The elderly population is the group most threatened by COVID-19, with the highest mortality rates. This study aims to analyse the case fatality of COVID-19 in a cohort of patients with degenerative dementia.
MethodsWe conducted a descriptive case-control study of a sample of patients diagnosed with primary neurodegenerative dementia.
ResultsTwenty-four of the 88 patients with COVID-19 included in the study died: 10/23 (43.4%) patients diagnosed with dementia and 14/65 (21.5%) controls; this difference was statistically significant.
DiscussionOur results suggest that case fatality of COVID-19 is significantly higher among patients with primary degenerative dementia than in other patients with similar mean ages and comorbidities.
La población anciana es la más amenazada por COVID-19, con mayores tasas de mortalidad. El objetivo de este trabajo es analizar la letalidad en una cohorte de pacientes de COVID-19 con demencia degenerativa.
MétodosHicimos un estudio descriptivo de casos-control de una muestra de pacientes diagnosticados con demencias neurodegenerativas primarias.
ResultadosDe los 88 pacientes incluidos en el estudio, 24 pacientes con COVID-19 fallecieron: 10/23 (43,4%) eran pacientes con diagnóstico de demencia y 14/65 (21,5%) pacientes del grupo control, una diferencia estadísticamente significativa.
DiscusiónLa letalidad entre los pacientes con demencia degenerativa primaria por COVID-19 es significativamente mayor en comparación con otros pacientes con edades medias y comorbilidades similares, según nuestro estudio.
On 11 March 2020, the WHO declared the outbreak of SARS-CoV-2 a pandemic. The virus is lethal and highly dangerous, and is similar to the SARS-CoV virus that emerged in 2003.1,2 As of 23 April 2020, there are estimated to be 2 544 792 confirmed cases worldwide, with 175 694 deaths recorded in 213 countries.1
This novel coronavirus belongs to the group of beta-coronaviruses, for which bats constitute the main reservoir and origin. They present high pathogenicity and infectivity, leading to high mortality rates.3 Clinical presentations of COVID-19 include a syndrome of respiratory insufficiency and pneumonia, with a clinical spectrum ranging from banal flu-like symptoms or even asymptomaticity to acute cases of highly fatal respiratory failure.4 SARS-CoV-2 is thought to infect the nervous system through the angiotensin-converting enzyme 2 (ACE2) receptor and the transmembrane protease serine 2 (TMPRSS2), both of which are necessary for the virus to enter cells and are present in neurons, glial cells, and respiratory epithelial cells.5
The elderly population is the group most threatened by COVID-19, with the highest mortality and fatality rates, especially among individuals who live in retirement or nursing homes, as shown by mass media and government data. Furthermore, some studies report that up to one-third of the elderly population living in nursing homes have primary degenerative dementia (PDD).6 In Spain, Ministry of Health data (consulted 23 April 2020) indicate that 36% of the 148 069 reported cases corresponded to individuals older than 70 years; this age group accounts for 86% of deaths from the disease.7 The proportion of individuals with primary degenerative dementia is known to be much higher in this age group (up to 9.4% in patients older than 70 years8); while the presence of primary degenerative dementia does not in itself increase the risk of developing COVID-19, it does increase the risk of complications and death.
Case fatality in this age group is higher than in the general population. A Chinese study reports case fatality rates of 8% in patients aged between 70–79 years and 14.8% in patients older than 80 years.9 However, to our knowledge, little evidence is available on case fatality rates in patients with primary dementias. The aim of this study is to analyse a series of patients with primary degenerative dementia and COVID-19 who were treated at our hospital, considering their clinical status, prognosis, and treatment. Our hypothesis is that presence of degenerative dementia increases case fatality rates among patients with COVID-19.
Material and methodsDesignWe conducted a descriptive case-control study of a sample of patients with PDD at the Málaga Institute of Biomedical Research and the neurology department at Hospital Regional Universitario de Málaga (HRUM).
Study groupAfter reviewing emergency department admissions between 14 March 2020 and 15 May 2020, inclusive, using the Diraya electronic history system, we included patients admitted to the emergency department at HRUM with suspected COVID-19. Patients with dementia were diagnosed at the memory units at HRUM and Hospital Virgen de la Victoria (Málaga). We also included patients with mild cognitive impairment of probable neurodegenerative origin. We excluded patients with vascular dementia due to stroke, dementia, or cognitive impairment due to another cause and patients with active neoplasia.
