Cervical artery dissection is an infrequent cause of ischaemic stroke. However, it explains nearly 20% of strokes in young patients (<45 years). Vertebral artery dissection is less common than carotid artery dissection (1-1.5 cases per 100000 person-years; only 16% are bilateral).1 Around 2% of patients experience spontaneous recurrences during the first 30 days. Several pathogenic factors for cervical artery dissection have been identified, including cervical spine trauma (in 40.5% of cases)2,3 and such other environmental factors as infections and oral contraceptives. Other risk factors include genetic disorders with a familial association, such as α1-antitrypsin deficiency, connective tissue disorders, gene polymorphisms causing vessel abnormalities, migraine, and hyperhomocysteinaemia.4,5 Cushing syndrome is not considered a risk factor for cervical artery dissection.
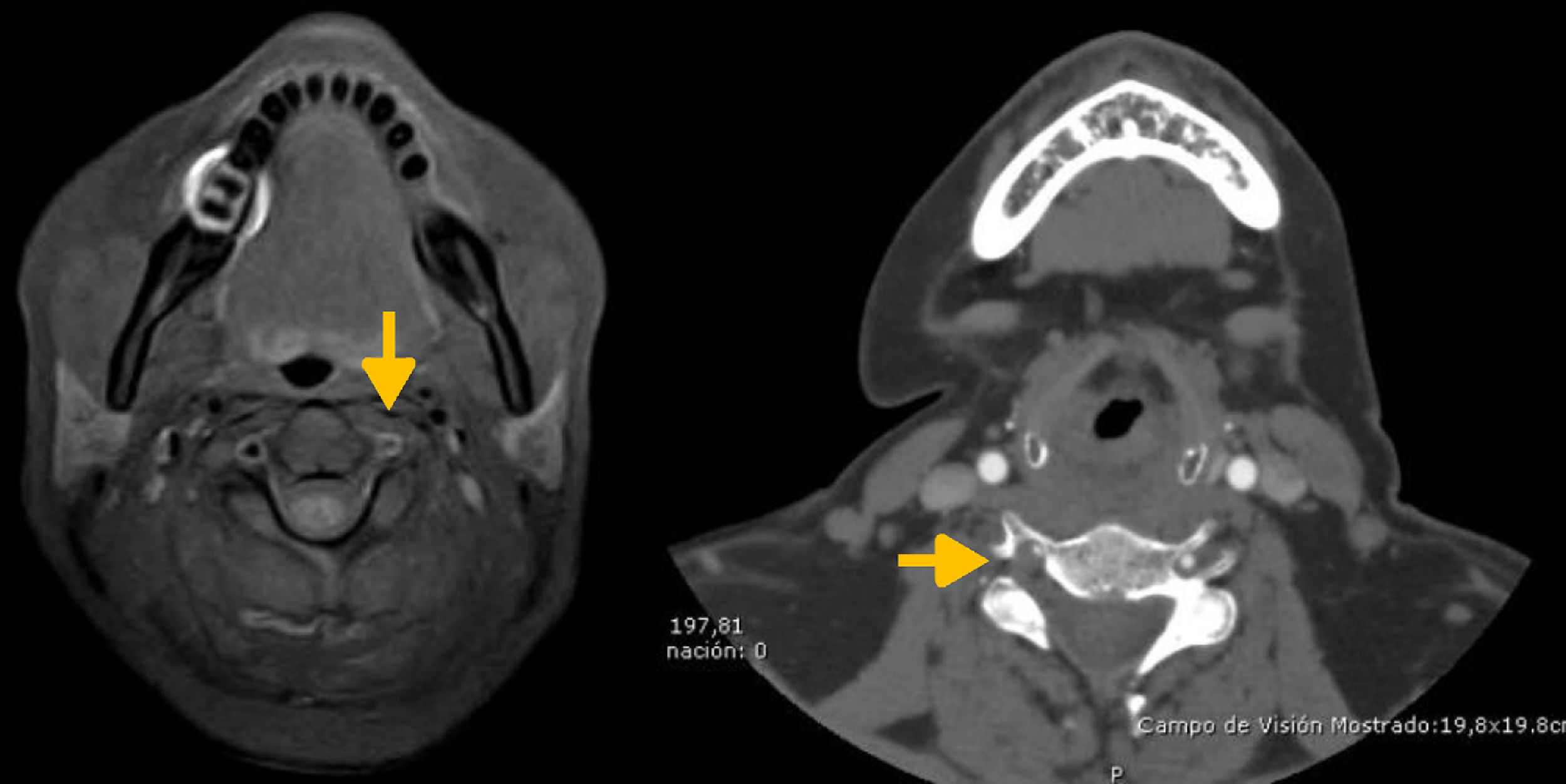
We present the case of a 38-year-old woman with no relevant medical history who was admitted to the emergency department due to pain in the left cervical region and sudden-onset ataxia. An MRI scan of the head and neck revealed acute infarction of the left side of the medulla oblongata and left vertebral artery dissection (Fig. 1). Symptoms improved, and the patient was discharged a week after symptom onset; she was prescribed antiplatelet treatment (aspirin 100mg). Five days later, the patient was readmitted due to another episode of severe neck pain, dizziness, and worsening of ataxia. A neck CT scan revealed another dissection, affecting the right vertebral artery, and recanalisation of the left vertebral artery (Fig. 2). A comprehensive hormone analysis revealed increased adrenocorticotropic hormone (ACTH) levels and presence of cortisol in 24-hour urine. The patient was diagnosed with ACTH-dependent Cushing syndrome due to production of ACTH and ectopic corticotropin-releasing hormone. We started treatment with ketoconazole. A chest, abdomen, and pelvis CT scan revealed an incidentaloma in the left adrenal gland.
In patients with Cushing syndrome, the catabolic effects of cortisol promote endothelial damage; vascular damage is therefore mainly caused by increased predisposition to systemic atherosclerosis. Cushing syndrome has traditionally been associated with an increased risk of intracranial aortic aneurysms.6 It has been suggested that aneurysm formation is a consequence of hypercortisolaemia, which affects the smooth muscle layer of the artery, causing metaplastic alterations, with fibroblast-like cells. High cortisol levels may increase blood vessel fragility, which may have a negative effect due to inhibition of collagen biosynthesis and increased catabolism of collagen.7 The levels of markers of damage and inflammation (endothelin, resistin, vascular endothelial growth factor, tumour necrosis factor alpha, interleukin-8) are known to increase in patients with Cushing syndrome, making vessel walls more vulnerable to trauma. Vertebral artery dissection associated with Cushing syndrome is an extremely rare occurrence, and the underlying mechanism is yet to be fully understood. Further research is necessary to determine whether hormone analyses should be included in the diagnostic protocol for spontaneous cervical artery dissection. To our knowledge, this is the first case of bilateral vertebral artery dissection as the initial manifestation of Cushing syndrome to be reported in the literature.
Please cite this article as: Pérez Torre P, Monreal Laguillo E, Vera Lechuga R, Cruz Culebras A. Disección arterial vertebral bilateral como manifestación inicial del síndrome de Cushing. Neurología. 2019;34:62–63.