Titin is a sarcomeric protein expressed in the cardiac and skeletal muscles. It is encoded by a single gene, TTN, located on the long arm of chromosome 2.1TTN gene mutations have been associated with a wide range of cardiomyopathies and skeletal muscle disorders (late-onset tibial muscular dystrophy, early-onset recessive distal titinopathy, autosomal recessive limb-girdle muscular dystrophy-10, etc).2 Tibial muscular dystrophy (TMD), also known as Udd distal myopathy (late-onset, type 2a), is characterised by late onset (between the ages of 35 and 55 years) and slow progression, and usually only affects the muscles of the anterior compartment of the lower limbs.3 These patients present normal or slightly elevated serum creatine kinase levels, with EMG results suggestive of myopathy.3,4 Muscle biopsy results reveal variability in fibre size, central nuclei, necrosis, fibroadipose tissue, and rimmed vacuoles.5 Muscle MRI reveals selective fat replacement in the muscles of the anterior compartments of the lower limbs.
We present the case of a 37-year-old man with lower limb weakness and muscle atrophy affecting the peroneal and tibialis anterior muscles and the extensor muscles of the toes. He had no history of diabetes mellitus, cancer, or connective tissue disorders. A cardiac comorbidity was also detected, and the patient was diagnosed with dilated non-ischaemic cardiomyopathy. His parents were non-consanguineous, and he had family history of muscle disease of unknown origin in a maternal uncle, who presented weakness and muscle atrophy in the lower limbs. To date, his parents have not consulted due to neurological or cardiac symptoms.
The neurological examination revealed atrophy and weakness in the muscles of the anterior compartment of the lower limbs, with asymmetric weakness of ankle dorsiflexion (right, 1/5; left, 3/5). He was unable to toe walk as a result of the poor dorsiflexion.
A blood analysis including muscle enzymes and a mitochondrial respiratory chain enzyme assay yielded normal results. Electroneurography showed no alterations, and the EMG study revealed low-amplitude polyphasic motor unit potentials with early recruitment of the tibialis anterior muscles; these findings are compatible with a chronic myopathic process. A biopsy study of the quadriceps revealed myopathic alterations with nuclear centralisation and vacuolar degeneration, with no ragged red fibres and normal COX staining.
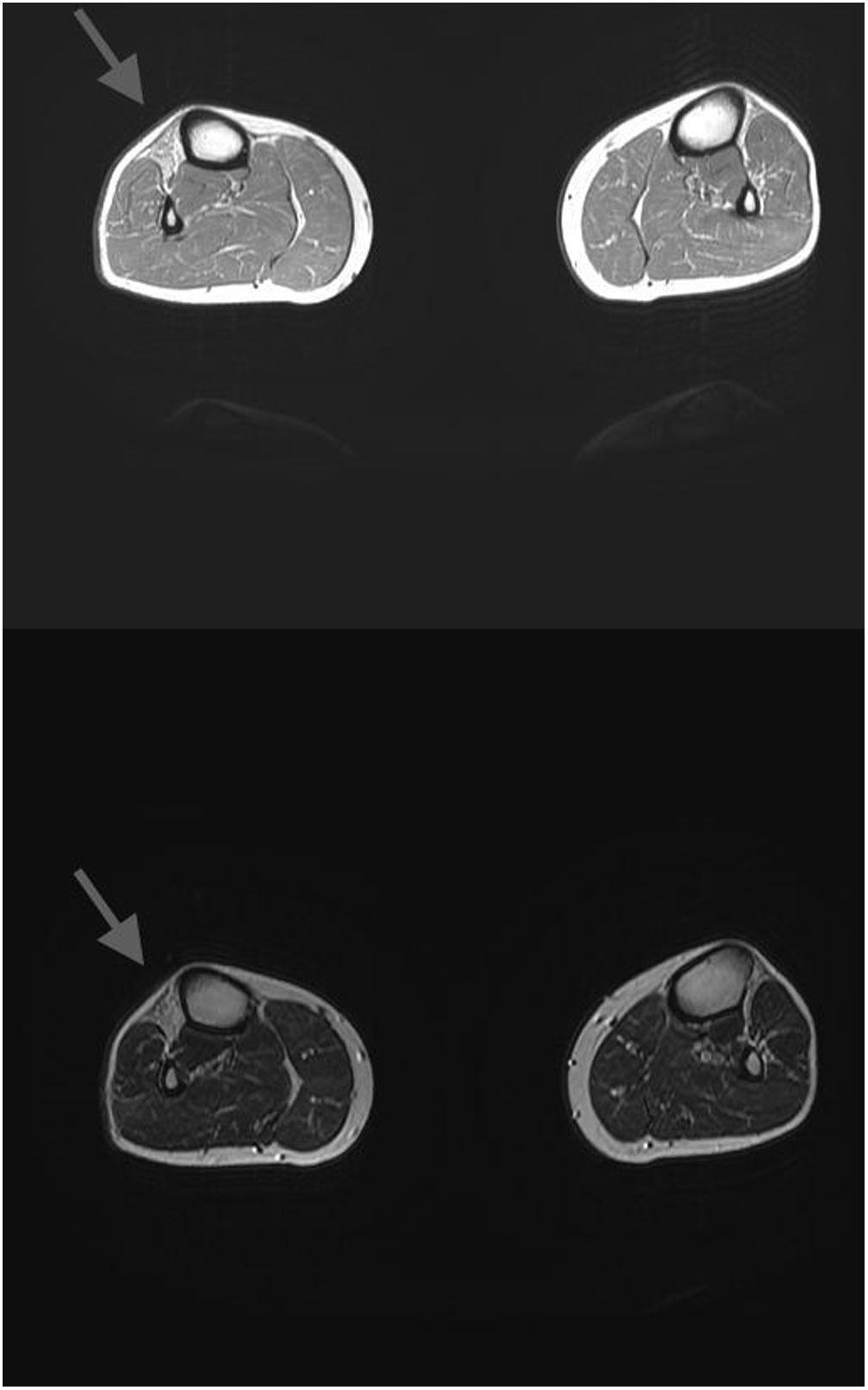
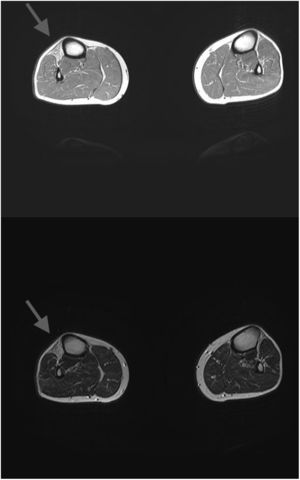
