Complex regional pain syndrome (CRPS) is characterised by the presence of pain accompanied by sensory, autonomic and motor symptoms, usually preceded by a lesion or immobilisation. The clinical course is disproportionate to the initial injury in intensity and in duration. Its distribution is regional, predominantly in limbs. It is classified as type I and type II, according to the absence or presence of nerve injury.
CasesWe present the cases of seven children, 6 girls and 1 boy, aged 7 to 15 years. Three had a history of previous trauma. In 5 cases, the symptoms were located in the lower limbs. Time to diagnosis was between 4 and 90 days. Three patients had clinical features of anxiety and depression. Imaging and immunological studies were performed to rule out differential diagnoses in all the children. Interdisciplinary treatment was performed with physiotherapy, psychotherapy, and gabapentin or pregabalin. All patients had a good clinical outcome, with no relapse in the follow-up period (between 4 and 30months).
ConclusionsCRPS is frequently unrecognised in children, leading to family anxiety and unnecessary para-clinical costs. Paediatricians and paediatric neurologists should be aware of this syndrome in order to avoid delay in diagnosis, unnecessary studies, and multiple visits to specialists, with a view to providing effective treatment.
El síndrome doloroso regional complejo (SDRC) se caracteriza por la presencia de dolor acompañado de síntomas sensoriales, autonómicos y motores. Es precedido habitualmente por una lesión o inmovilización. Su curso clínico es desproporcionado con respecto a la lesión inicial tanto en su intensidad como en su duración. Su distribución es regional, predominando en las extremidades. Se clasifica en tipo I y tipo II según ausencia o presencia de lesión nerviosa.
Casos clínicosSe presentan 7 casos clínicos, 6 niñas y un varón con SDRC tipo I, con edades comprendidas entre 7-15 años. Tres tenían antecedente de traumatismo previo. En 5 casos los síntomas se localizaron en miembros inferiores. La demora diagnóstica fue entre 4-90 días. Tres pacientes presentaron elementos de ansiedad y depresión. En todos se realizaron pruebas complementarias de imagen e inmunológicas para descartar diagnósticos diferenciales. Se realizó tratamiento interdisciplinario no farmacológico (fisioterapia y psicoterapia) y farmacológico con analgésicos mayores, gabapentina o pregabalina. Todos presentaron buena evolución, sin recidivas en el seguimiento que fue entre 4 meses y 2,5 años.
ConclusionesEl poco reconocimiento de este síndrome en niños, la ansiedad familiar que genera y los costos en paraclínica innecesaria, resaltan la importancia de su difusión entre pediatras y neuropediatras para favorecer su reconocimiento, evitar estudios innecesarios y múltiples consultas a especialistas que retrasan el diagnóstico y el inicio de un tratamiento efectivo.
In 1864, Mitchell, Morehouse, and Ken described what is known today as complex regional pain syndrome (CRPS) type II.1 Several other terms have been given to CRPS, including reflex sympathetic dystrophy and Sudeck atrophy for CRPS type I, and causalgia for CRPS type II.1 In 1995, a consensus was reached to group these entities under the name CRPS.2–4 CRPS is characterised by the presence of pain in association with sensory, autonomic, and motor symptoms. This pain is disproportionate to the initial lesion in terms of intensity and duration.2,4,7–9 Diagnosis, which relies on clinical observation and is made by exclusion, is based on the Budapest criteria proposed by the International Association for the Study of Pain (IASP) in 2003 and validated in 2010; these criteria are highly sensitive (0.99) and specific (0.68).2,4,9,10 To date, no complementary tests able to confirm a diagnosis of CRPS have been developed. Rather, these tests are ordered to rule out other possible diagnoses.8 CRPS is classified as type I or II according to presence or absence of a nerve lesion.1,2,4,7,9
The exact pathophysiological mechanism of CRPS type I is yet to be determined. Several peripheral nervous system (PNS), central nervous system (CNS), and local factors, along with genetic and psychological factors, have been suggested to be involved.2,4,7,9
CRPS type I is infrequently recognised in paediatric patients,2,3,5–8 which results in delayed diagnosis and late initiation of appropriate treatment.7
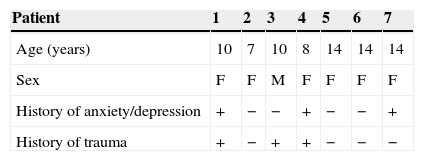
Clinical casesWe present 7 clinical cases of paediatric patients with CRPS type I. Population characteristics and clinical presentation are described in Table 1. Patients were predominantly female (6/7). Mean age was 11±4 years (range, 7-15 years).
