Guillaume–Barré syndrome (GBS) is an acute immune-mediated disease affecting the peripheral nervous system. It can be divided into different subtypes according to clinical, immunological, neurophysiological, and pathological criteria.1
GBS includes at least 3 patterns: acute inflammatory demyelinating polyneuropathy (AIDP), acute motor axonal neuropathy/acute motor-sensory axonal neuropathy (AMAN and AMSAN), and Miller Fisher syndrome.
AMAN is a pure motor form of GBS which is frequently associated with the presence of certain anti-ganglioside antibodies and preceded by an infection with Campylobacter jejuni. This clinical form may present clinical characteristics that delay diagnosis.
We present the case of a man, aged 29, who came to the emergency department due to acute tetraparesis predominantly affecting the upper limbs and associated with back pain. The patient reported having had diarrhoea one week before. He claimed not to have experienced autonomic dysfunctions or sensory disorders. The neurological examination revealed normal reflexes and asymmetric tetraparesis predominantly affecting right-sided distal regions and the upper limbs.
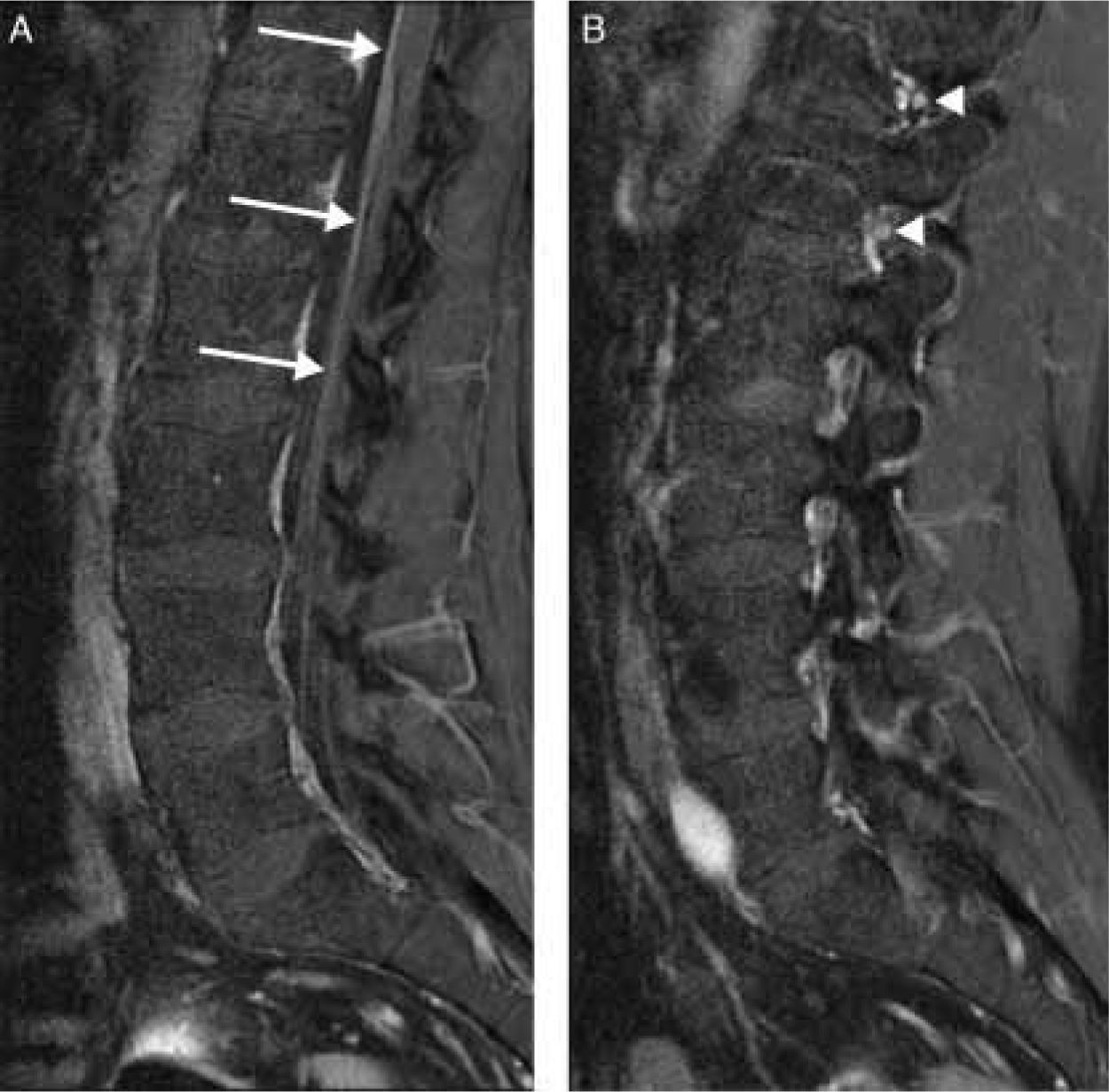
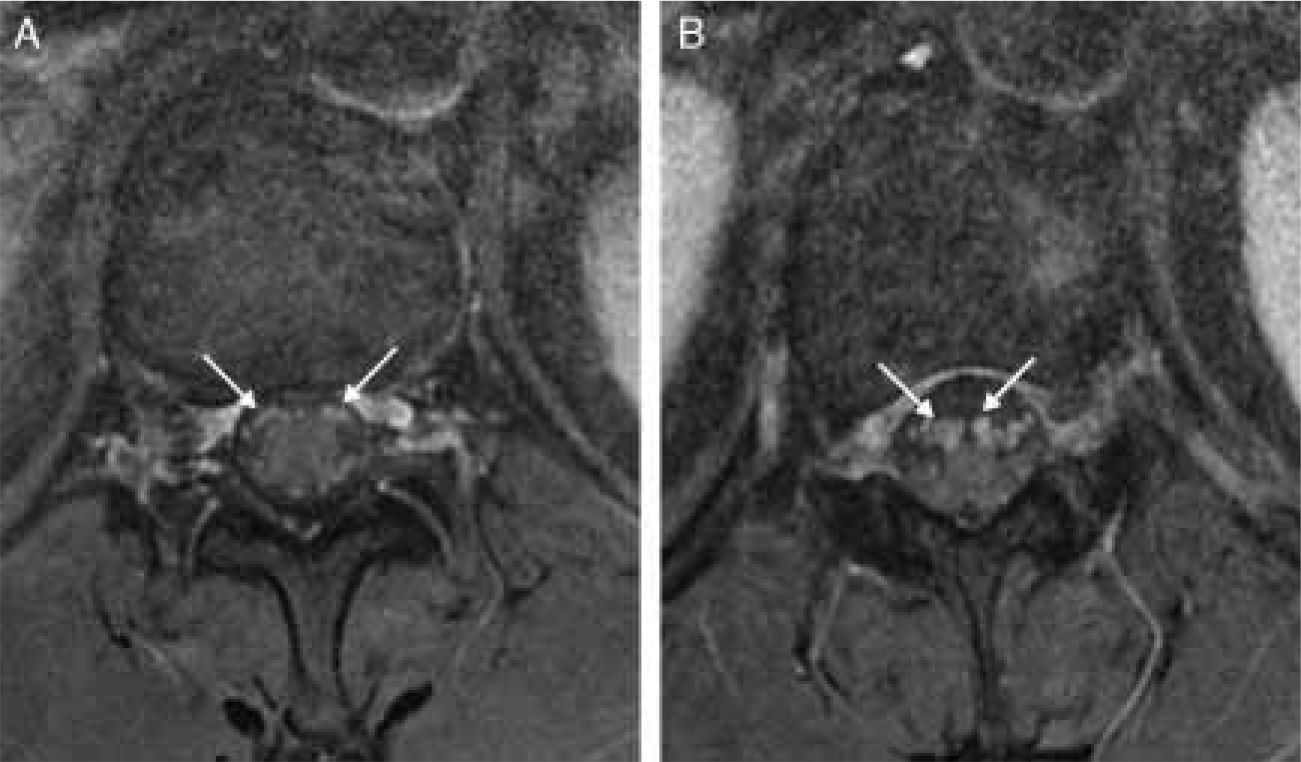
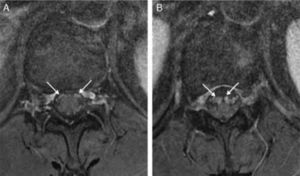
Contrast-enhanced MR imaging of the spinal cord revealed enhancement limited to the anterior nerve roots (Figs. 1 and 2).
The patient's Achilles reflex subsequently disappeared. The CSF study showed albuminocytological dissociation. The neurophysiological study revealed a decrease in motor evoked potential amplitude with no changes in velocity or latencies and normal sensory nerve conduction. Conduction block was not detected. F-waves displayed normal persistence and latency in the upper and lower limbs. The needle study showed abundant spontaneous muscle activity in proximal and distal muscles of the upper and lower limbs with a reduced recruitment pattern. These neurological findings were compatible with exclusively motor and axonal impairment. Serology tests for C. jejuni were positive (1/1000). Tests were negative for anti-ganglioside antibodies GM1, GM2, GD1a, GT1B, and GQ1b. The patient was diagnosed with AMAN and treated with immunoglobulins (2g/kg body weight), after which symptoms improved.
