were admitted to the HIE for neurological illnesses. The most common neurological illness, according to the diagnoses established by emergency departments, was stroke, which affected 488 of the patient total of 655 (76.5%). Ischaemic stroke was the most common diagnosis, followed by transient ischaemic attack, followed by intracranial haemorrhage (ICH); these diagnoses accounted for 59.4%, 10.3%, and 6.8% of the total, respectively. The remaining 167 patients were diagnosed with other non-vascular neurological complaints; of these, the most common were epilepsy, headaches, cranial nerve pair paralysis and meningitis (Table 1).
Patients diagnosed with neurological disease upon admission: diagnoses at admission and at discharge.
| Diagnoses at admission (n=655) | Diagnoses at discharge (n=655) | |
| Stroke | 488 (76.5%) | 387 (60.3%) |
| Ischaemic stroke | 387 (59.4%) | 259 (40.3%) |
| Intracranial haemorrhage | 44 (6.8%) | 46 (7.2%) |
| Transient ischaemic attack | 67 (10.3%) | 82 (12.8%) |
| Epilepsy | 50 (7.7%) | 59 (9.2%) |
| Headache | 17 (2.6%) | 28 (4.4%) |
| Cranial nerve paralysis | 14 (2.2%) | 11 (1.7%) |
| Meningitis/encephalitis | 13 (2%) | 14 (2.1%) |
| Multiple sclerosis | 6 (0.9%) | 5 (0.8%) |
| Syncope | 8 (1.2%) | 22 (3.4%) |
| Confusional syndrome | 8 (1.2%) | 12 (1.9%) |
| Radiculopathy/polyneuropathy | 8 (1.2%) | 11 (1.7%) |
| Brain tumour | 7 (1.1%) | 6 (1%) |
| Spinal injury | 5 (0.8%) | 5 (0.8%) |
| Dementia | 2 (0.3%) | 4 (0.6%) |
| Movement disorder | 3 (0.5%) | 3 (0.5%) |
| Vertigo | 3 (0.5%) | 7 (1.1%) |
| Other (transient global amnesia, Wernicke encephalopathy, myasthenia gravis, neuroleptic malignant syndrome, etc.) | 8 (1.2%) | 30 (2.7%) |
| Mental illness | – | 11 (1.7%) |
| Non-neurological diagnosis | – | 39 (6.1%) |
| Information unavailable | 4 (0.6%) | 13 (2%) |
Of these 655 patients, 272 were admitted to the NL ward and the rest to the IM ward. (Of the latter, 37 were seen by NL through a consult and 346 were never seen by NL.) According to diagnoses listed on patients’ discharge reports, the diagnosis established by the emergency department was modified in 203 patients (31%), and some even fell outside of the field of neurology (Table 1). Of the 488 patients diagnosed with stroke by the emergency department, only 369 retained that diagnosis upon discharge. Of 150 patients diagnosed as suffering something other than stroke, 17 listed a diagnosis of stroke in their discharge reports. While stroke was still the most common diagnosis in the discharge reports, it accounted for only 60.3% of the total diagnoses, 16.2% less than the figure given by emergency department admission reports. Regarding other diagnostic categories, diagnoses such as epilepsy, headache and meningitis were still frequent. There was an increase in diagnoses of syncope, mental disorders, and non-neurological diseases in patients who nonetheless had been admitted due to a suspected neurological disorder (Table 1). In 17 cases, complete information could not be obtained. This occurred in 4 cases due to lack of diagnosis at admission, and in 13 cases due to lack of diagnosis at discharge.
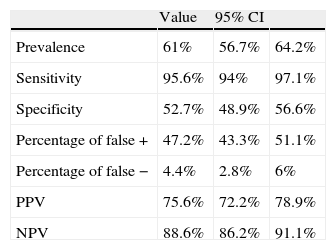
Although diagnosis of stroke by the emergency department showed very high sensitivity (95.6%), specificity was very low (52.7%). The probability of the emergency department's diagnosis of stroke being correct (PPV) was 75.6%. Therefore, 25% of patients diagnosed with stroke by the emergency department were not experiencing a stroke. The NPV was 88.6%, meaning that 11% of patients who were not initially diagnosed with stroke did in fact have a stroke (Table 2).
