In patients with supratentorial lesions, gaze deviation is usually directed toward the side of the lesion. In exceptional cases, gaze deviates to the contralateral side, in which case it is known as wrong-way deviation.1 Although rare, association between wrong-way deviation and thalamic haemorrhagic stroke is well documented.2–4 However, association with thalamic ischaemic stroke has not previously been described.
We report a case of wrong-way deviation secondary to thalamic ischaemic stroke and analyse its potential relevance in understanding the mechanisms underlying this phenomenon.
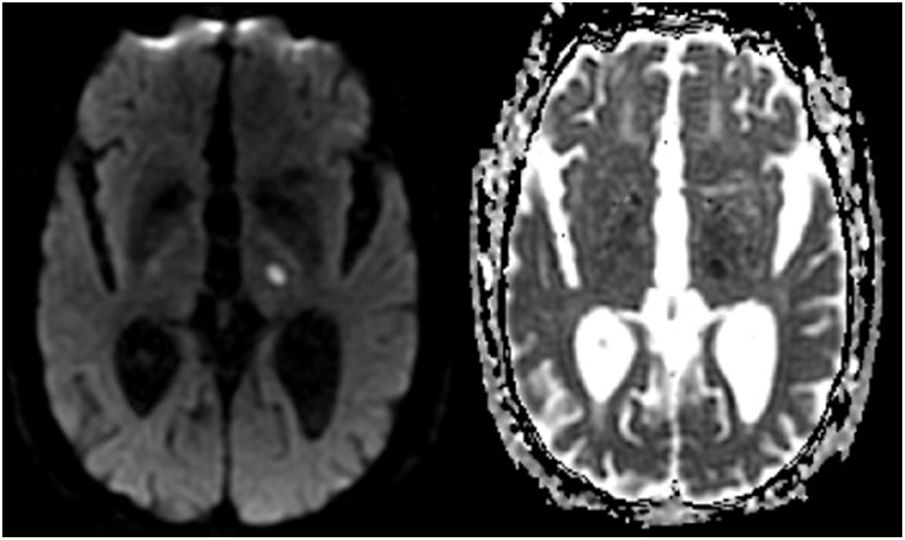
Our patient is an 87-year-old man with history of arterial hypertension, prostate cancer with local extension under conservative treatment, and questionable non-motor focal seizures treated with levetiracetam. These seizures, only witnessed by his son, consisted of short episodes of disconnection and sucking motions. An EEG revealed no epileptiform activity and an MRI study only showed leukoaraiosis. He was admitted to our hospital following code stroke activation due to sensory alteration of the right limbs upon awakening. The medical history interview revealed no data suggesting seizures. Examination revealed an excellent level of consciousness and attention, multimodal hypoaesthesia in the right limbs, and gaze deviation to the right manifesting as jerk nystagmus to the left, which was more pronounced when looking leftward. Corrective saccades to the left were observed during smooth pursuit movements in both directions. Results of the electrocardiogram and laboratory analysis performed at admission were normal. The baseline CT study yielded normal results; a CT angiography revealed stenosis of the left posterior cerebral artery. An MRI study (Fig. 1) revealed acute ischaemic stroke in the left thalamus. The hospital stay was uneventful, and the described focal symptoms persisted at discharge.
In 1979, Sharpe et al.5 described similar neuro-ophthalmological alterations to those of our patient in individuals undergoing surgical decortication due to epilepsy. They postulated that the alterations may be explained by asymmetric tone in the smooth pursuit pathways, which would cause a deviation contralateral to the lesion on the horizontal plane. This would lead to corrective saccades, always towards the affected side, during smooth pursuit movements, both in leftward and rightward gaze. Furthermore, as long as patients tried to maintain a fixed gaze, they presented jerk nystagmus, also towards the side of the lesion.5
In 1984, Brigell et al.6 published a case of right thalamic ischaemic stroke with similar neuro-ophthalmological findings to those of our patient and those reported by Sharpe et al.5 Their patient presented impaired smooth pursuit with corrective saccades ipsilateral to the lesion. The authors, in line with the theory of Sharpe et al.,5 suggested involvement of the transthalamic segment of the smooth pursuit pathway, which projects to the thalamic dorsal medial nucleus.6 As shown in the MRI study (Fig. 1), lesion location in our patient is compatible with that considered to be the thalamic dorsal medial nucleus.
Since then, participation of the thalamus in controlling eye movements, and more specifically smooth pursuit, has been well studied in animal models, with the work of Tanaka7 being particularly relevant. Furthermore, asymmetric tone of the smooth pursuit pathways has also successfully been proposed as an explanation for oculomotor alterations with similar characteristics, such as downbeat nystagmus.8
We should underscore that in the published cases of wrong-way deviation due to thalamic haematoma, associated nystagmus has not been reported. This is unsurprising, given the low level of consciousness frequently present in these patients and the subsequent lack of saccadic movements. Furthermore, the underlying mechanisms are probably different: compression of the oculomotor pathways in the rostral brainstem due to the mass effect of the haemorrhage.9
It has also suggested that wrong-way deviation may be an irritative phenomenon, as supported by experience with animal models10 and deep brain stimulation on the thalamus of epileptic patients.11 Despite the unclear history of our patient, the clinical symptoms and neuroimaging findings make this mechanism implausible.
In conclusion, wrong-way deviation is also possible in the event of thalamic ischaemic lesions. Our case, like those described by Sharpe et al.5 and Brigell et al.,6 supports the hypothesis that this phenomenon may be caused by asymmetry in the smooth pursuit pathways. However, as reported by the literature, it seems reasonable to consider that the most plausible mechanism is different in other cases. Proper characterisation of the symptoms caused by lesions to the human nervous system may be important in better understanding their functioning.
Please cite this article as: San Pedro Murillo E, Rodríguez López A, Morales García E, Herrero San Martín A. «Wrong-way deviation» por ictus isquémico talámico: una nueva asociación. Neurología. 2021;36:479–480.