Cavernous angiomas or haemangiomas, also known as cavernomas, are non-cancerous vascular lesions. Anatomical pathology studies show that they are made up of sinusoidal capillaries of different diameters with an endothelial lining, in addition to elastic fibres in which perivascular fibrosis is observed. These elements are enclosed within a connective tissue capsule.1–3 Cavernous angiomas are dynamic lesions that normally increase in size over time. Growth is mainly due to 2 processes: thrombosis of the capillaries themselves, or bleeding at the lesion.
It is estimated that up to 12% of all vascular alterations of the spinal cord are caused by cavernous angiomas or cavernomas. They are mainly located on vertebral bodies and they occasionally reach epidural regions. They can be found in the intradural extramedullary space or they may be limited to an intramedullary location. Cavernous angiomas account for 4% of the lesions located in the epidural space, with the most common manifestation being extension into that space from the vertebral body.1–3
An exclusively epidural location is rare. This study presents 2 cases of spinal epidural cavernous angiomas with different radiological presentations. This made presurgical diagnosis more difficult.
Our patients, both women, were aged 31 years (case 1) and 58 years (case 2) and had similar clinical courses: progressive back pain developing for several years, localised by the patient at the midline (apophyseal joint pain upon examination). Pain intensity increased with movement, which prevented patients from performing daily activities. The 58-year-old patient had a personal history of hypothyroidism and several vertebral fractures secondary to osteoporosis. Results from the neurological examination were completely normal in both cases.
Radiology studies showed kyphosis in both patients and old compression fractures of the vertebrae (from T8 to T10) in case 2.
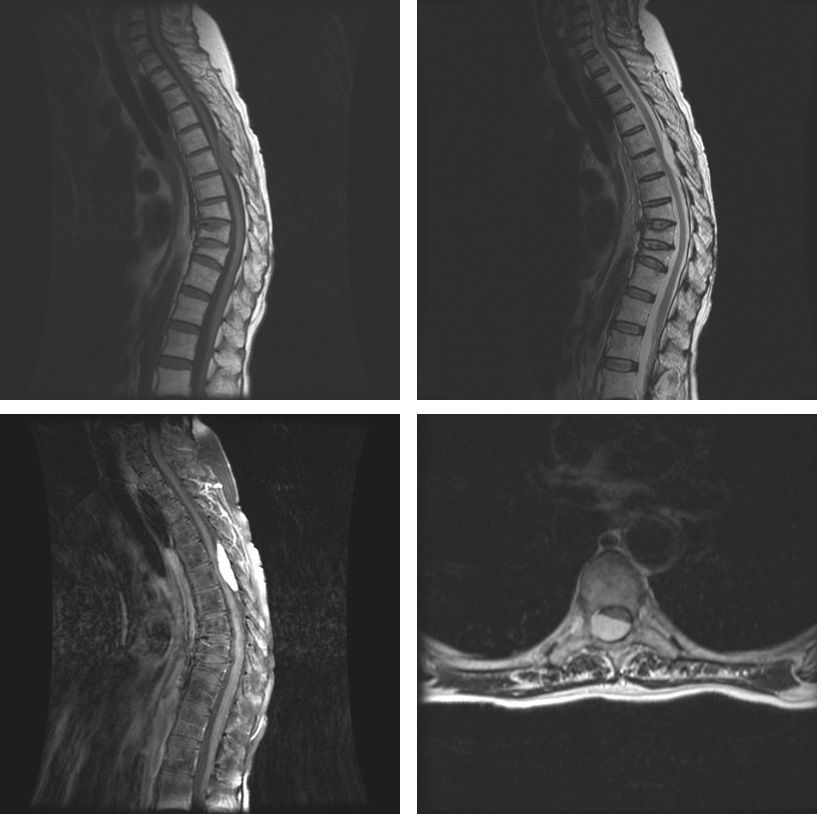
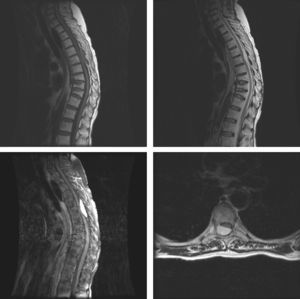
Magnetic resonance imaging (MRI) scans showed different findings in the two patients. In case 1, MRI scan showed a nodule in the posterior epidural space measuring 1.7×0.6cm in diameter. It was located on the T5 vertebral body and exerted no obvious compression on the spinal cord. The lesion was hypointense in the T1-weighted image and hyperintense in the T2-weighted image, with no enhancement when intravenous contrast was administered (Fig. 1). The lesion in case 2 was located in the posterior extradural space and measured 4.5×2.2cm in diameter, extending from T5 to T7. It was compressing the spinal cord. Unlike in case 1, this lesion was isointense in the T1-weighted image, hyperintense in the T2-weighted image, and showed intense enhancement after intravenous administration of contrast (Fig. 2).
