Transcatheter aortic valve implantation (TAVI) is the treatment of choice in patients with severe, symptomatic aortic stenosis and presenting high surgical risk.1 Stroke is a frequent complication that significantly increases mortality, occurring within 24hours of the procedure in up to 50% of cases.2,3 Mechanical thrombectomy via the endovascular route is the gold standard treatment for acute large cerebral artery occlusion; different techniques have been developed that combine the use of retrievable stents (stent-retriever/stentriever) and aspiration catheters.
We report the first case of extraction of a fragment of a bioprosthetic heart valve, which had migrated to the middle cerebral artery (MCA) in the context of TAVI-related periprocedural stroke. Thrombectomy was performed with the Y-configuration double stent retriever technique.
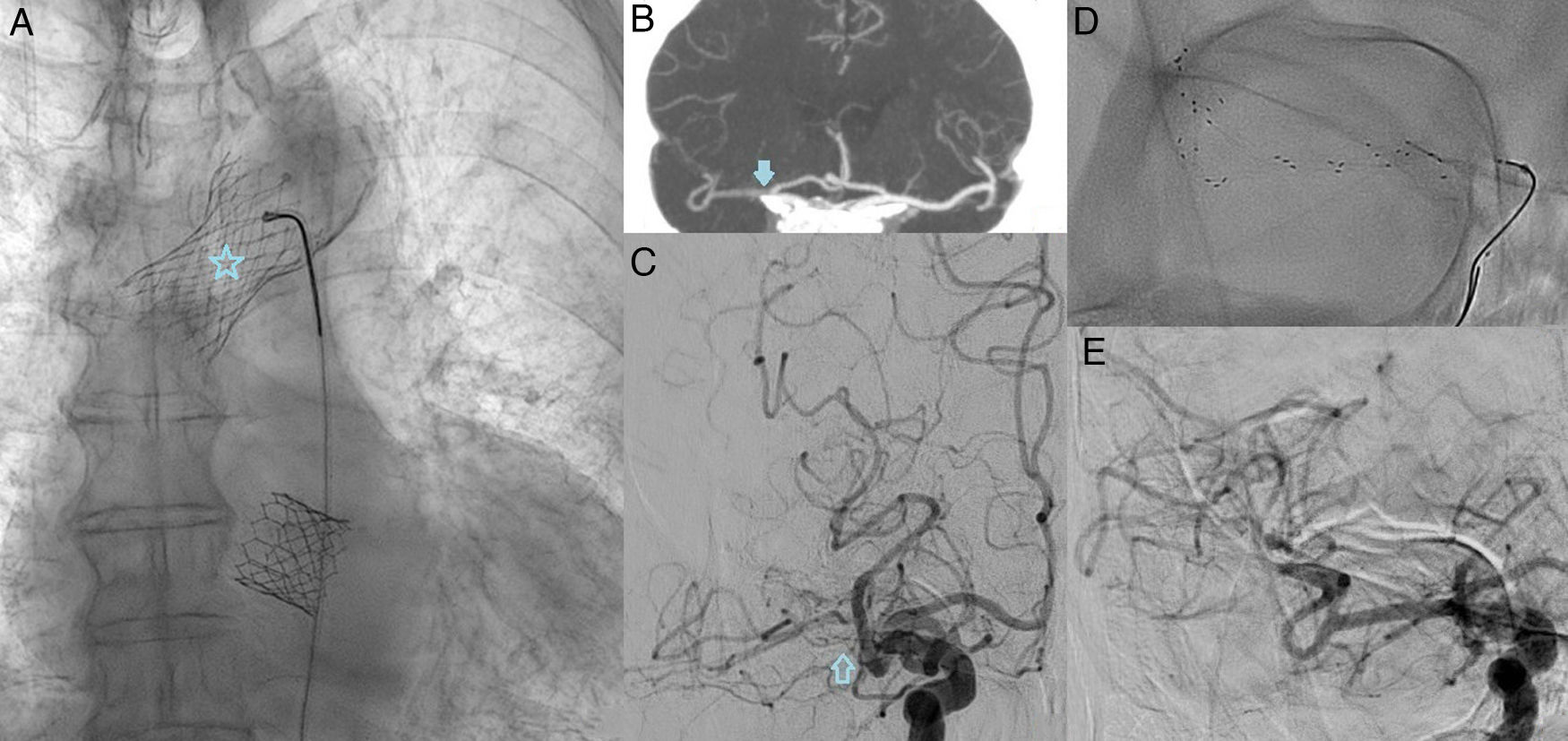
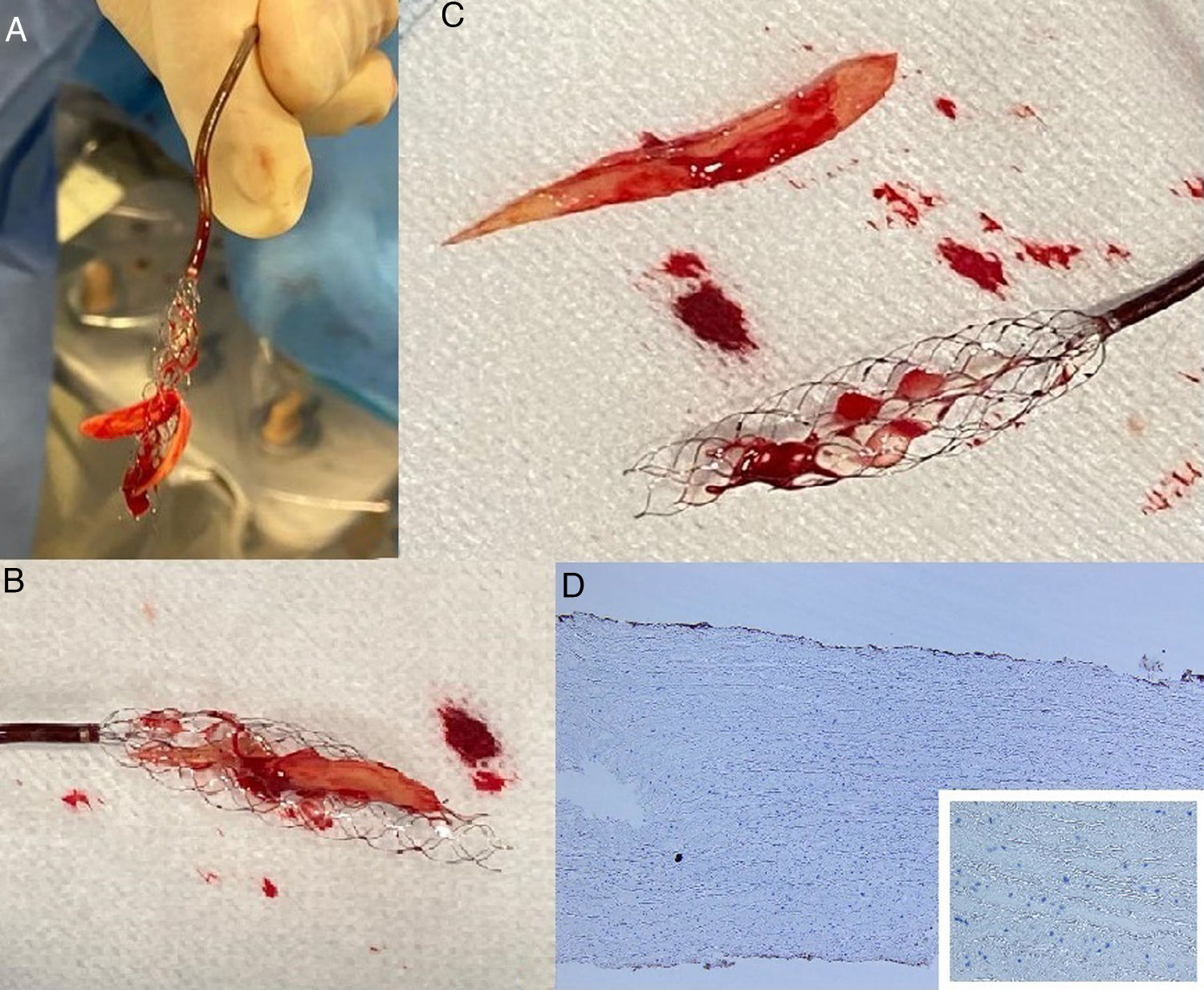
Our patient was an 83-year-old man with history of dyslipidaemia, arterial hypertension, and chronic kidney disease who was independent for daily living activities. He was admitted to our hospital due to acute heart failure secondary to 2 aortic lesions, with moderately reduced left ventricular ejection fraction (43%). The patient underwent endovascular treatment following heparinisation. During TAVI, the self-expanding bioprosthesis migrated to the ascending aorta; a second, balloon-expandable prosthesis was therefore implanted, with the first remaining lodged in the aortic arch (Fig. 1A). After extubation, the patient presented left faciobrachiocrural hemiparesis, left hemihypoaesthesia, and left homonymous