Control groupTo compare the case fatality of COVID-19 in patients with primary dementias, we also analysed a group of patients with COVID-19 without dementia from our hospital. We excluded patients with a final aetiological diagnosis other than COVID-19.
Study protocolWe selected patients meeting the inclusion criteria and admitted to the HRUM emergency department’s COVID-19 unit. The unit is an independent area dedicated to the assessment of patients presenting biological hazard. It includes a consultation area, a critical care room, and a dedicated radiology team. All patients with signs and symptoms compatible with SARS-CoV-2 infection were admitted through this pathway. Patients were assessed by a physician who requested a laboratory analysis and radiological and microbiological studies, in line with the recommendations of the Spanish Ministry of Health.10
We included patients with acute respiratory infection compatible with COVID-19, as Spain was considered to present community transmission. RT-PCR testing was performed in all patients with moderate-severe symptoms or mild cases presenting some risk factor for severe COVID-19. Diagnosis was clinical in patients with mild symptoms and no risk factors; these were considered “possible cases.”11 RT-PCR testing was performed at least once in all hospitalised patients. Those patients with clinical/radiological signs compatible with COVID-19, negative RT-PCR results, and no other likely aetiology were considered “probable cases,” in accordance with the guidelines of the Spanish Ministry of Health. Patients with positive RT-PCR results were considered confirmed cases. In our study, clinical history data were systematically recorded using a predefined form.
ObjectivesThe main aim of this study was to estimate case fatality. Case fatality was estimated according to the number of deaths occurring during the recruitment period. We included a similar control group of patients with COVID-19 and without primary dementia from the same hospital, to test the hypothesis of a higher case fatality rate of COVID-19 in the group with primary dementia.
Sample characteristicsCOVID-19 was diagnosed according to the classification of the Spanish Ministry of Health: confirmed cases (patients with positive RT-PCR results for SARS-CoV-2) and probable cases (patients with a severe acute respiratory infection requiring hospitalisation and with clinical and radiological characteristics compatible with COVID-19, in the absence of RT-PCR confirmation). We recorded all the treatments administered for COVID-19: azithromycin, hydroxychloroquine/chloroquine, lopinavir/ritonavir, remdesivir, anti–IL-6, anti–IL-1, steroids, and intravenous immunoglobulins.
Other variablesWe collected data on the following variables: age; sex; institutionalisation in retirement or nursing homes (patients dependent for such everyday tasks as getting dressed, eating, walking, or hygiene); and cardiovascular risk factors, including history of smoking, hypertension, type 2 diabetes mellitus, heart disease (ischaemic heart disease, congestive heart failure, or significant arrhythmic events [atrial fibrillation]), and pulmonary disease (chronic obstructive pulmonary disease, pulmonary fibrosis, or active asthma). Regarding dementia, we collected the following data from patients diagnosed with primary dementia at the memory unit: type of degenerative dementia (Alzheimer disease, Lewy body dementia, frontotemporal dementia, corticobasal syndrome, progressive supranuclear palsy, Parkinson’s dementia), and degree of dementia according to the Hughes Clinical Dementia Rating scale (CDR 0.5 = questionable dementia; CDR 1 = mild cognitive impairment; CDR 2 = moderate cognitive impairment; CDR 3 = severe cognitive impairment). We also recorded data on treatment with acetylcholinesterase inhibitors, memantine, and antipsychotics.
Data availabilityAny unpublished anonymised data will be available to qualified researchers upon request.
Statistical analysisWe first used the chi-square test and t test or the Mann-Whitney U test to compare the main characteristics between patients with dementia and matched controls without dementia, as well as to compare the main characteristics of patients with dementia according to vital prognosis. Qualitative variables are expressed as absolute frequencies and percentages and quantitative variables as mean (SD) or median (IQR), according to whether they present normal distribution. Normal distribution for continuous variables was confirmed using the Kolmogorov-Smirnov test. We conducted 2 stepwise logistic regression models: one to analyse which variables are independently associated with case fatality and another to identify the variables associated with case fatality in patients with dementia. This analysis only included variables with statistical significance or clinical interest. A P-value < .05 was considered statistically significant in all analyses. Data were analysed using the R 2.4.0 statistical software.