Population characteristics and clinical presentation.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| Age (years) | 10 | 7 | 10 | 8 | 14 | 14 | 14 |
| Sex | F | F | M | F | F | F | F |
| History of anxiety/depression | + | − | − | + | − | − | + |
| History of trauma | + | − | + | + | − | − | − |
| Clinical presentation | |||||||
|---|---|---|---|---|---|---|---|
| Pain | + | + | + | + | + | + | + |
| Mechanical allodynia | + | − | + | − | − | − | − |
| Cold skin | + | + | + | + | + | + | + |
| Cyanosis | − | + | + | + | + | + | + |
| Functional weakness | + | + | + | + | + | + | + |
| Atrophy | − | + | + | − | − | − | − |
| Location | RUL | RLL | LLL | RLL | RLL | LLL | LUL |
| Diagnostic latency (days) | 15 | 90 | 90 | 10 | 4 | 90 | 90 |
| Follow-up (months) | 24 | 30 | 24 | 18 | 12 | 6 | 4 |
F: female; M: male; RUL: right upper limb; RLL: right lower limb; LUL: left upper limb, LLL: left lower limb.
The triggering factor, identified in only 3 children, was minor trauma: sprained ankle, mild knee trauma, and arm traction injury. None of them required immobilisation.
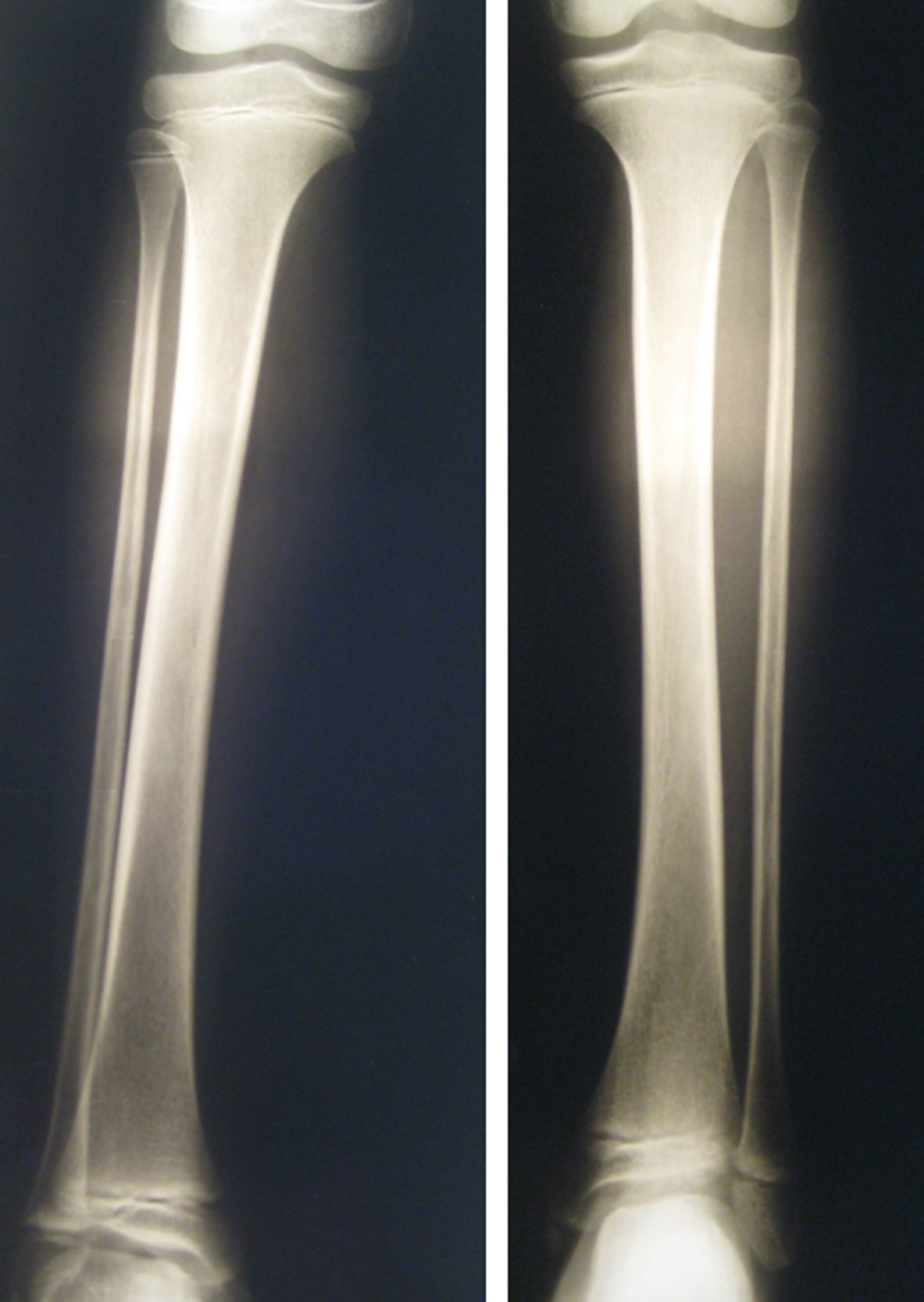
Pain, functional weakness, and cold skin temperature were present in all patients, and most exhibited cyanosis (6/7). Limb atrophy was seen in 2 patients in whom the syndrome was diagnosed late (Fig. 1).