hemianopsia with anosognosia, scoring 16 on the National Institutes of Health Stroke Scale (NIHSS). A CT scan revealed presence of contrast inside blood vessels and in the brain parenchyma; the contrast medium had been administered during TAVI. As a result, the Alberta Stroke Programme Early CT (ASPECT) score could not be established. CT images revealed engorgement of the parenchyma of the right hemisphere and asymmetric parenchymal enhancement, with reduced uptake in the right caudate nucleus and putamen as compared to the left; this may correspond to an ASPECT score of 8. CT angiography revealed asymmetric repletion of the M1 segment of the MCA bilaterally, which was less marked in the right vs the left M1 segment (Fig. 1B), corresponding to occlusion in digital subtraction arteriography images (Fig. 1C). With the patient under local anaesthesia and via right femoral artery access, a Neuron™ MAX 088 reperfusion catheter (6F long sheath/90cm long) (Penumbra; Alameda, CA, USA) was placed in the cervical segment of the right internal carotid artery as a guide catheter. Thrombectomy was performed with the SAVE technique: we used a Solitaire® 6×40mm stent retriever (Medtronic; Fridley, MN, USA) and a Sofia™ 5F aspiration catheter (MicroVention; Aliso Viejo, CA, USA), which was placed in contact with the proximal face of the embolus. Carotid flow was reversed with aspiration through the guide catheter. The procedure was unsuccessful after 3 passes in both segments of the MCA. Finally, we applied the Y-configuration double stent retriever technique: the Solitaire® 6×40mm stent was placed in the inferior division of the MCA; after