NEW DEVELOPMENTS IN HEADACHE AND INTRACRANIAL HYPERTE
Más datosMigraine affects more than 4.5 million people in Spain, resulting in a considerable socioeconomic impact. Although national and international guidelines have been published, the management of patients with migraine, especially those with chronic migraine, is inadequate.
Subjects and methodsWe conducted a survey among 40 primary care (PC) physicians in Spain as part of a European project involving 201 physicians from 5 countries.
ResultsMost participants issued diagnoses of episodic migraine and chronic migraine (93% vs 65%); 82.5% indicated that they did not refer these patients to specialists, and 100% of PC physicians stated that they were responsible for patient follow-up. The main tools used in PC for diagnosis and follow-up were clinical interviews, medical histories, and the patient diaries. Our data revealed that the treatments prescribed were not in accordance with the national and international guidelines. Participants who did not refer patients estimated that only 48% of patients received preventive treatment, and that the assessment of efficacy was based on patient perception. Seventy percent of respondents indicated a need for migraine training. Finally, 100% of participants considered that a guide for medical history taking and referral would be essential or useful for the management of migraine in PC.
ConclusionsThe survey results revealed a need for training and guidance in PC to improve the diagnosis and management of patients with migraine, particularly chronic migraine.
La migraña afecta a más de 4,5 millones de personas en España con el consiguiente impacto socioeconómico. A pesar de la existencia de guías nacionales e internacionales, el manejo del paciente migrañoso, especialmente con migraña crónica, es inadecuado.
Sujetos y métodosSe llevó a cabo una encuesta a 40 médicos de Atención Primaria (AP) de España dentro de un proyecto europeo que involucraba a 201 médicos de 5 países.
ResultadosLa mayoría de los participantes diagnostican migraña episódica y migraña crónica (93% vs. 65%). El 82,5% indicó que no derivaba a los pacientes al especialista y en el 100% de casos los médicos de AP declararon ser los encargados del seguimiento del paciente. Las principales herramientas usadas en AP para el diagnóstico y seguimiento son la entrevista clínica, la guía de anamnesis y el diario del paciente. Se observó que los tratamientos prescritos no están en concordancia con las guías nacionales ni internacionales. Los participantes que no derivan al paciente estiman que solo el 48% recibe tratamiento preventivo y que la valoración de la eficacia se hace mediante la percepción del paciente. El 70% indica una necesidad de formación en migraña. Finalmente, el 100% de los participantes consideran que una guía para la anamnesis y la derivación sería imprescindible o de utilidad para el manejo de la migraña en AP.
ConclusionesLos resultados de la encuesta muestran que hay una necesidad de formación y guía en AP para mejorar el diagnóstico y manejo del paciente con migraña, especialmente con migraña crónica.
Migraine is the main cause of recurrent headache worldwide,1 and affects more than 4.5 million people in Spain.2 With an estimated prevalence of 12%–15%, it is more frequently reported in women than in men (4:1),2–4 and constitutes the most frequent reason for consultation in Spanish neurology departments.5 Migraine has a significant impact on disability and quality of life,6 and causes a considerable socioeconomic burden, both in terms of use of healthcare resources7 and lost working days and productivity.8 Furthermore, in Spain, approximately one million people have chronic migraine,2 defined as headache manifesting at least 15 days per month for over 3 months.9,10 Chronic migraine causes a greater personal and socioeconomic burden than episodic migraine.11–13
According to the International Classification of Headache Disorders (ICHD) and the European Headache Federation (EHF), chronic migraine frequently requires the patient to be referred to a neurologist specialising in headache, due to the complexity of its management; however, episodic migraine can and should be managed in primary care (PC).9,14 The Clinical Practice Guidelines for Headache of the Spanish Society of Neurology (SEN) recommend referring patients from PC to the general neurology department if headache does not improve despite at least one therapeutic trial, as well as patients diagnosed with chronic migraine, among others. The referral criteria recommended by the SEN include, among others, headache not responding to standard treatment, medication overuse headache, and the need for special treatments.15 However, only 60% of neurologists in Spain believe that the diagnosis of migraine should be established by PC physicians, and 70.5% of patients with migraine attended at neurology consultations are referred by a PC physician.16 Furthermore, in a study conducted in Cantabria and Salamanca in 2010, of the 105 PC physicians surveyed, only 44% diagnosed migraine correctly, with more than half (56%) making mistakes in diagnosis and more than one-third reporting errors in treatment.17
Although chronic migraine requires preventive treatment, a study published in 2010 showed that less than 10% of patients consulting due to migraine received it (25%–50% would need it). Furthermore, only approximately 10% of patients receive triptans, the drug of choice to treat moderate-severe migraine attacks.5 In this regard, the Vancouver Declaration on Global Headache Patient Advocacy18 underscores the importance of providing all patients with headache with access to specialists trained in headache care, and considers the implementation of training programmes for headache specialists as a priority.