Reliability of stroke diagnosis in emergency departments.
| Value | 95% CI | ||
| Prevalence | 61% | 56.7% | 64.2% |
| Sensitivity | 95.6% | 94% | 97.1% |
| Specificity | 52.7% | 48.9% | 56.6% |
| Percentage of false + | 47.2% | 43.3% | 51.1% |
| Percentage of false − | 4.4% | 2.8% | 6% |
| PPV | 75.6% | 72.2% | 78.9% |
| NPV | 88.6% | 86.2% | 91.1% |
CI: confidence interval; NPV: negative predictive value; PPV: positive predictive value.
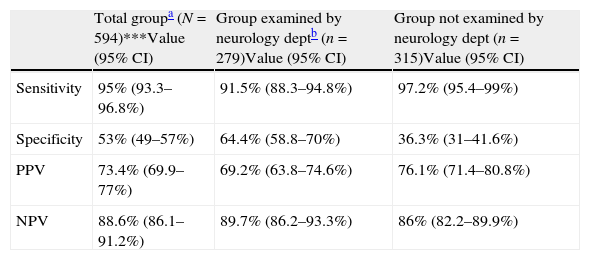
The PPV is even lower (73.4%) if we examine the validity of emergency department diagnoses of ischaemic stroke (excluding patients with ICH), and becomes lower still for the patient subgroup evaluated by NL during the hospital stay (69.2%) (Table 3).
Reliability of ischaemic stroke diagnosis in emergency departments.
| Total groupa (N=594)***Value (95% CI) | Group examined by neurology deptb (n=279)Value (95% CI) | Group not examined by neurology dept (n=315)Value (95% CI) | |
| Sensitivity | 95% (93.3–96.8%) | 91.5% (88.3–94.8%) | 97.2% (95.4–99%) |
| Specificity | 53% (49–57%) | 64.4% (58.8–70%) | 36.3% (31–41.6%) |
| PPV | 73.4% (69.9–77%) | 69.2% (63.8–74.6%) | 76.1% (71.4–80.8%) |
| NPV | 88.6% (86.1–91.2%) | 89.7% (86.2–93.3%) | 86% (82.2–89.9%) |
CI: confidence interval; NPV: negative predictive value; PPV: positive predictive value.
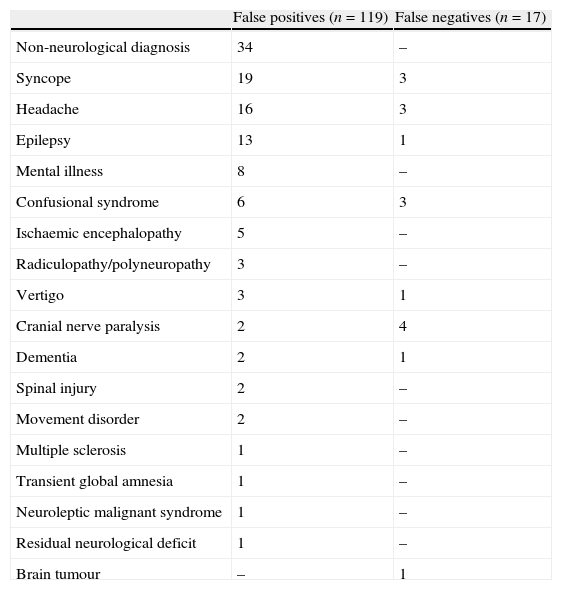
The definitive diagnoses at discharge for false positives and erroneous diagnoses at admission for false negatives are given in Table 4.
Definitive diagnoses at discharge for false positives and erroneous diagnoses at admission for false negatives.
| False positives (n=119) | False negatives (n=17) | |
| Non-neurological diagnosis | 34 | – |
| Syncope | 19 | 3 |
| Headache | 16 | 3 |
| Epilepsy | 13 | 1 |
| Mental illness | 8 | – |
| Confusional syndrome | 6 | 3 |
| Ischaemic encephalopathy | 5 | – |
| Radiculopathy/polyneuropathy | 3 | – |
| Vertigo | 3 | 1 |
| Cranial nerve paralysis | 2 | 4 |
| Dementia | 2 | 1 |
| Spinal injury | 2 | – |
| Movement disorder | 2 | – |
| Multiple sclerosis | 1 | – |
| Transient global amnesia | 1 | – |
| Neuroleptic malignant syndrome | 1 | – |
| Residual neurological deficit | 1 | – |
| Brain tumour | – | 1 |
There is no question that the most frequent neurological illness among cases admitted to the hospital is stroke. In our series, stroke cases account for 60.3% of the total neurological diagnoses upon admission to the HIE, and most were listed as ischaemic stroke.