crossing the mesh with a microguidewire and a microcatheter, a second Solitaire® 4×40mm stent retriever (Medtronic; Fridley, MN, USA) was deployed in the superior division, with the proximal half of the 2 stents overlapping in the main trunk (Fig. 1D). The 5F catheter was advanced to the MCA, and aspiration was started with both the 5F catheter and the guide catheter. Both stents were removed at the same time, together with the intermediate catheter (dual stent retriever technique combined with distal and proximal aspiration, or dual SOLUMBRA technique), achieving recanalisation of the occluded artery (Fig. 1E), with a modified Treatment In Cerebral Infarction (mTICI) score of 2c. The embolus was trapped between the stents; it was an elongated, flat piece of solid biological tissue (Fig. 2). Time between TAVI and MCA recanalisation was approximately 6hours. The patient presented a neurological improvement immediately after thrombectomy, but left brachiocrural hemiparesis (4/5) and left hemihypoaesthesia persisted (NIHSS=5). A head CT scan performed 24hours later revealed hyperdensity in the sulci of the right convexity, compatible with contrast extravasation and/or subarachnoid bleeding, with no evidence of corticosubcortical or deep brain hypodensities associated with established ischaemic lesions. The patient died 48hours after the procedure due to severe bradycardia and cardiac arrest (cardiopulmonary resuscitation was unsuccessful), which were attributed to the aberrant position of the migrated prosthesis. According to a histopathological study, the material extracted during thrombectomy was bovine pericardium (Fig. 2D).