All this suggests a need to reinforce the diagnosis and basic management of migraine and training in headache in Spain.5 The My-LIFE anamnesis project sought to analyse the diagnosis and the follow-up of patients with migraine, especially chronic migraine, by PC physicians in Germany, France, Spain, Italy, and the United Kingdom. In this study, we analyse the data reported by Spanish participants in the European My-LIFE anamnesis project.19,20
Patients and methodsThe My-LIFE anamnesis project included an international online survey of PC physicians with experience in the treatment of headache, addressing their real practice and the needs for migraine history taking in PC settings. This project included PC physicians from 5 European countries: Germany, Spain, France, Italy, and the United Kingdom. A steering committee of 7 European migraine experts designed the survey based on their clinical experience, after a search of the relevant scientific literature. From this information, an initial survey was created and used in 3 simulated consultations with 2 neurologists and a PC physician, and 3 different patients previously diagnosed with chronic migraine by their regular doctor. The simulated consultations were used to identify limitations in communication during migraine history taking. In June 2019, 3 simulated consultations were held in Barcelona. The information obtained in these simulated consultations was used to develop the final version of the project survey. This final version was published on a restricted-access online platform, and 40 PC physicians were invited to complete it.
The Spanish version of the online survey may be consulted in the Supplementary material (Appendix). PC physicians were selected according to the following criteria: 1) ≥ 2 years of experience in PC; 2) seeing ≥ 5 patients with headache disorders per week; 3) regularly taking medical history of their patients with headache disorders; 4) currently having ≥ 1 patient suffering from migraine under acute or preventive treatment. Previous articles provide a detailed description of the study design, the development and distribution of the survey, and the processing and statistical analysis of the data.19,20
ResultsSimulated consultationsOf the 3 simulated consultations, neurologists participated in 2 and a PC physician in one. Neurologists considered that a guide for migraine history taking would be useful for the identification and management of chronic migraine in PC. The PC physician considered it relevant to include red flags for secondary headache. Patients considered the use of a headache diary very useful, as it helped them to better describe their experience with migraine, its frequency, and impact on daily living. Both physicians and patients mentioned the complexity of differentiating between tension-type headache, chronic migraine, and symptomatic medication overuse headache.
Profile of participantsThe participants in the My-LIFE anamnesis project were 201 PC physicians from 5 European countries (Germany, Spain, France, Italy, and the United Kingdom), 40 of whom were from Spain. The general profile of the Spanish participants did not significantly differ from that of the rest of the sample. The PC physicians participating in the study had a mean of 25 years of experience (range, 12–35), and attended a mean of 189 patients per week, 12.5% of whom presented headache. Of these, 37% presented migraine: 68% episodic migraine and 32% chronic migraine.
