Infectious processes are one of the most frequent causes of morbidity and mortality in patients with systemic lupus erythematosus (SLE). This is due both to the immunological dysfunction caused by the disease itself and the immunosuppressive treatment.1 Most of these infections are of bacterial origin,2 although infection with parvovirus or viruses from the herpesvirus family, including varicella-zoster virus (VZV), is not infrequent.3 In turn, case series of systemic infections with such fungi as Cryptococcus neoformans have also been reported.4
Most cases of C. neoformans meningoencephalitis occur in patients with AIDS with CD4 counts below 100 cells/µL,5 but it also manifests in seronegative patients, especially those who are immunocompromised for other reasons, including patients with SLE.6,7 Cases of meningoencephalitis due to VZV infection in patients with SLE are scarce in the literature.8
The aim of this article is to report the first case in the literature of central nervous system co-infection with C. neoformans and VZV in a patient with SLE and treated with mycophenolate mofetil (MMF) and corticosteroids.
Our patient was an 18-year-old woman with SLE with haematological (autoimmune haemolytic anaemia treated with decreasing doses of prednisone from the previous year) and pulmonary involvement (bronchiectasis and recurring infections treated with antibiotics and cycles of prophylactic azithromycin), as well as positive antiphospholipid antibodies, treated with prednisone (5 mg/24 h), MMF (1 g/12 h), and hydroxychloroquine.
The patient initially presented persistent severe headache and vomiting after manifesting symptoms compatible with respiratory infection in the previous week, which were treated with antibiotics. An eczema-like lesion without vesicles was observed on the outer ear. Several days later, she manifested behavioural alterations and irritability, as well as decreased level of consciousness, and finally an episode compatible with seizure. The patient did not present fever during the episodes.
An emergency head CT scan revealed a slight left occipital cortical hypodensity. She subsequently underwent a lumbar puncture, obtaining clear cerebrospinal fluid (CSF), which revealed slight, predominantly mononuclear pleocytosis (100 cells) and high protein levels. Opening pressure was not measured at that time.
Due to the possibility of autoimmune encephalitis, the patient received a megadose of methylprednisolone. She was also treated with aciclovir and antibiotics (as we could not rule out meningoencephalitis that resolved due to the recent antibiotic treatment), and MMF was suspended due to the possibility of posterior reversible encephalopathy syndrome.