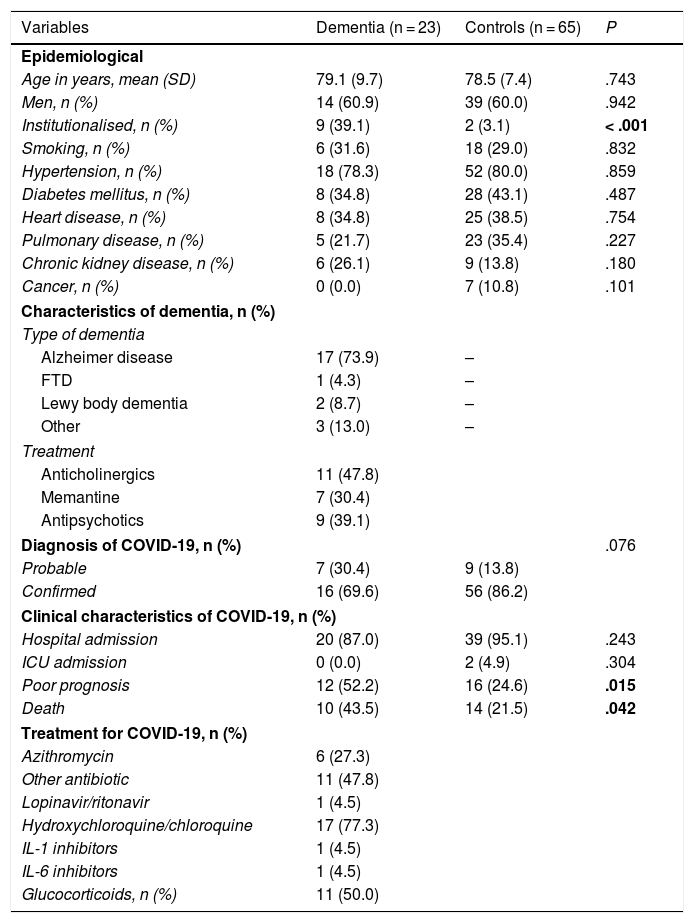
ResultsCharacteristics of patients with COVID-19The sample included a total of 23 cases and 65 controls. Table 1 includes the main characteristics of both groups. Most patients were men (60%), and mean age was 79 years. Hypertension was the most frequent comorbidity, followed by diabetes mellitus and heart disease. Regarding epidemiological characteristics, we found no significant differences between cases and controls, except in the percentage of institutionalised patients, which was higher among patients with dementia (39.1% vs 3.1%; P < .001).
Characteristics of cases and controls.
| Variables | Dementia (n = 23) | Controls (n = 65) | P |
|---|---|---|---|
| Epidemiological | |||
| Age in years, mean (SD) | 79.1 (9.7) | 78.5 (7.4) | .743 |
| Men, n (%) | 14 (60.9) | 39 (60.0) | .942 |
| Institutionalised, n (%) | 9 (39.1) | 2 (3.1) | < .001 |
| Smoking, n (%) | 6 (31.6) | 18 (29.0) | .832 |
| Hypertension, n (%) | 18 (78.3) | 52 (80.0) | .859 |
| Diabetes mellitus, n (%) | 8 (34.8) | 28 (43.1) | .487 |
| Heart disease, n (%) | 8 (34.8) | 25 (38.5) | .754 |
| Pulmonary disease, n (%) | 5 (21.7) | 23 (35.4) | .227 |
| Chronic kidney disease, n (%) | 6 (26.1) | 9 (13.8) | .180 |
| Cancer, n (%) | 0 (0.0) | 7 (10.8) | .101 |
| Characteristics of dementia, n (%) | |||
| Type of dementia | |||
| Alzheimer disease | 17 (73.9) | – | |
| FTD | 1 (4.3) | – | |
| Lewy body dementia | 2 (8.7) | – | |
| Other | 3 (13.0) | – | |
| Treatment | |||
| Anticholinergics | 11 (47.8) | ||
| Memantine | 7 (30.4) | ||
| Antipsychotics | 9 (39.1) | ||
| Diagnosis of COVID-19, n (%) | .076 | ||
| Probable | 7 (30.4) | 9 (13.8) | |
| Confirmed | 16 (69.6) | 56 (86.2) | |
| Clinical characteristics of COVID-19, n (%) | |||
| Hospital admission | 20 (87.0) | 39 (95.1) | .243 |
| ICU admission | 0 (0.0) | 2 (4.9) | .304 |
| Poor prognosis | 12 (52.2) | 16 (24.6) | .015 |
| Death | 10 (43.5) | 14 (21.5) | .042 |
| Treatment for COVID-19, n (%) | |||
| Azithromycin | 6 (27.3) | ||
| Other antibiotic | 11 (47.8) | ||
| Lopinavir/ritonavir | 1 (4.5) | ||
| Hydroxychloroquine/chloroquine | 17 (77.3) | ||
| IL-1 inhibitors | 1 (4.5) | ||
| IL-6 inhibitors | 1 (4.5) | ||
| Glucocorticoids, n (%) | 11 (50.0) | ||
Statistically significant differences are shown in bold. FTD: frontotemporal dementia; ICU: intensive care unit.