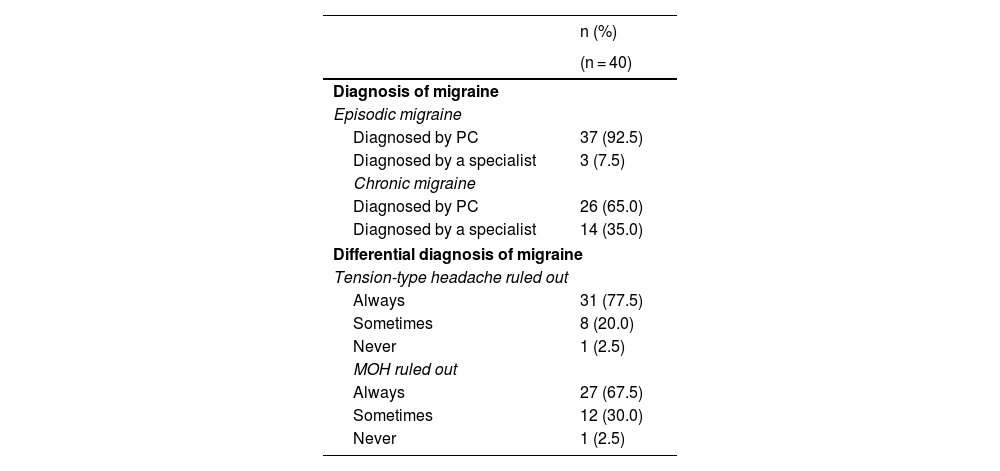
Clinical practice of participantsNinety-three percent of participants reported that they diagnosed episodic migraine without referring the patients; however, this percentage decreased to 65% in the case of chronic migraine (Table 1). Of the participants in Spain, 78% answered that they always ruled out tension-type headache, and 68% always ruled out medication overuse headache during history taking (Table 1).
Diagnosis of chronic and episodic migraine in Spain.
| n (%) | |
|---|---|
| (n = 40) | |
| Diagnosis of migraine | |
| Episodic migraine | |
| Diagnosed by PC | 37 (92.5) |
| Diagnosed by a specialist | 3 (7.5) |
| Chronic migraine | |
| Diagnosed by PC | 26 (65.0) |
| Diagnosed by a specialist | 14 (35.0) |
| Differential diagnosis of migraine | |
| Tension-type headache ruled out | |
| Always | 31 (77.5) |
| Sometimes | 8 (20.0) |
| Never | 1 (2.5) |
| MOH ruled out | |
| Always | 27 (67.5) |
| Sometimes | 12 (30.0) |
| Never | 1 (2.5) |
MOH: medication overuse headache; PC: primary care.
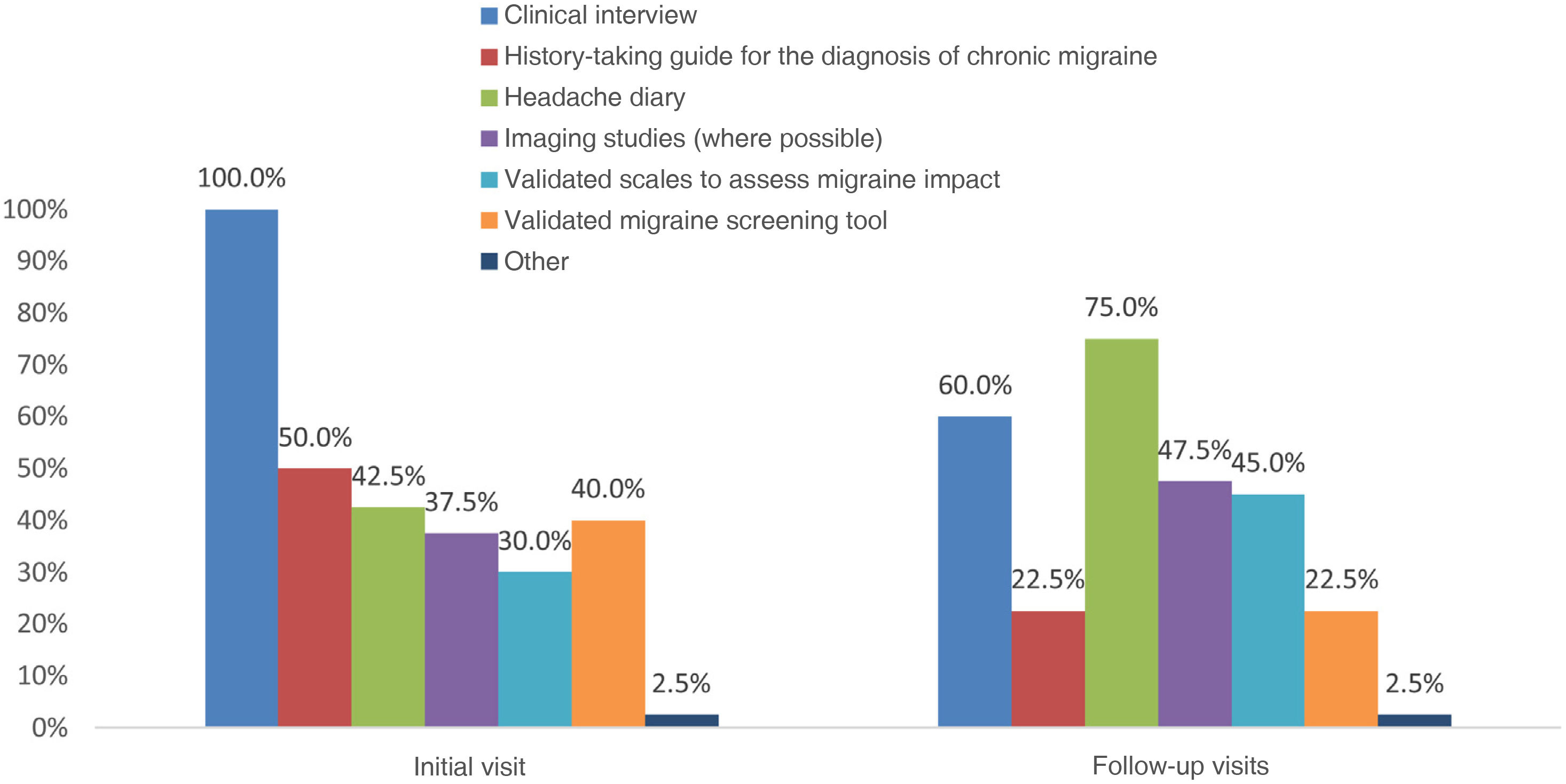
Regarding PC assessment of patients with chronic or disabling migraine, all participants reported that they conducted a clinical interview during the first visit, but only 50% used a guide for migraine history taking (Fig. 1). Of the participants that did use a guide, 54% reported that it was a validated and published document, and in 89% of cases, it mentioned red flags.