The NINDS study showed that rtPA treatment for ischaemic stroke increases the number of patients with minimal to no disability by 12%, although it does not significantly lower mortality.3 Information on results from patients treated in a non-clinical trial setting normally comes from hospitals with experience in administering rtPA which consider the drug to be safe.10–12 However, if fibrinolysis is used incorrectly, it can increase mortality and morbidity instead of providing beneficial effects.13 Two studies performed in 137 random hospitals14 and 29 hospitals within the same region in Cleveland (Ohio, USA)4 showed that using rtPA in routine clinical practice increased patient mortality. Similar results have been found in a regional network of stroke records from 104 German hospitals. A study showed that thrombolytic treatment in hospitals with limited experience with those agents tripled the risk of in-hospital mortality (24% vs 8.6%).15 The differences in results found for experienced hospitals and those with limited experience with rtPA is probably due to the differences in fibrinolysis protocol violation rates (in some studies, as many as 50% of patients receiving rtPA were not treated according to treatment guidelines).4,7,16,17 This was observed in the Cleveland study, which showed that introduction of thrombolysis in general hospitals, with frequent protocol violations, produced very high rates of ICH (15.7%) and significantly higher mortality rates among patients treated with rtPA (15.7% vs 5.1%).4,18
Protocol violations are much more common when rtPA is prescribed by emergency department doctors than when it is prescribed by neurologists (30% vs 5%).19 In fact, fibrinolytic treatments performed in the emergency department of one local hospital included protocol violations in 32% of all cases, and 10% of the affected patients had symptomatic ICH.20 A study of 10880 stroke patients in 29 hospitals in the United States showed that centres restricting prescription of rtPA to neurologists alone had the lowest in-hospital mortality rates.21 This could be due to stricter adherence to treatment guidelines. Similarly, the German study group for stroke records found the best result from fibrinolysis treatment in hospitals containing a neurology department and stroke unit.15
The first step toward evaluating clinical criteria on the fibrinolysis protocol is diagnosing stroke correctly. In this study, we have shown that the emergency department diagnosis is a very sensitive test; few patients suffering from stroke are not identified as such. The 4.4% of false negatives is relevant, since these patients were unable to benefit from fibrinolytic treatment and other specific treatments for acute stroke. Nevertheless, in the specific case of employing fibrinolytic treatment that entails a risk of intracranial haemorrhage, it is crucial that patients be identified properly so that only patients experiencing a stroke will be treated. This is why it is so important for the emergency department diagnosis to have a very high PPV, meaning accurate positive identification of all patients experiencing a stroke. In our analysis, we show that in one local hospital in Andalusia, 24.4% of patients diagnosed with stroke by the emergency department were later found not to have suffered a stroke. If we exclude the group of patients with ICH, who did not receive fibrinolytic treatment, we find that the percentage of patients erroneously diagnosed with ictus in the emergency department rises to 26.6%. If we reduce the group to include only those patients evaluated by a neurologist during the stay, the percentage rises to 30.8%. The increased percentage of error may reside in two factors: on the one hand, ICHs are easy to detect in CT scans, unlike acute ischaemic strokes, and on the other, better evaluation of the patient by NL may result in stroke diagnoses established by emergency departments being modified in a higher percentage of patients. Therefore, if fibrinolytic treatment had been administered based on the emergency department diagnosis, we would have exposed a high number of patients erroneously diagnosed with stroke to an unjustified risk of cerebral haemorrhage. This risk virtually erases the benefits of disability reduction in patients diagnosed correctly. Its presence raises serious ethical questions with regard to allowing the treatment to be administered under such conditions in local hospitals in Andalusia.
We cannot extrapolate these results to other local hospitals in Spain. However, it is reasonable to believe that results would be no better in the 14 out of 17 local hospitals in which there is no contact with the speciality of neurology. Identification of stroke in the HIE emergency department may have improved in recent years, since a neurologist is now present at the hospital. In any case, this would demonstrate the added value of the speciality in local hospitals in Andalusia.
In conclusion, making fibrinolytic treatment available to all is not enough. On the most basic level, it is necessary for treatment to be administered safely. This fact is what requires us to create the necessary measures so that the treatment can be administered to all, safely, in centres with SUs and on-call NL specialists. These requirements are set forth by both PASI6 and the SNS stroke care strategy.8 One alternative for health districts whose geography prevents the rapid transfer of patients to a hospital with a SU would be developing a telemedicine system, although such a system would not be a substitute for the standard of care provided in specialised hospitals.7
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez Fernández E, et al. Fiabilidad del diagnóstico de ictus en urgencias. Neurología. 2012;27:284–9.