(A) Chest radiography (AP view) performed after implantation of the second prosthetic valve, showing the first bioprosthesis lodged in the aortic arch (star). (B) CT angiography of the circle of Willis (coronal view, maximum intensity projection), showing a filling defect in the M1 segment of the right MCA (arrow). (C) Digital subtraction angiography (AP view), confirming an occlusion in the right MCA (hollow arrow). (D) Fluoroscopy (AP view) showing the Y-configuration double stent retriever technique at the bifurcation of the MCA. (E) Digital subtraction angiography (AP view) performed after the procedure, showing complete recanalisation of the right MCA. AP: anteroposterior; CT: computed tomography; MCA: middle cerebral artery.
TAVI-related periprocedural stroke is frequently associated with embolism during the procedure. The most frequent causes are atheromas or calcium emboli originating at the native valve, aorta, or left ventricle; thromboemboli generated by manipulation of guidewires, catheters, and angioplasty balloons; prosthetic valve fragments; and air bubbles.3–5 De novo atrial fibrillation and persistent intraprocedural hypoperfusion also play a role, although they are less frequent.5 To date, only one case has been reported of extraction of a small fragment of a valve bioprosthesis, which was implanted several years earlier.6 In our patient, the second bioprosthesis was put in place by passing a catheter through the first prosthetic valve, leading to its rupture and the migration of a fragment to the right MCA, lodging at the bifurcation. During thrombectomy, several stent passes were performed, without success, possibly due to the stent’s inability to grip the embolus. Aspiration was also unsuccessful, as the large, solid, flat, and partially occlusive embolus prevented us from generating sufficient negative pressure through the catheter to aspirate it.
Evidence from several recently published case series supports the efficacy and safety of using 2 stent retrievers simultaneously as a rescue procedure after failure of standard mechanical thrombectomy in patients with occlusions of artery bifurcations caused by solid emboli.7,8 Two strategies have been described for positioning the stents: 1) the parallel double stent retriever technique, in which 2 microcatheters are placed, with one in each branch of the bifurcation, and 2 stents are deployed simultaneously, with the proximal half of one stent remaining adjacent to the proximal half of the other stent in the main trunk; and 2) the Y-configuration double stent retriever technique, in which one stent is deployed in one branch and then a microcatheter crosses the first stent and places the second stent in the other branch, with the proximal half of both stents overlapping in the trunk.9,10 The first technique increases radial force and the surface of interaction between the stent and the embolus, which in turn increases the risk of endothelial damage.10 The second technique, which is somewhat more complex as it involves passing through a deployed stent, may achieve greater extraction force as the stents act as a tweezer. Both techniques may also involve aspiration with an intermediate catheter, similarly to the combined strategies currently used.11 In our patient, the context of TAVI-related periprocedural stroke and the CT images and angiography findings after successive passes suggested presence of a mobile, solid embolus lodged at the bifurcation, requiring the use of 2 stents for extraction. The Y-configuration double stent retriever technique successfully extracted the embolus.
This case underscores the importance of thorough examination of radiological images. Proper analysis of radiological and clinical data will help us to determine the type of thromboembolic material, with a view to establishing the most appropriate strategy for fast, safe, and complete extraction.
Please cite this article as: Martínez González JP, Guerrero Vara R, Medina Iglesias V, Branera Pujol J, Camps Renom P. Doble stentriever para recanalización de la arteria cerebral media ocluida por un émbolo inusual. Neurología. 2022;37:403–405.