The tools used during the first consultation with patients with chronic or disabling migraine were different from those used in follow-up visits (Fig. 1). Headache diaries were more frequently used in follow-up visits (75%) than in the first visit (42.5%). The main parameters recorded in diaries were the frequency and duration of attacks, and the medication used.
Forty-eight percent of participants requested imaging studies during follow-up; the main reason for these studies was to rule out secondary headaches (69%). Regarding the use of validated scales, the most widely used were the D-Migraine (57.7%) and ID-Chronic Migraine scales (38.5%) in the initial visit, and the HURT scale (46.2%) in follow-up visits. The remaining scales were used by less than 50% of participants; up to 27% of respondents did not use any of the scales mentioned in the survey (Fig. 2).
Of all PC physicians, 82.5% reported that they usually or always treated patients with chronic migraine and only 17.5% referred them to a specialist (5% always and 12.5% usually). The main reason for specialist referral after the diagnosis of chronic or disabling migraine was to rule out secondary headaches (57%) or for prescription of preventive treatment (57%).
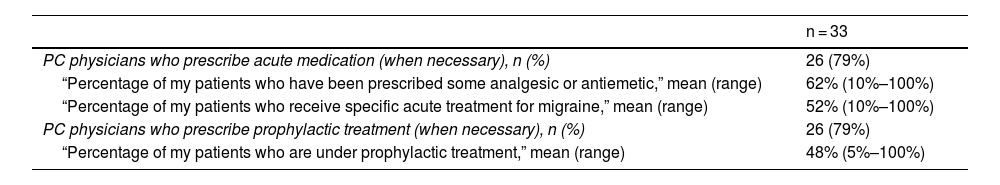
Of the PC physicians who treated chronic migraine without referring the patient, 79% prescribed symptomatic treatments and the same percentage prescribed preventive treatments, when necessary. These participants estimated that 62% of their patients with chronic migraine received analgesics or antiemetics, and 52% specific acute antimigraine drugs. Respondents also estimated that 48% of their patients with chronic migraine received preventive treatment prescribed by PC (Table 2).