Upper left: sagittal section, T1-weighted MRI image showing isointense epidural lesion affecting various levels. Osteoporotic fractures of 3 vertebral bodies. Centre: hypointense lesion on T2-weighted MRI image (sagittal section). Lower left: MRI image confirms contrast uptake (sagittal section). Lower right: Axial section, T1-weighted MRI image with contrast uptake showing spinal compression caused by the cavernous angioma.
Both patients underwent surgical resection of their lesions; the main objective was completing a histological study. In case 2, surgery was also indicated because the lesion was causing spinal cord compression. After marking under fluoroscopic guidance, dorsal laminectomy was employed as the surgical technique. These 2 lesions were very similar macroscopically; both were exclusively located in the epidural space and closely adherent to the dura mater. They were nodular in appearance, dark-coloured, and highly vascularised. While both exhibited significant intraoperative bleeding, blood transfusions were not necessary. In case 2, the lesion had invaded the right intervertebral foramen slightly at T6–T7, without widening it or causing extraforaminal protrusion.
Anatomical pathology results were compatible with cavernous haemangioma or angioma in both cases.
Patients remained neurologically asymptomatic after surgery and their progress has been satisfactory.
Cavernous angiomas or haemangiomas, also known as cavernomas, are non-cancerous vascular lesions that may be found at many locations. However, radiological manifestations of extra-axial or durally attached cavernous angiomas or haemangiomas, and specifically extradural spinal haemangiomas, differ significantly from intraparenchymal or intra-axial cavernomas in that they mimic tumours.4 In the epidural vertebral space, cavernous haemangiomas appear as homogeneous lesions (with no haemorrhages and therefore lacking the haemosiderin deposits that give rise to ‘popcorn-like’ images or the perilesional halo of intraparenchymal cavernomas). They are well-circumscribed, either hypointense or isointense in T1-weighted images and hyperintense in T2-weighted images, and display contrast enhancement. This has been observed in the largest patient series in the literature, including the 5 cases reported by Talacchi et al.,5 the 5-patient series by Shin et al.,6 and the 6 cases documented by Feng et al.7 This was also true for case 2. Nevertheless, the epidural cavernoma in patient 1 did not show gadolinium uptake, which made it difficult to establish a working presurgical diagnosis. This is in fact the second case of epidural spinal cavernous angioma displaying no contrast uptake to be reported in the international literature. The first case was described in 2007 by Lee et al.,8 who reported that only one of their 14 patients presented epidural spinal haemangioma with no gadolinium uptake.
After ruling out technical problems with the contrast injection, as in case 1, we cannot explain the difference in behaviour between these examples of epidural spinal cavernomas. We could not find any histopathological differences between the 2 cases that could provide a rationale for these disparate radiological findings.
Regarding clinical presentation and the treatment approach for this entity, we should highlight the following considerations. Clinical presentation of back pain or apophyseal joint pain pinpointed by the patient is not exclusive to this type of lesion; it can also be a sign of any epidural lesion stimulating nociceptors due to increased spinal pressure as a result of mass effect. This is also the case for skull haemangiomas. Surgical treatment of these lesions is indicated for two reasons: true cord compression, as in case 2, or to complete a histological study to determine the diagnosis of the lesion, as in case 1.
Differential diagnosis of this entity should consider other epidural tumours, such as lymphomas, metastatic tumours, meningiomas, or neurinomas-neurofibromas. Another entity that should be considered is epidural angiolipoma, a lipoma with a significant vascular component. An MRI scan with fat suppression sequences should therefore be performed in order to rule out this tumour type.2,3,9
Lastly and according to the findings from our study, we highlight that cavernous angioma must always be considered in the differential diagnosis of epidural spinal lesions, whether or not they display contrast uptake in the imaging studies.
Please cite this article as: Rodríguez-Boto G, Rivero-Garvía M, Gutiérrez-González R, Pérez-Zamarrón A, Vaquero J. Angiomas cavernosos epidurales espinales. Neurología. 2014;29:443–445.