Membranous interventricular septal aneurysms are rare congenital heart defects associated with increased risk of embolic stroke. However, this association cannot be clearly established due to the low incidence of this type of aneurysm.
We present the case of a 66-year-old man who was referred to our department due to left thalamic stroke presenting with instability, poor coordination, and language alterations; symptoms lasted 5hours and improved progressively, with the patient presenting no sequelae. The patient reported history of heart disease (although no medical records were available) and no other relevant history. Physical examination revealed systolic murmur at the left sternal border and systolic and diastolic murmurs in the aortic area. An electrocardiography study displayed sinus rhythm with right bundle branch block and left anterior fascicular block.
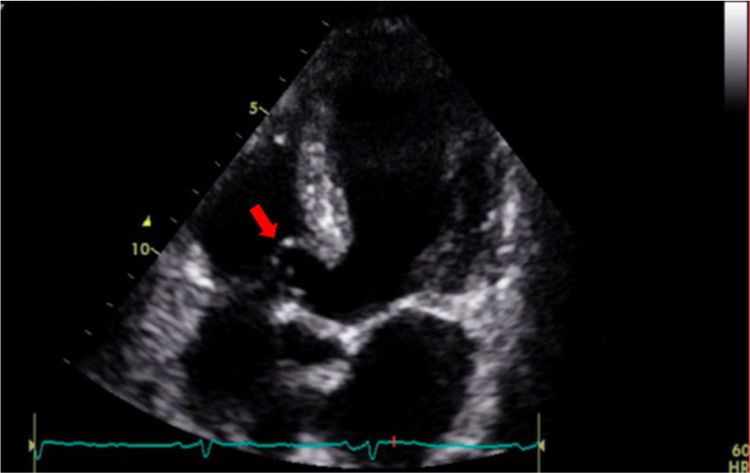
Brain MRI revealed no alterations. We performed several screening tests, including an ultrasound study of the supra-aortic trunks, a study of hypercoagulability disorders (protein C or protein S deficiency, antithrombin III, factor V Leiden, prothrombin G20210A, lupus anticoagulant, and anticardiolipin antibodies), an echocardiogram, and Holter monitoring to rule out any arrhythmia with high embolic potential, such as atrial fibrillation. All tests yielded normal results, with the exception of transthoracic echocardiogram, which revealed an aneurysm in the membranous interventricular septum with perimembranous interventricular communication (Fig. 1), moderate aortic insufficiency, and mild left ventricular hypertrophy, with normal left ventricular global and segmental systolic function.
These findings were confirmed with a transoesophageal echocardiogram, which revealed an aneurysm protruding towards the right ventricular outflow tract and a perimembranous ventricular septal defect with left-to-right shunt. We did not detect any other possible causes of embolism, such as patent foramen ovale, interatrial septal aneurysm, thrombi in the left atrial appendage, or atherosclerotic plaques in the aortic arch.
In summary, our patient was a 66-year-old man with stroke who did not present atrial fibrillation, patent foramen ovale, hypercoagulability disorders, or evidence of artery disease at other levels. As he presented few cardiovascular risk factors, we hypothesise that the pathogenic mechanism of stroke was a thrombus originating in the membranous interventricular septal aneurysm.
Membranous interventricular septal aneurysms are recognised as a possible cause of embolism.1 In the case presented here, embolism seems to have been the cause of thalamic stroke, which usually causes pure sensory or atypical lacunar syndromes.2
The incidence of this heart defect is estimated at 0.2%–3% in the general population.3 In most cases, the aneurysm is a benign, incidental finding,4 although it can cause aortic or tricuspid regurgitation, right ventricular outflow tract obstruction, infective endocarditis, aneurysm rupture, atrioventricular block, or thromboembolism.5 Individuals with asymptomatic membranous interventricular septal aneurysms should be followed up to detect any of these complications.6 Patients presenting unexplained embolic events should be thoroughly assessed to rule out presence of this rare heart defect.
Differential diagnosis of membranous interventricular septal aneurysms includes sinus of Valsalva aneurysms, abscesses, and ischaemic or traumatic aneurysms.7 Our patient's clinical history, the absence of infection and history of surgery or myocardial infarction, and the location of the aneurysm suggest that this heart defect was caused by spontaneous partial closure of the interventricular communication; this is in fact the most frequent cause of membranous interventricular septal aneurysms.
Treatment options for patients with stroke include surgical excision and repair of the aneurysm and anticoagulant treatment. Less frequently, patients may benefit from percutaneous closure, although this technique is more challenging when applied to membranous interventricular septal aneurysms than to other types of heart defects.8 In our case, we informed the patient about the possible management strategies; as he was unwilling to undergo surgery, we started anticoagulation with acenocoumarol. After 3 years of follow-up, the patient has presented no further embolic events or complications.
Membranous interventricular septal aneurysms, though rare, may potentially cause severe complications. Given that the most appropriate management strategy in these patients is yet to be established, we deemed it interesting to report this case of satisfactory progression with conservative treatment.
Please cite this article as: Alcón Durán B, Hernández-Jiménez V, Alcocer Ayuga M, Saavedra Falero J. Infarto talámico en un paciente con aneurisma del septo interventricular. Neurología. 2020;35:509–510.