Prescription patterns of PC physicians who do not refer patients with chronic migraine.
| n = 33 | |
|---|---|
| PC physicians who prescribe acute medication (when necessary), n (%) | 26 (79%) |
| “Percentage of my patients who have been prescribed some analgesic or antiemetic,” mean (range) | 62% (10%–100%) |
| “Percentage of my patients who receive specific acute treatment for migraine,” mean (range) | 52% (10%–100%) |
| PC physicians who prescribe prophylactic treatment (when necessary), n (%) | 26 (79%) |
| “Percentage of my patients who are under prophylactic treatment,” mean (range) | 48% (5%–100%) |
PC: primary care.
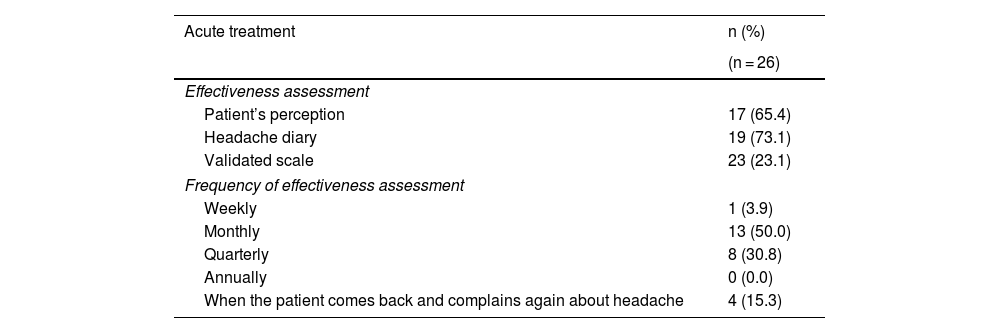
All survey participants reported that they were responsible for the follow-up of patients with chronic or disabling migraine, regardless of whether the diagnosis was established by a specialist or a PC physician. PC physicians mainly evaluated the effectiveness of the acute treatment prescribed on a monthly basis (50%), using headache diaries (73%) and patient perception (65%) (Table 3). Regarding preventive treatment, effectiveness was mainly assessed on a monthly basis (50%), using patient perception (73%) and headache diaries (62%) (Table 3). In Spain, PC physicians assessed the treatment prescribed by headache specialists using headache diaries (86%) and, to a lesser extent, patient perception (57%), with variable frequency.
Assessment of the effectiveness of treatment in patients who are not referred and are treated by PC physicians.
| Acute treatment | n (%) |
|---|---|
| (n = 26) | |
| Effectiveness assessment | |
| Patient’s perception | 17 (65.4) |
| Headache diary | 19 (73.1) |
| Validated scale | 23 (23.1) |
| Frequency of effectiveness assessment | |
| Weekly | 1 (3.9) |
| Monthly | 13 (50.0) |
| Quarterly | 8 (30.8) |
| Annually | 0 (0.0) |
| When the patient comes back and complains again about headache | 4 (15.3) |
| Prophylactic treatment | n (%) |
|---|---|
| (n = 26) | |
| Effectiveness assessment | |
| Patient’s perception | 19 (73.1) |
| Headache diary | 16 (61.5) |
| Validated scale | 6 (23.1) |
| Frequency of effectiveness assessment | |
| Weekly | 0 (0.0) |
| Monthly | 13 (50.0) |
| Quarterly | 9 (34.6) |
| Annually | 0 (0.0) |
| When the patient comes back and complains again about headache | 4 (15.4) |
The main reasons reported for referral to a specialist during follow-up were ineffectiveness of the prescribed acute treatment (82.5%), ineffectiveness of preventive treatment (72.5%), highly disabling migraine (72.5%), and diagnostic uncertainty (67.5%). Only 30% of participants referred patients with migraine with aura and 37.5% referred patients with suspected chronic migraine.
Creation of a guide for migraine history takingAlthough PC physicians are the main agents responsible for the diagnosis and follow-up of patients with migraine, only 10% of participants considered they had sufficient training on the management of patients with chronic migraine, and 30% reported a lack of training.