Most patients presented Alzheimer-type dementia (73.9%), which was moderate or severe in most cases (56.5%). Eighteen patients were under treatment with anticholinesterase inhibitors and/or memantine and 9 were receiving antipsychotics.
Regarding COVID-19 characteristics, 16 cases (69.6%) were confirmed by RT-PCR testing and 7 were considered probable cases. A higher percentage of patients than controls had poor prognosis (52.2% vs 24.6%; P = .015), or died (43.5% vs 21.5%; P = .042). Table 1 shows the treatments administered.
Factors associated with case fatality in patients with COVID-19Twenty-four of the 88 patients included in the study died: 10 patients with dementia (43.4%) and 14 controls (21.5%).
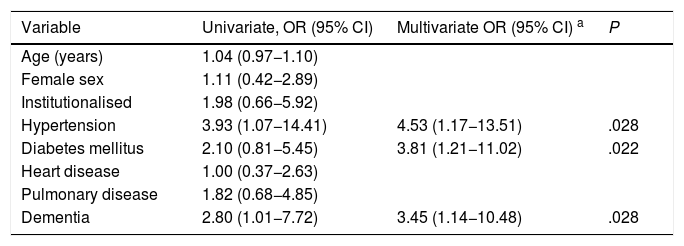
Table 2 shows the multivariate logistic regression analysis (dependent variable: case fatality) in patients with COVID-19. Arterial hypertension, diabetes mellitus, and dementia were independently associated with case fatality in patients with COVID-19.
Multivariate analysis of case fatality in patients with COVID-19.
| Variable | Univariate, OR (95% CI) | Multivariate OR (95% CI) a | P |
|---|---|---|---|
| Age (years) | 1.04 (0.97−1.10) | ||
| Female sex | 1.11 (0.42−2.89) | ||
| Institutionalised | 1.98 (0.66−5.92) | ||
| Hypertension | 3.93 (1.07−14.41) | 4.53 (1.17−13.51) | .028 |
| Diabetes mellitus | 2.10 (0.81−5.45) | 3.81 (1.21−11.02) | .022 |
| Heart disease | 1.00 (0.37−2.63) | ||
| Pulmonary disease | 1.82 (0.68−4.85) | ||
| Dementia | 2.80 (1.01−7.72) | 3.45 (1.14−10.48) | .028 |
The variables included in the equation were: sex, age, arterial hypertension, diabetes mellitus, and dementia.
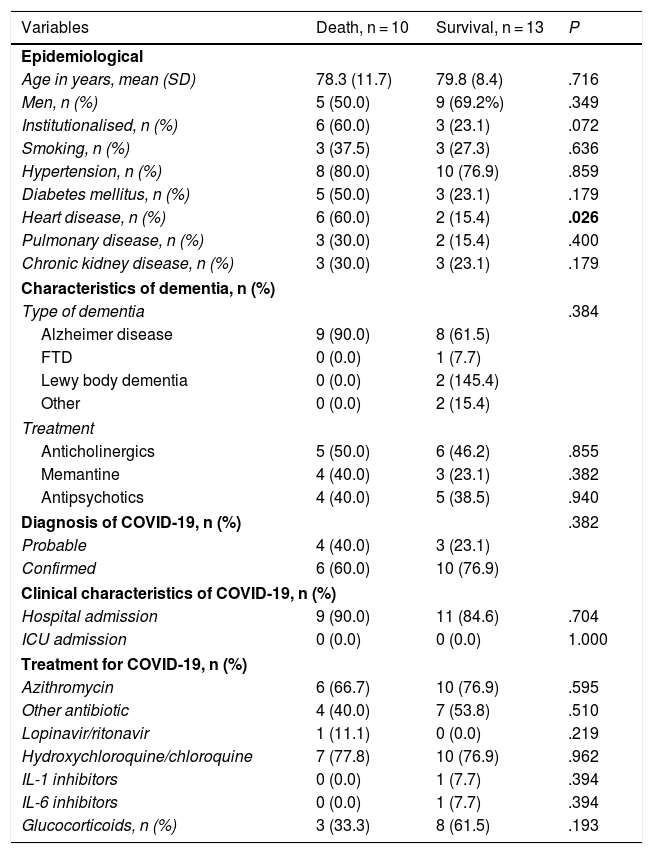
In the bivariate analysis (Table 3), patients with heart disease presented significantly higher case fatality rates (60% vs 15.4%; P = .026). Furthermore, patients living in nursing homes showed a trend towards higher case fatality than that recorded in non-institutionalised patients (60% vs 23.1%; P = .072). We found no other differences between these groups.