Time elapsed from symptom onset to diagnosis of CRPS was 56±43 days (range, 4-90 days). In 4 children, the syndrome was diagnosed late (90 days after symptom onset). All patients were evaluated by several specialists before CRPS was considered as a possible diagnosis. Mean follow-up time was 16.9±9.8months (range, 4-30months).
Complementary tests were performed in all cases to determine pain aetiology. The first test performed was radiography of the affected limb; results at symptom onset were normal in all children. In 2 out of 4 patients with late diagnosis, a follow-up radiography showed bone demineralisation (Fig. 2). Five patients underwent a bone scintigraphy study; low tracer uptake was observed in 2, both of whom had a late diagnosis. Other tests performed were an MRI study of the affected limb (4 patients), electromyography and nerve conduction velocity (2), and echo Doppler (5). Furthermore, all patients underwent immune/inflammatory tests including a complete blood count, erythrocyte sedimentation rate, and tests for rheumatoid factor, antinuclear antibodies, anti-dsDNA antibodies, anti-neutrophil cytoplasmic antibodies, and anticardiolipin antibodies. Results from all additional tests were normal.
All children received high doses of weak analgesics (non-steroidal anti-inflammatory drugs) and strong analgesics (morphine or derivatives), and experienced no clinical improvement. Brachial plexus block was performed in one patient. As no response was achieved, the catheter was withdrawn after 48hours. After patients had been diagnosed with CRPS, gabapentin was administered to 5 patients at a dose of 30mg/kg/day, and pregabalin to 2 patients at a dose of 150-300mg/day. All patients were given physiotherapy, first with passive mobilisation and then with active mobilisation. Three children were treated with occupational therapy, and 4 with hydrotherapy. The 2 patients presenting allodynia underwent cutaneous desensitisation. Treatment with gabapentin or pregabalin plus physiotherapy lasted between 3 and 6 months. Two children with psychiatric comorbidities were treated with antidepressants, anxiolytics, and psychotherapy. Response was excellent in all patients. During the follow-up period, symptoms resolved and there were no cases of relapse.
DiscussionThe incidence rate of CRPS in adults ranges from 5 to 26 cases per 100000 people per year; however, its incidence in children is unknown.3,8 As our study shows, CRPS is much more common among preadolescent and adolescent girls; some series report percentages as high as 90%.7,9,11
The main symptom is pain that is disproportional to the initial trauma. Pain may also present after prolonged immobilisation or stressful events in up to 8% of cases, as described in the literature.3,12 Four of the 7 patients (57%) in our study had no history of trauma or immobilisation. This proportion is similar to those reported by other studies with paediatric patients in which the absence of a triggering event accounted for up to 48% of the cases.2,7
CRPS in adults evolves in 3 stages: (1) an acute stage, with pain, hyperalgesia, allodynia, oedema, erythema, and elevated skin temperature; (2) a dystrophic stage, with pain, muscle rigidity, and vasomotor and autonomic changes; and (3) an atrophic stage, in which pain lessens but patients show rigidity and cutaneous, muscle, and bone atrophy.3 However, paediatric CRPS does not follow this 3-stage pattern: cold skin temperature and cyanosis are more frequently reported than oedema and sweating,2,8,13 as was demonstrated by most cases in our series. Trophic changes, which are more frequent in adults,13 were observed in 2 children in our series, both of whom were diagnosed late. Although allodynia is a common symptom,2,8 it was present in only 2 of our patients.