We requested a CSF microbiological study, including Gram and India ink staining, bacterial and fungal cultures, and a PCR assay panel (FilmArray®). The PCR assay detected Cryptococcus and VZV, and India ink staining showed presence of fungi. The culture was also positive for C. neoformans. We started treatment with amphotericin B and flucytosine and suspended antibiotic treatment and high-dose corticosteroids, but maintained aciclovir.
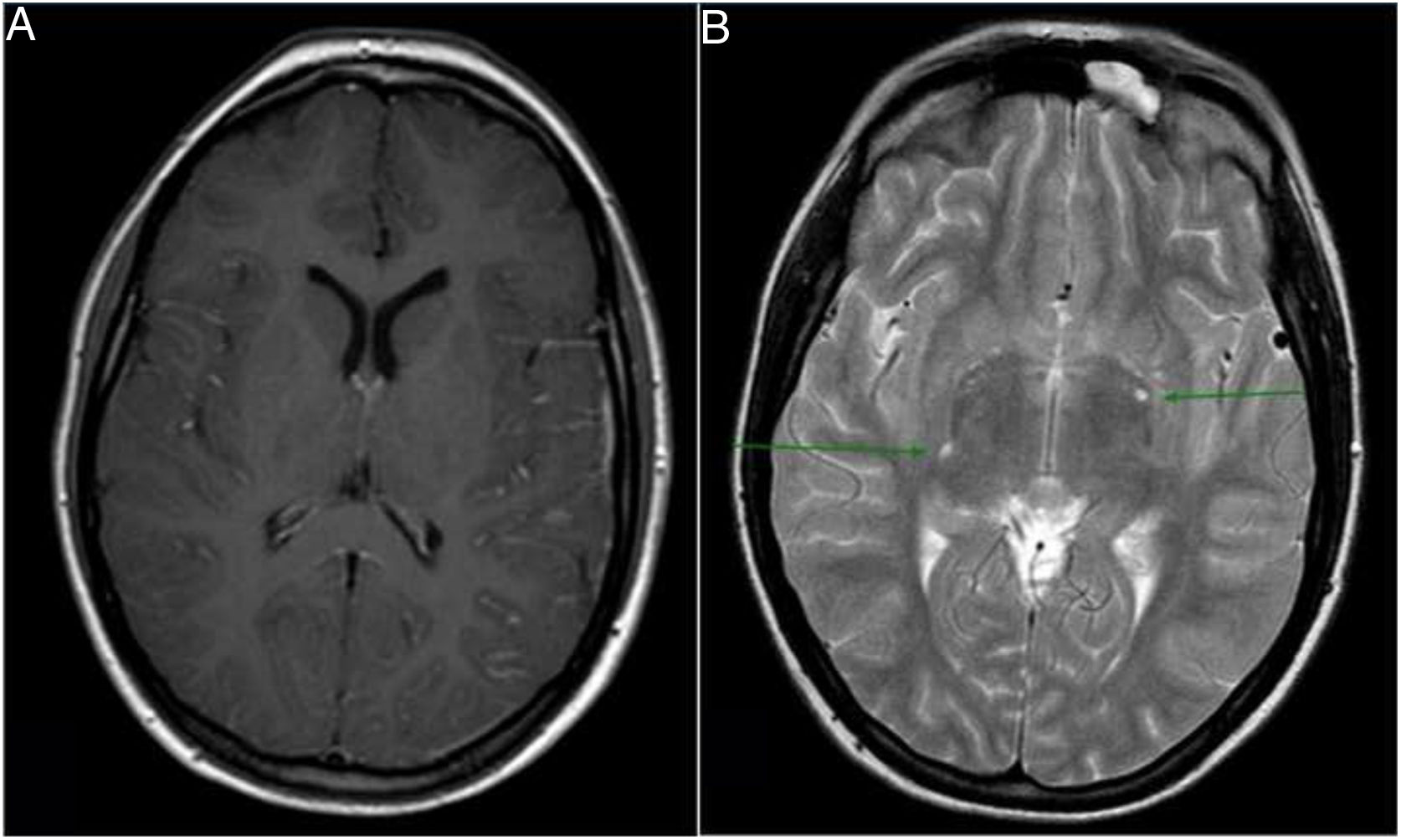
A brain MRI scan confirmed that the hypodensity observed in the head CT scan corresponded to vasogenic oedema, which is compatible with an encephalitis-like inflammatory process in this clinical context. We also observed diffuse leptomeningeal enhancement and 2 dilated Virchow-Robin spaces with minimal contrast enhancement (Fig. 1). Dilated Virchow-Robin spaces in the basal ganglia constitute one characteristic of brain cryptococcosis, and may merge and form what are known as gelatinous pseudocysts.
In the subsequent hours, the patient developed vesicles in the eczema previously observed on the outer ear. Reduced level of consciousness and intense headache persisted, in association with bilateral limitation of gaze abduction. Due to these symptoms, we suspected intracranial hypertension, which is also characteristic of cryptococcal meningitis. CSF pressure was measured, revealing an opening pressure of 60 cm H2O. In the absence of an intracranial space-occupying lesion, an external lumbar drain was placed, and achieved a significant improvement. Aciclovir was suspended after 2 weeks, and amphotericin B and flucytosine after 3 weeks; after 4 weeks, oral fluconazole was started and the external lumbar drain was removed. The patient’s condition progressed favourably, with eventual full resolution.
DiscussionOurs is the first case in the literature of central nervous system co-infection with VZV and C. neoformans. The literature does include reports of cryptococcal meningitis9 following cutaneous herpes zoster, and vice versa,10 in HIV-positive patients, with no presence of VZV in the CSF.
Several factors may have contributed to co-infection, including immunosuppressive treatment with corticosteroids and MMF, as well as the presence of SLE, an autoimmune disease.
This case highlights the importance of considering the possibility of infection with atypical pathogens, even simultaneously, as cause of encephalitis in patients with autoimmune diseases, especially those receiving immunosuppressive treatment. Therefore, we recommend performing an extensive microbiological study including bacterial cultures as well as fungal and viral studies.
FundingThe authors of this study have been awarded a grant by the Spanish Foundation of Rheumatology.
Please cite this article as: Cabezudo-García P, Castro-Sánchez MV, Mena-Vázquez N, Fernández-Nebro A, Meningoencefalitis por Cryptococcus neoformans y virus varicela-zoster en paciente con lupus eritematoso sistémico. Neurología. 2021;36:719–721.