SUNCT (short-lasting unilateral neuralgiform headache attack with conjunctival injection and tearing) syndrome was first defined by Sjaastad et al. in 1978.1 Since then, several studies on this topic have been published.2,3 The International Classification of Headache Disorders currently places it in the trigeminal autonomic cephalalgias subgroup.4 Although it is considered a primary headache in most cases, other cases are secondary to structural abnormalities in the posterior fossa, and especially in the hypophyseal region.5,6 More controversial is whether or not pharmacological agents may trigger this entity. For example, dopaminergic agents may exert a bidirectional influence. We describe one case of SUNCT syndrome secondary to consumption of ergoline dopamine agonist in a patient with hyperprolactinemia due to pituitary microadenoma.
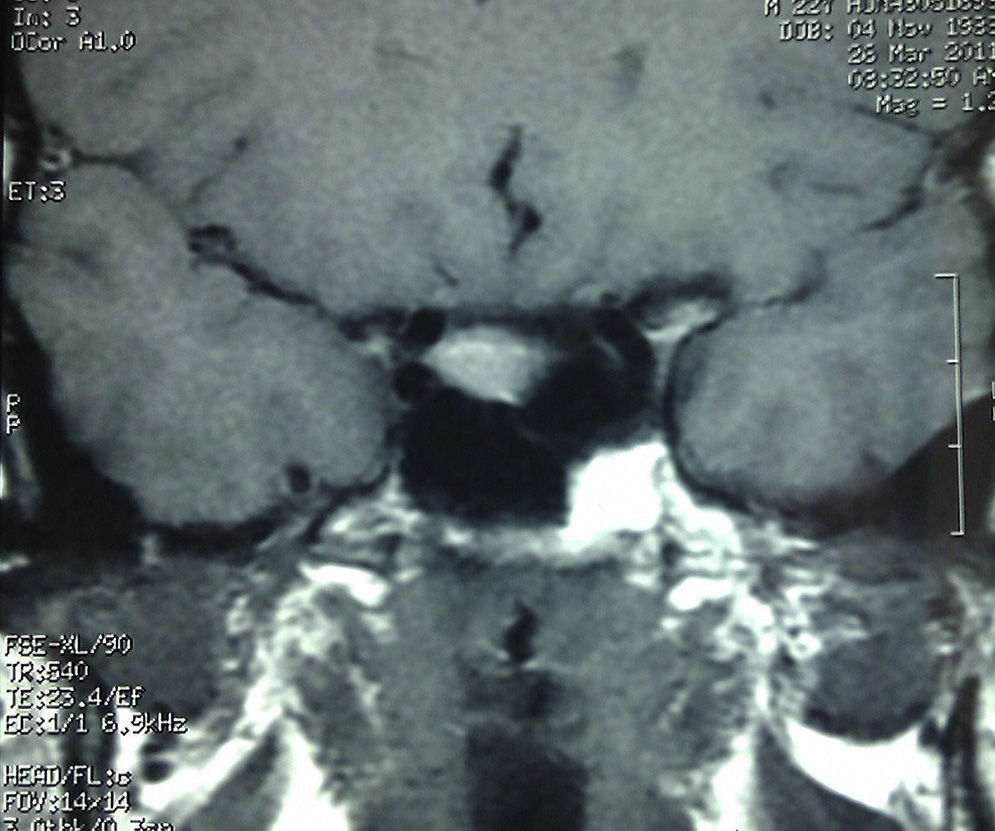
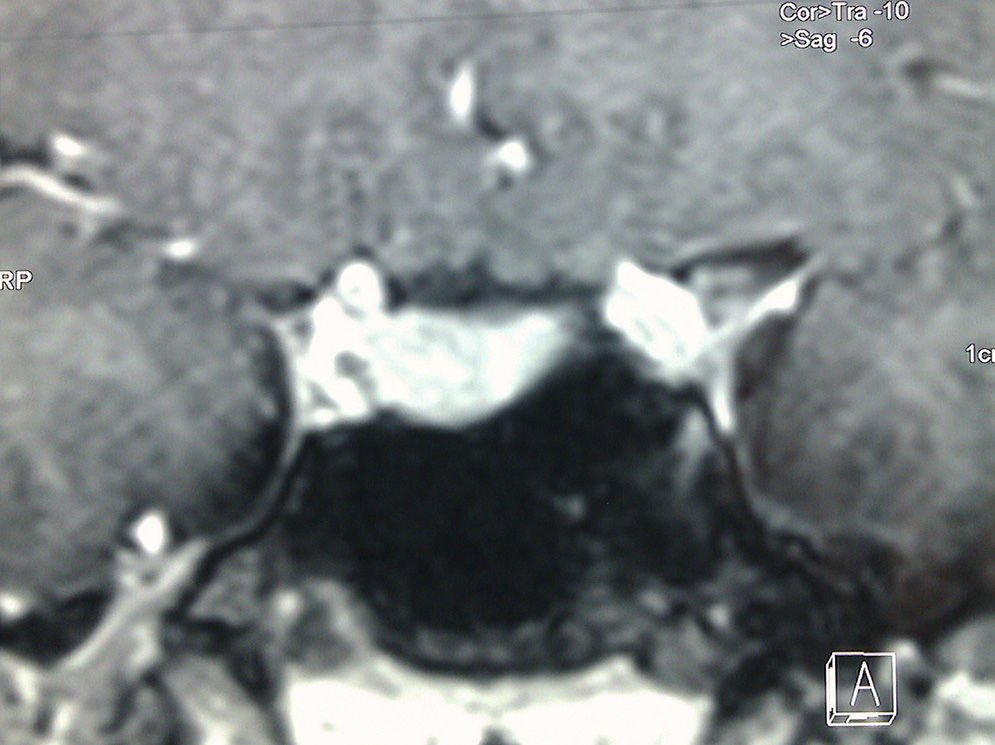
Our patient was a 24-year-old man with a diagnosis of hyperprolactinemia secondary to right-sided pituitary microprolactinoma without cavernous sinus invasion. The patient was in treatment with cabergoline. After treatment onset, he experienced intense and pulsatile headache episodes. Pain was located in the right periorbital region and accompanied by conjunctival injection, tearing, and ipsilateral rhinorrhoea. Episodes lasted no more than 3minutes, but they progressively grew more frequent until the patient was experiencing episodes every 30minutes daily. Headache met criteria for SUNCT syndrome. Doctors suspended treatment with cabergoline and began lamotrigine dosed at 50mg/12h. A new MRI revealed a pituitary microadenoma with no changes with respect to a previous MRI (Figs. 1 and 2). Fifteen days after changing treatment, the patient showed clear signs of improvement; by 3 months, he had fewer than 5 episodes per month. Since prolactin levels remained high, doctors began treatment with quinagolide (non-ergoline dopaminergic agent); this reverted prolactin levels to normal but did not exacerbate the headaches.