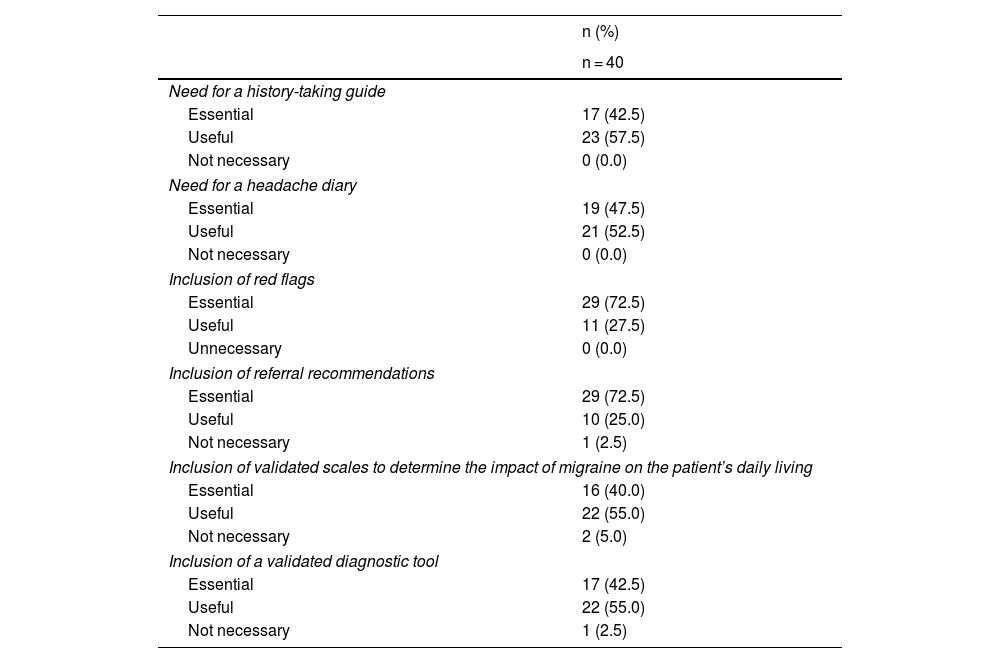
Participants considered having a guide for migraine history taking and referral to be essential (42.5%) or useful (57.5%) for the management of patients with chronic migraine (Table 4). The main subjects suggested for inclusion in the guide were pain characteristics (onset, intensity, localisation, duration, quality, etc.) (97.5%), associated symptoms (nausea, photophobia, phonophobia, osmophobia) (97.5%), frequency of attacks (92.5%), and factors predisposing to migraine (92.5%). Furthermore, participants considered that such a guide should include red flags (essential for 72.5% of participants and useful for the remaining 27.5%) and recommendations for referral (essential for 72.5% and useful for 25%) (Table 4). Most participants also considered it useful to include validated scales to assess the impact of migraine on the patient’s daily living (Table 4).
Opinions of PC physicians on the need for a migraine history-taking guide and a headache diary in chronic migraine.
| n (%) | |
|---|---|
| n = 40 | |
| Need for a history-taking guide | |
| Essential | 17 (42.5) |
| Useful | 23 (57.5) |
| Not necessary | 0 (0.0) |
| Need for a headache diary | |
| Essential | 19 (47.5) |
| Useful | 21 (52.5) |
| Not necessary | 0 (0.0) |
| Inclusion of red flags | |
| Essential | 29 (72.5) |
| Useful | 11 (27.5) |
| Unnecessary | 0 (0.0) |
| Inclusion of referral recommendations | |
| Essential | 29 (72.5) |
| Useful | 10 (25.0) |
| Not necessary | 1 (2.5) |
| Inclusion of validated scales to determine the impact of migraine on the patient’s daily living | |
| Essential | 16 (40.0) |
| Useful | 22 (55.0) |
| Not necessary | 2 (5.0) |
| Inclusion of a validated diagnostic tool | |
| Essential | 17 (42.5) |
| Useful | 22 (55.0) |
| Not necessary | 1 (2.5) |
All participants considered headache diaries to be essential (47.5%) or useful (52.5%) for the management of patients with chronic migraine (Table 4). In the opinion of PC physicians in Spain, the main items to be included in the headache diary are migraine days (95%), duration of the migraine attack (92.5%), characteristics of migraine (92.5%), and medication used (92.5%).