Characteristics of patients with dementia and COVID-19.
| Variables | Death, n = 10 | Survival, n = 13 | P |
|---|---|---|---|
| Epidemiological | |||
| Age in years, mean (SD) | 78.3 (11.7) | 79.8 (8.4) | .716 |
| Men, n (%) | 5 (50.0) | 9 (69.2%) | .349 |
| Institutionalised, n (%) | 6 (60.0) | 3 (23.1) | .072 |
| Smoking, n (%) | 3 (37.5) | 3 (27.3) | .636 |
| Hypertension, n (%) | 8 (80.0) | 10 (76.9) | .859 |
| Diabetes mellitus, n (%) | 5 (50.0) | 3 (23.1) | .179 |
| Heart disease, n (%) | 6 (60.0) | 2 (15.4) | .026 |
| Pulmonary disease, n (%) | 3 (30.0) | 2 (15.4) | .400 |
| Chronic kidney disease, n (%) | 3 (30.0) | 3 (23.1) | .179 |
| Characteristics of dementia, n (%) | |||
| Type of dementia | .384 | ||
| Alzheimer disease | 9 (90.0) | 8 (61.5) | |
| FTD | 0 (0.0) | 1 (7.7) | |
| Lewy body dementia | 0 (0.0) | 2 (145.4) | |
| Other | 0 (0.0) | 2 (15.4) | |
| Treatment | |||
| Anticholinergics | 5 (50.0) | 6 (46.2) | .855 |
| Memantine | 4 (40.0) | 3 (23.1) | .382 |
| Antipsychotics | 4 (40.0) | 5 (38.5) | .940 |
| Diagnosis of COVID-19, n (%) | .382 | ||
| Probable | 4 (40.0) | 3 (23.1) | |
| Confirmed | 6 (60.0) | 10 (76.9) | |
| Clinical characteristics of COVID-19, n (%) | |||
| Hospital admission | 9 (90.0) | 11 (84.6) | .704 |
| ICU admission | 0 (0.0) | 0 (0.0) | 1.000 |
| Treatment for COVID-19, n (%) | |||
| Azithromycin | 6 (66.7) | 10 (76.9) | .595 |
| Other antibiotic | 4 (40.0) | 7 (53.8) | .510 |
| Lopinavir/ritonavir | 1 (11.1) | 0 (0.0) | .219 |
| Hydroxychloroquine/chloroquine | 7 (77.8) | 10 (76.9) | .962 |
| IL-1 inhibitors | 0 (0.0) | 1 (7.7) | .394 |
| IL-6 inhibitors | 0 (0.0) | 1 (7.7) | .394 |
| Glucocorticoids, n (%) | 3 (33.3) | 8 (61.5) | .193 |
Statistically significant differences are shown in bold. FTD: frontotemporal dementia; ICU: intensive care unit.
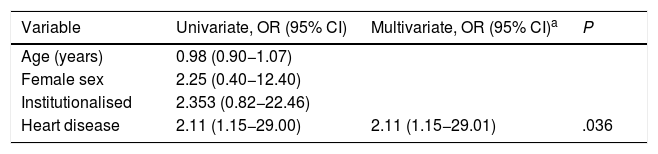
Table 4 shows the multivariate logistic regression analysis (dependent variable: case fatality of COVID-19) in patients with dementia. Heart disease was associated with a twofold increase in the risk of death due to COVID-19 in patients diagnosed with dementia.
Multivariate analysis of case fatality in patients with dementia and COVID-19.
| Variable | Univariate, OR (95% CI) | Multivariate, OR (95% CI)a | P |
|---|---|---|---|
| Age (years) | 0.98 (0.90−1.07) | ||
| Female sex | 2.25 (0.40−12.40) | ||
| Institutionalised | 2.353 (0.82−22.46) | ||
| Heart disease | 2.11 (1.15−29.00) | 2.11 (1.15−29.01) | .036 |
All variables were included in the equation.
