Spontaneous vertebral artery dissection (VAD) is a known cause of ischaemic stroke among young adults. Neck trauma and connective tissue diseases are associated factors.1,2
Sensorimotor radiculopathy secondary to local compression at spinal root level is a rare manifestation of VAD.3,4 We present the case of a patient with peripheral paralysis of the right arm due to an intramural haematoma in the right vertebral artery exerting pressure on the C5 and C6 roots.
Our patient was a 49-year-old man who was examined due to progressive proximal paralysis of the right arm. Two weeks before that, he had experienced cervical pain radiating to the right shoulder and arm, with no history of neck trauma or manipulation. Neurological examination revealed weakness of the right deltoid muscle (1/5) and biceps (3/5). Right-sided biceps reflex was absent, brachioradialis reflex was diminished, and triceps reflex was normal. Motor balance and sensitivity were preserved in the left arm and in both legs.
A needle electromyography showed a marked innervation deficit of the right brachioradialis, biceps, deltoid, and supraspinatus muscles. These findings were compatible with postganglionic neuropathic lesion of the proximal brachial plexus.
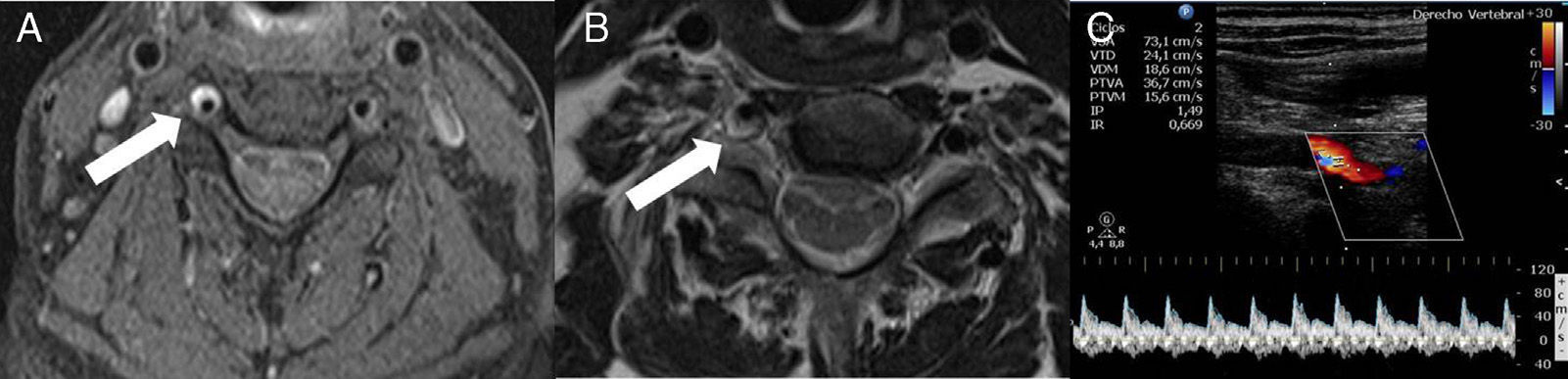
Fat-suppressed magnetic resonance imaging (MRI) of the neck showed a hyperintense crescent-shaped image in segments V1 and V2 of the right vertebral artery (Fig. 1) indicating an intramural haematoma secondary to arterial dissection. No relevant findings were observed in the brain MRI images; echo Doppler of extracranial vessels showed a biphasic flow in the V2 segment of the right vertebral artery. Pulsatility index was high but no intimal flap was detected.
Neck MRI axial images (A, B): fat saturated T1-weighted sequence (A) showing a hyperintense signal surrounding the right vertebral artery at the C5 level (arrow), which is compatible with intramural haematoma. The T1-weighted sequence (B) shows compression of the C5 root (arrow) due to expansion of the haematoma. Colour Doppler ultrasound of the extracranial portion of the right vertebral artery (C) shows a biphasic flow in the V2 segment and increased pulsatility. No flow is observed in segment V1.
The patient began treatment with antiplatelet drugs and physiotherapy, which improved symptoms after a few weeks. In the follow-up visit 2 months later, he was asymptomatic.
Cervical artery dissections represent 2% of all strokes and up to 20% of all thromboembolic strokes occurring in young patients. Vertebral artery dissection has an approximate incidence of 1.5 cases per 100000 inhabitants. It can be spontaneous, secondary to recent neck trauma or manipulation, or associated with diagnosed or subclinical connective tissue disease2 or with recent infections.1,5 Dissection most commonly originates in the V3 segment,6 followed by V1 and V2 segments.
The most common symptoms include vertigo, headache, and neck pain; the least frequent are ischaemic stroke, transient ischaemic attacks, and subarachnoid haemorrhage.2 In rare cases it manifests as peripheral neuropathy and the most commonly affected nerve root is C5.
Arterial dissection occurs when blood enters the tunica media and the haematoma expands, causing the arterial wall to dissect. Compression of motor roots due to haematoma expansion within wall layers, or to impaired perfusion in the vasa nervorum causing radicular ischaemia, are the most widely accepted hypotheses to explain radiculopathy secondary to VAD.
Before non-invasive techniques such as MRI and Doppler ultrasound were used, arteriography was the technique of choice. MRI is currently a very sensitive method that enables identification of intramural haematoma, as well as the arterial lumen decreased by stenosis, in most cases.7 In addition, Doppler ultrasound can be a very useful tool for measuring flow by means of high resolution images,3 and to stratify the risk of ischaemic recurrence.8
Anticoagulants and antiplatelet drugs are the treatment of choice to prevent dissection progression and thromboembolic events associated with VAD.9 When medical treatment fails, intravascular treatment represents a safe and effective therapeutic option.10,11 The prognosis for radiculopathy secondary to VAD seems positive according to published studies12; resolution of symptoms and abnormalities on the vascular wall is frequent.
Please cite this article as: Llull L, la Puma D, Falgàs N, Renú A, Iranzo A. Radiculopatía compresiva C5-C6 secundaria a disección espontánea de la arteria vertebral derecha. Neurología. 2016;31:61–62.