The SARS-CoV-2 virus was first identified in December 2019 in the city of Wuhan, China. This novel betacoronaviridae has been related with several neurological symptoms and complication, as anosmia, headache, seizure and stroke.1 The relationship with stroke could be explained by coagulopathy and endothelial dysfunction and there is a theoretical risk for large-vessel stroke.2 We report a 70-years-old man with subacute encephalopathy due to a multiple brain acute vascular lesions presumably related with CoviD-19 vasculopathy.
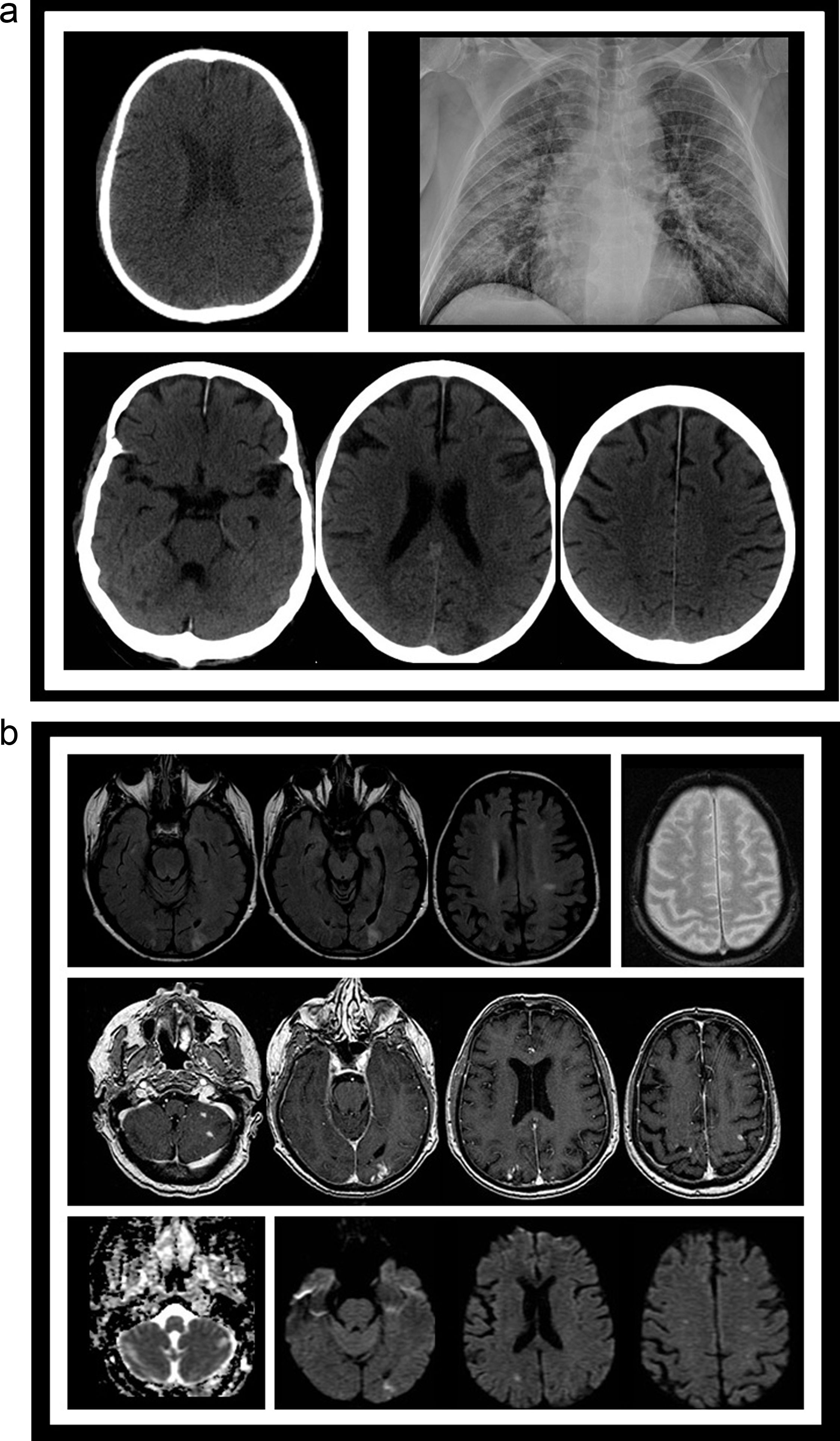
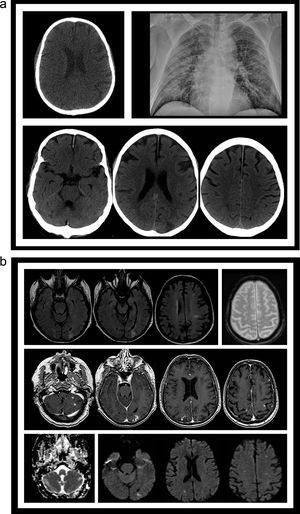
We present a 70-year-old man with a diagnosis of Bence-Jones light chain disease that was admitted to hospital at the end of March complained about fever and cough. The temperature was 38°C (100.4°F). Neurological examination at admission was unremarkable. A chest X-ray was performed, showing new bilateral infiltrates and PCR for SARS-CoV-2 was positive. The patient was started with hydroxychloroquine and support oxygen therapy for 7 days. Ten days later, the patient experienced began with an episode of subacute disorientation and conduct disorder, without any neurological focal symptomatology. We perform a An unenhanced cranial CT that showed showing multiple low attenuate hypodense brain and cerebellar lesions, and a brain MRI with angiographic sequence acquired a week later confirmed confirms multiple supra and infratentorial subacute ischemic lesions, without large and medium vessel occlusion or stenosis (Fig. 1a and b). An extended study that included transthoracic and transesophageal echocardiography, antiphospholipid antibodies, supra aortic arteries study was normal. Therefore, it was decided to start anticoagulant treatment, with a good evolution until the resolution of the clinical situation. Discussion
(a) CT image (A) from PET/CT scan evaluation for the light-chain disease showing no abnormality ten days before the onset of fever. Chest RX (B) showing bilateral lung infiltrates. Different slices from head CT (C) obtained after the patient developed neurological symptoms demonstrating several low attenuating lesions (arrows), both cortical and white matter locations. (b) Different sequences from a MRI study obtained a week after the start of the neurological symptoms. FLAIR slices (A), gradient-echo (B), postgadolinium injection 3D FSPGR T1-weighted slices (C), ADC map (D) and diffusion-weighted slices, showing several subacute small infarcts (arrows), with high signal in both T2 and DWI images, contrast enhancement, and decreased ADC values in some of them.
We present a patient with Bence-Jones light chain disease and CoviD19 that developed an encephalopathy due to multivascular acute lesions. We hypothesize that the lesions could be related with a SARS-CoV-2 induce rain vasculopathy. Is well known, that the ACE2 receptor allows the virus that causes COVID-19 to infect and destroy our cells.3 Brain capillary express ACE2 receptor.4 This could induce an inflammatory thrombogenic vasculopathy. This catastrophic microvascular injury syndrome mediated by activation of complement pathways and the associated procoagulant state could explain this findings.5 The microvascular injury could be also related with the high incidence of Post-intensive Care Syndrome in CoviD-19.6 We propose that every patient with encephalopathy, acute neurological non focal symptoms or post-intensive-care syndrome should be studied to rule out a microvascular damage.