Lastly, 40% of participants considered a checklist or brief descriptive document with recommendations on how to proceed to be the best formats for the history-taking guides. Only 20% of participants considered it necessary to create an extensive and detailed document.
DiscussionThe results of this online survey distributed among PC physicians provide an overview of the diagnosis and management of patients with chronic or disabling migraine in the Spanish PC setting. The main results suggest that, although we selected PC physicians interested in headaches, the diagnosis of chronic or disabling migraine in PC was insufficient, and their treatment was suboptimal; similar results were reported in the other countries participating in the survey.
According to national and international recommendations, a diagnosis of episodic and chronic migraine can be established in PC; however, patients with chronic migraine should be referred to specialists due to the complexity of their management.9,14,15 In this study, the great majority of PC physicians in Spain diagnosed patients with episodic migraine (93%), but only 65% diagnosed patients with chronic migraine. This rate of diagnosis in PC in Spain is similar to that observed in the 5 European countries previously analysed in this project (mean, 61%; ranging from 45% in Italy to 81% in France)19 and is consistent with the rate observed in a previous study conducted in Spain, in which only 60% of neurologists considered that diagnosis of migraine should be established by PC physicians.16
However, the rate of referral to specialists is low, and is not in line with the recommendations of the national and international guidelines9,14,15,21: only 17.5% of participants referred patients with chronic or disabling migraine to a specialist (5% always referred these patients and 12.5% frequently). Despite this low rate, Spain is the only participating country where any percentage of PC physicians reported they always refer these patients. In the remaining participating countries, no participant reported systematically referring patients.19,20 This group of PC physicians who always or frequently refer patients with migraine to specialists probably do this due to insufficient training, together with a system that tolerates high rates of referral. Furthermore, the rate of prescription of triptans in PC tends to be low, and no preventive treatments are usually prescribed.
Only 79% of participants in Spain prescribed preventive treatment to patients with chronic migraine, and only 48% of patients received this type of treatment. These data are much lower than those reported by PC physicians from the United Kingdom, where 94% prescribed preventive treatment and up to 64% of patients received this treatment.19,20 Preventive treatment of migraine aims to reduce the intensity, duration, and frequency of migraine attacks. Optimal treatment improves patients’ quality of life and reduces the risk of chronic transformation, consequently reducing disease-related disability.22 The data from this survey suggest that patients with chronic migraine are undertreated in Spain, as reported in previous studies,23–25 and that PC physicians still need training on how and when to start preventive treatments.22 In this regard, a survey of neurologists in Spain found that they considered that improvements should be made to the training of PC physicians on headache, especially regarding preventive treatment.5 Furthermore, undertreatment may be a consequence of the low rate of referral observed, as preventive treatments are infrequently prescribed by PC physicians in Spain, and some treatments must be administered at hospital. The European data from this study show that up to 83% of participants from Germany mentioned access to preventive treatment as a reason for referral, as compared to 19% in Italy and 17% in the United Kingdom.19
Specific guidelines are available for the diagnosis and management of headache in PC9 that include tools to help identify chronic migraine, such as headache diaries or calendars and validated scales to assess the impact of migraine on the patient’s daily living.9,26,27 The results of our study suggest that the main tools used to assess chronic migraine in PC are the clinical interview and the headache diary. All participants performed a clinical interview during the first visit, although only 60% did this during follow-up visits. One possible explanation for the decreased relevance of the clinical interview is the limited time available for PC visits in Spain. Regarding the use of headache diaries or calendars, 75% of participants reported using a headache diary during follow-up visits; this is in line with the relevant guidelines and consistent with the information reported by the other European countries included in the project (68.7%). The items recorded in the headache diary are similar in all countries, with the exception of headache intensity and whether pain increases with exercise, which were reported more frequently in Spain with regard to the European mean observed.19