The literature describes patients with SUNCT syndrome with pituitary micro or macroadenomas, both functional and non-functional.7–12 Although the pathophysiological relationship has yet to be fully established, the most plausible hypothesis for most authors is possible mechanical excitation of the trigeminal nerve due to a local compressive effect at the level of the cavernous sinus. However, this does not explain how microadenomas would cause this syndrome. Another hypothesis points to the potential neurohumoral alteration caused by these tumours. In line with this hypothesis, there are published descriptions of cases of exacerbation or onset of SUNCT after starting treatment with dopaminergic agonists,9–12 as in the case we present in this article. However, there are also cases in which starting treatment improved a prior SUNCT-type headache.7 Therefore, both effects are possible, but the pathophysiological mechanisms are unknown in both situations. In our case, the time between treatment onset and pain onset, the absence of prior symptoms of SUNCT syndrome despite presence of microprolactinoma, absence of clinical and radiological changes in the underlying pituitary disease, and resolution of pain after discontinuing the drug all support the idea that the ergoline-dopaminergic agonist is an important triggering factor for headache. Starting treatment with another agonist did not result in exacerbation of the headache for reasons that remain unclear, but this could be due to the non-ergoline nature of the second drug. This situation is also described in one published case.9
Therefore, and despite the neurophysiological questions that remain unanswered, awareness of these cases of secondary SUNCT syndrome is important. Doctors should also consider any intercurrent medications that could significantly promote the development of headache, as in our case.
Please cite this article as: Pulido Fontes L, Mayor Gómez S. Cefalea tipo SUNCT (Short-lasting unilateral neuralgiform headache attack with conjuntival injection and tearing) asociada a lesión hipofisaria. Neurología. 2015;30:458–459.
Presented as poster format in the headache section at the 64th Annual Meeting of the Spanish Society of Neurology.