An MRI scan of the muscles of the lower limbs (Fig. 1) revealed atrophy with fat replacement in the extensor muscles (tibialis anterior, extensor digitorum longus, and extensor hallucis longus, predominantly on the right side). A cardiac MRI scan revealed biventricular dilatation with moderate systolic dysfunction affecting both ventricles, and dilatation of both atria; these findings are compatible with non-ischaemic cardiomyopathy.
Massive sequencing of 8 genes associated with muscular dystrophies (ANO5, DMD, DYSF, EMD, FHL1, LMNA, SYNE1, and SYNE2) detected no pathogenic mutations. A subsequent sequencing study of 22 genes, including TTN, revealed loss of heterozygosity, affecting at least exons 32 to 364 of the gene. The study detected the c.86581T>A (p.Trp28861Arg) TTN variant in homozygosis. Cosegregation analysis detected the same variant in heterozygosis in both parents.
TTN mutations have been associated with various muscle diseases, cardiomyopathies, or a combination of both. The first mutation (an 11-bp insertion/deletion) was reported in 2002, and was called FINmaj.6 A dominant missense mutation in exon 364 (c.107840T>A p.Ile35947Asn) was subsequently detected in a Belgian family.5 In 2008, Hackman et al.4 described 3 novel mutations in 2 Spanish families and 2 French families (2 deletions, g.292998delT and g.293376delA) and a nonsense mutation (g.293379C>T [p.Q33396X]). A more recent study describes the phenotype of an Italian family with TMD and a new heterozygous mutation, g.293326A>C, which predicts the amino acid substitution p.His33378Pro.7 Algahtani et al.8 report the heterozygous nonsense mutation c.85652C>G (p.Pro28551Arg) in a Saudi patient with bilateral facial weakness.
We describe a novel variant of TTN in homozygosis in a Spanish patient with TMD and cardiomyopathy. The patient presented nucleotide variant c.86581T>A (p.Trp28861Arg), apparently in homozygosis, in exon 341 of TTN. This variant causes the substitution of tryptophan for arginine at position 28861 of the polypeptide chain; these 2 amino acids have moderately different physicochemical properties. The change is located in a residue of the fibronectin type III domain, a conserved protein domain widely found in animal proteins. This variant has not previously been described in the literature, nor is it included in the ClinVar, dbSNP, ExAC, or ESP databases.
The presence of weakness affecting the muscles of the anterior compartment of the lower limbs suggests that this novel homozygous variant of TTN is pathogenic, and potentially involved in the pathogenesis of TMD and cardiomyopathy.
Please cite this article as: Lopez-Bravo A, Roche-Bueno JC, Romera-López A, Larrode-Pellicer P. Una nueva variante en el gen de la titina en un paciente con miopatía distal de miembros inferiores y miocardiopatía dilatada. Neurología. 2021;36:721–723.