In contrast, the use of validated scales for assessing the impact of migraine was limited: only 30% of participants used them during the first visit and up to 27% never used them. Considering that guidelines recommend using such scales during follow-up,9,14,15,27 it would be important to encourage their use in PC in Spain. The most widely used scale in the first consultation in Spain is the ID-Migraine (57.7%), a self-administered survey including 3 questions and specifically designed for use in PC. The survey, which has been shown to be valid and reliable for identifying migraines,28 is used by 77.8% of participants from Italy and 37.5% from the United Kingdom. It should also be mentioned that the ID-Chronic Migraine scale is used by approximately 60% of participants in Italy, but only 38.5% in Spain.19,20 This difference may be explained by the recent translation and validation of the Italian-language version of the scale.29
We also observed that 48% of participants prescribed imaging studies in follow-up visits. This may reflect a high level of diagnostic uncertainty, which results in increased use of healthcare resources and, consequently, increased cost of diagnostic confirmation. These data are in line with the findings of previous studies, which associate chronic migraine with increased use of healthcare resources in PC.14
Despite the high prevalence of chronic migraine,3 only 10% of participants considered they had sufficient training on the management of patients with chronic migraine. The lack of training on the diagnosis and management of chronic migraine in PC and other settings has previously been reported both in Spain and internationally.17,18,30–34 This need for training in Spain becomes more apparent when we compare the responses of Spanish participants with those from the remaining European countries, where only 55.2% consider that guidelines should include red flags and only 30.8% recommendations for referral.20 Finally, 40% of participants in Spain considered it essential to include validated scales to determine the impact of migraine on the patient’s daily living. We should underscore that these scales do not include red flags for the identification of secondary headache or recommended criteria for referral.
In this line, the SEN’s Headache Study Group recently published a series of recommendations on complementary examinations, criteria for referral, and red flags in patients with headache. This protocol may be applied both in emergency departments and in PC, and is aimed at improving the diagnosis and treatment of patients with (primary or secondary) headache and craniofacial neuralgia.35,36 Considering that the diagnostic delay in patients with migraine in Spain is more than 2 years, better coordination between specialists and PC is needed to improve patient management.37
The findings of this study support the need to establish protocols for the follow-up, treatment, and referral of patients with migraine, as proposed by Pascual et al.38 in a recent study conducted within the framework of the Global Campaign against Headache. In line with the conclusions of a 2006 study34 reporting a survey of 721 PC physicians in Spain, our data show a continued need for and interest in migraine training. Knowing the available tools and training PC physicians on the diagnosis and management of chronic migraine are essential for optimising the management of migraine patients and improving their quality of life.
LimitationsOne limitation of our study is that in the selection of participants, we sought to ensure a certain degree of knowledge on the treatment of headache; also, our study is based on a survey and, therefore, on participants’ recollections, which leads to a possible risk of double bias. Furthermore, although the sample was randomly selected, we cannot guarantee its representativeness of the population of PC physicians in Spain, as we applied selection criteria to ensure some experience with migraine.
ConclusionPC physicians in Spain are equipped with tools for the identification, management, and referral of patients with chronic and disabling migraine. However, these tools are not sufficiently used. Although follow-up of patients with migraine is mainly conducted in PC, PC physicians admit that patients with chronic migraine do not always receive symptomatic treatment or, particularly, adequate preventive treatment. Preventive medications, especially in chronic migraine, are very underused by PC physicians. Therefore, we believe that it continues to be necessary to reinforce the training of PC physicians to improve the management of these patients, and especially of those with chronic migraine, who require more complex and specialised treatments.
FundingThis study received financial support from Novartis Pharma AG.
Conflicts of interestSamuel Díaz Insa declares that he has received no funding for the drafting of this study. He has received personal funding from Allergan/Abbvie, Chiesi, Fundació Universitat-Empresa, Kern Pharma, Eli Lilly, Lundbeck, MSD, Novartis, and Teva.
María Navarro-Zornoza is an employee of Novartis Pharmaceuticals.
Rainel Sánchez-de la Rosa is an employee and shareholder of Novartis Pharma AG.
Angel L. Guerrero declares that he has received no funding for the drafting of this study. He has received funding from Allergan/Abbvie, Exeltis, Eli Lilly, Novartis, and Teva.