Three months after onset of symptoms, he presented distal weakness predominantly affecting the upper limbs (4/5 on the Medical Research Council scale).
AMAN is a form of GBS that exclusively affects motor function of the peripheral nervous system and causes axonal impairment while sparing myelin.1 It seems that there is a relationship between AMAN and a prior infection with C. jejuni. This bacterial species has surface lipooligosaccharides that work as antigens and possess structures similar to those of some peripheral nerve gangliosides.2 In these cases, neurophysiological studies show motor impairment with signs of axonal damage. However, some authors, such as Berciano et al., have shown that the pathological basis of this disease is demyelination even if neurophysiological studies are unable to demonstrate this finding in some cases. Demyelination is primarily radicular with secondary wallerian degeneration.3
Different studies have shown contrast uptake by nerve roots in acute polyradiculoneuropathies4–8 or even by cranial nerves.4 This uptake seems to be due to the absence of perineurium in preforaminal nerve roots and to a compromised blood–nerve barrier.9 It has been suggested that this uptake is related to more severe pain and a poorer prognosis. Doctors decided to perform an MRI scan due to the initial asymmetry of the symptoms and because reflexes that were initially present disappeared during the course of the disease. The presence of normal reflexes or even hyperreflexia has been described in other patients with AMAN.10 Although the MRI is not necessary to establish a diagnosis of AMAN or others forms of GBS, it may be useful for differential diagnosis of acute tetraparesis.
Please cite this article as: Gutiérrez-Gutiérrez G, Ibáñez Sanz L, Lobato Rodríguez R. Captación de raíces anteriores en la neuropatía aguda motora axonal. Neurología. 2014;29:59–61.