The prevalence of cardiovascular comorbidities and chronic respiratory disease was considerable in both groups, with no significant differences between patients with primary dementia and controls. Primary dementia probably increases the risk of death, in comparison with individuals without degenerative dementia. A Spanish study showed a population attributable risk of 11.3%; however, epidemiological data on COVID-19–associated mortality rates are limited, and we are yet to determine the effect on vital prognosis of such important variables as the use of certain drugs (eg, antipsychotics), comorbidities, and age.8
According to published case series,9,12 patients with COVID-19 and presenting such comorbidities as arterial hypertension, heart diseases, diabetes, or history of such respiratory diseases as chronic obstructive pulmonary disease present greater risk of complications and case fatality. Up to 80% of deaths due to COVID-19 are recorded in patients older than 80 years, with some comorbidity recorded in up to 80% of cases; diabetes presents the greatest effect on mortality.12
An Italian study conducted in May 2020 reported a mortality rate of 62.2% (51/82) in patients with primary dementia, with higher rates associated with more severe dementia (83.9% in patients with severe dementia).13 These results are similar to our own: we found a COVID-19–associated case fatality rate of 43.4% in patients with dementia; this was significantly higher than the rate in the control group. The case fatality rate was higher in older patients, in those with more severe dementias, and in institutionalised patients. Arterial hypertension, diabetes mellitus, and dementia were independently associated with case fatality in the analysis of all patients with COVID-19. Heart diseases were more prevalent in the group of patients with primary degenerative dementia, and were associated with a statistically significant increase in the mortality rate.
We should be aware of the prevalence of primary dementia in patients older than 80 years, which amounts to 9.4%.8 Considering these data, it seems probable that degenerative dementia increases the risk of death in patients with COVID-19, although there is not yet sufficient evidence supporting this hypothesis. Another significant factor is that patients with moderate or severe dementia are not usually admitted to intensive care units, especially during the specific circumstances of this pandemic. This results in higher mortality due to SARS-CoV-2 infection in patients with dementia in general. In our study, no patient from the study group was admitted to the ICU.
Furthermore, patients living in nursing homes in Spain present a high mortality rate. In 2019, there were 5417 centres in Spain, with approximately 271 696 residents. Mortality rates associated with COVID-19 in these centres are alarming: up to 10 719 residents had died as of 16 April, due to the precarious situation of the healthcare system and the lack of healthcare resources in many of these residences.14 Our study shows that case fatality was higher among previously institutionalised patients (66.6% vs 28.5%), although this was not a significant factor for case fatality. One of the main causes for institutionalisation is the onset of moderate or severe dementia. Up to 76% of patients presented some degree of cognitive impairment (probably underdiagnosed in many cases), and a third were diagnosed with dementia, with a mean age of 81.2 (10.2) years.6
Mortality due to COVID-19 in nursing homes is not currently well-established, and data provided by Spanish government agencies are not rigorous.
The care provided to patients with dementia during this pandemic should not be neglected. The increased workload due to the pandemic may reduce care and quality of life in this group of patients,14 especially those living in retirement or nursing homes.15
It is also important to acknowledge the neuroinvasive potential of SARS-CoV-2, which may impact progression or give rise to neuropathological changes leading to neurodegenerative disease, such as Alzheimer disease; therefore, in the short or medium term we may find ourselves facing a “delayed pandemic.”16
The limitations of our study include the small number of cases, and a possible selection bias, as patients were retrospectively selected from the group of patients who attended the emergency department at our hospital; those who died at another hospital or at a nursing home were not considered. The case fatality rate among institutionalised patients is significantly higher, which may represent an additional confounding factor; therefore, the effect of dementia on the case fatality rate of COVID-19 in this group of patients may be overestimated.
ConclusionOur study suggests that the case fatality of COVID-19 is significantly higher in patients with primary degenerative dementia than among other patients with similar ages and comorbidities. Several factors influence this trend: these patients are not usually admitted to intensive care units; they present greater limitations on the use of advanced and aggressive treatments; they present a higher rate of cardiovascular and respiratory comorbidities; and lastly, a significant percentage of this group is institutionalised. Future studies with larger samples of patients with dementia and COVID-19 are needed to confirm our results and to identify other possible risk factors associated with the severity of COVID-19 in patients with dementia.
FundingThis study was funded by the COVID-19 fund from Institute of Health Carlos III, Spain (project no. COV20/00157).
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Reyes-Bueno JA, Mena-Vázquez N, Ojea-Ortega T, Gonzalez-Sotomayor MM, Cabezudo-Garcia P, Ciano-Petersen NL et al. Análisis de letalidad por COVID-19 en pacientes con demencia neurodegenerativa. Neurología. 2020;35:639–645.