Diagnosis is made by exclusion; additional laboratory and imaging tests are therefore needed to rule out such potential diagnoses as traumatic lesions, inflammatory diseases (osteomyelitis, juvenile rheumatoid arthritis), and tumours.2,7,8 Radiography, an imaging technique commonly used in children with CRPS, can rule out fractures and tumours. In this series, it was the first test to be ordered after symptom onset in all patients. Results were normal in all cases. Bone demineralisation may present in advanced stages,7 as in 2 of our patients with late diagnosis. Bone scintigraphy studies may yield normal results or display low tracer uptake; less frequently, they may show high tracer uptake, as occurs in adults.2,7,8 Normal results rule out osteomyelitis, some types of tumours, and stress fractures. The echo Doppler test must be performed when a thrombotic lesion is suspected.2 Inflammatory diseases can be ruled out by performing a complete blood count with erythrocyte sedimentation rate and tests for rheumatoid factor, antinuclear antibodies, anti-dsDNA antibodies, anti-neutrophil cytoplasmic antibodies, and anticardiolipin antibodies.2 Electromyography and nerve conduction velocity are recommended for a suspected diagnosis of neuropathic lesion.2
Treatment for CRPS type I is more effective in children than in adults.2 It is based on physiotherapy with coadjuvant occupational therapy, and achieves exceptional results.6-8,11,14 The treatment focuses on preserving limb function rather than just treating pain. Frequency, duration, and intensity of the treatment depend on the child; some cases require 6 to 7hours of treatment per day.8 Some authors have reported remission rates of more than 90% in patients completing 6hours a day of physiotherapy only.8,14 Physiotherapy and psychotherapy combined achieve no better results than physiotherapy alone.8,14 Transcutaneous electrical nerve stimulation (TENS) has been used in several case series as part of a multimodal treatment; however, its effectiveness is yet to be determined.8,11
This type of pain responds poorly to analgesics, as seen in our series. In fact, strong analgesics such as morphine are usually ineffective. Scientific evidence is insufficient to determine the effectiveness of non-steroidal and opiate analgesics for paediatric CRPS type I.8,11
Gabapentin has proved to be an effective and safe treatment option for neuropathic pain in CRPS, whereas there is no evidence regarding the effectiveness and safety of other antiepileptic drugs (carbamazepine, phenytoin).3,6,11 In our series, as in other studies, clinical response to gabapentin was highly satisfactory. Pregabalin was administered to 2 patients, who responded very well; however, other studies report lower efficacy.6,11
Some studies have documented good response to tricyclic antidepressants such as amitriptyline.6,11
In more severe cases, a nerve block may be necessary to lessen pain in order for patients to undergo physiotherapy.8 In our series, a brachial plexus block was performed in one patient before CRPS was diagnosed. No changes in symptoms and pain intensity were observed. As a result, the catheter was withdrawn 48hours later.
There is no evidence that other treatments used in adults (ketamine, anti-free radicals, calcitonin, biphosphonates, or topical anaesthetics such as capsaicin) are effective in paediatric patients.3
Spinal cord stimulation and sympathectomy have been used in some patients who did not respond to other treatments, as part of a multidisciplinary treatment and rehabilitation programme.8 However, experience with this treatment is insufficient in paediatric patients.15
Paediatric CRPS has a good long-term prognosis. The recurrence rate is higher in children than in adults, reaching 30% in some series; however, response to reinitiating treatment is excellent.6,8,13,14 So far, no relapses have occurred in our series.
Delays in diagnosis are a common feature in different published series. They result in delayed treatment initiation, slower recovery, and the need for more invasive techniques to manage pain.6,7,14
ConclusionsAccording to the literature, there are substantial differences between paediatric and adult CRPS cases. These can be seen in our series: predominance of female patients, disease most commonly affecting the lower limb, less marked neurological signs and symptoms, cold skin temperature in most cases, greater impact of psychological factors, absence of the 3 stages that characterise adult CRPS, better response to physiotherapy and occupational therapy, and excellent prognosis.2,5,7,8,13
Pain in paediatric patients is a source of great anxiety and has a negative psychological impact on both patients and their families. Doctors managing paediatric patients should be aware of this entity and the differences in clinical presentation between paediatric and adult CRPS in order to avoid unnecessary tests and delays in diagnosis and treatment.
Most data on CRPS type I come from studies in adults. Further research on paediatric cases is therefore necessary to deepen our knowledge of this entity. This will enable doctors to recognise CRPS and develop diagnostic and treatment protocols suitable for paediatric patients. We feel that our study provides valuable findings in this area.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pedemonte Stalla V, Medici Olaso C, Kanopa Almada V, Gonzalez Rabelino G. Síndrome doloroso regional complejo tipo i. Análisis de una casuística infantil. Neurología. 2015;30:347–351.