Chronic subdural haematoma (CSDH) represents a clinical challenge due to its high recurrence rate. Endovascular middle meningeal artery embolisation (eMMAE) has emerged as an alternative for those patients presenting health problems or multiple recurrences of CSDH. Despite several encouraging reports, the safety profile, indications, and limitations of the technique are not clearly established.
DevelopmentThis study aimed to evaluate the current evidence on eMMAE in patients with CSDH. We performed a systematic review of the literature, following the PRISMA guidelines. Our search yielded a total of 6 studies, in which a total of 164 patients with CSDH underwent eMMAE. The recurrence rate across all studies was 6.7%, and complications occurred in up to 6% of patients.
ConclusionseMMAE is a feasible technique for treating CSDH, with a relatively low recurrence rate and an acceptable rate of complications. Further prospective and randomised studies are needed to formally establish a clear profile of the safety and effectiveness of the technique.
Dadas las altas tasas de recurrencia, el hematoma subdural crónico (HSDC) es una condición que supone un reto para el clínico. La embolización endovascular de la arteria meníngea media (EeAMM) ha surgido como una alternativa para aquellos pacientes con problemas de salud o con varias recurrencias de su HSDC. A pesar de la publicación de algunos artículos prometedores referentes a esta técnica, el perfil de seguridad, las indicaciones y las limitaciones no están claramente establecidas.
DesarrolloNuestro objetivo es evaluar la evidencia actual sobre la EeAMM en el HSDC. Se realizó una revisión sistemática de la literatura según las guías PRISMA. Nuestra búsqueda arrojó un total de 6 estudios, en los que 164 pacientes con HSDC se sometieron a EeAMM. La tasa de recurrencia entre todos los estudios fue del 6,7% y se produjeron complicaciones en hasta el 6% de los pacientes.
ConclusiónLa EeAMM es una técnica factible en el tratamiento del HSDC con una tasa de recurrencia relativamente baja y tasas aceptables de complicaciones. Se necesitan más estudios prospectivos y aleatorizados para establecer formalmente un perfil de seguridad claro y su efectividad.
Chronic subdural haematoma (CSDH) is defined as a collection of blood degradation products in the subdural space, between the surface of the brain and the dura mater.1 While CSDHs can be asymptomatic, when they increase in volume they can cause a mass effect on the cerebral cortex, resulting in focal neurological signs.2 Because the compliance of the brain parenchyma decreases with age, these haematomas are more common among older individuals or those with some degree of cerebral atrophy.3 With population ageing in Europe and the increased use of antiplatelet and anticoagulation drugs, CSDH is expected to be the most frequent reason for emergency neurosurgery by 2030.4
Classically, the condition is treated with urgent surgical evacuation via one or 2 burr holes.1 While this procedure can alleviate the mass effect of the haematoma almost instantly, it may not be able to interrupt the pathophysiological mechanisms that lead to CSDH.5 Therefore, despite being considered a simple procedure, burr-hole evacuation is associated with a considerable rate of CSDH recurrence, which reaches 30% according to some authors.3,6,7 In patients presenting recurrence of haematoma, repeated interventions are associated with a progressive increase in the likelihood of poor prognosis, particularly given the frailness associated with older age.2,8,9
In 2000, Mandai et al.10 described the successful treatment of recurrent CSDH with a technique involving endovascular embolisation of the middle meningeal artery (MMA). Selective embolisation of the dural branches can block the mechanism causing CSDH recurrence.11,12 Since then, isolated case reports and small series have demonstrated the effectiveness of the technique in patients with CSDH.13–16 However, the possibility of publication bias and the heterogeneity of the techniques used make it a challenge to determine the true therapeutic value of this procedure.
In the light of the above, we considered it necessary to conduct a systematic review of the current literature. The objective of this study is to determine the effectiveness of endovascular embolisation in treating CSDH, the pathophysiological basis of the treatment, its safety profile and associated rate of complications, and long-term outcomes.
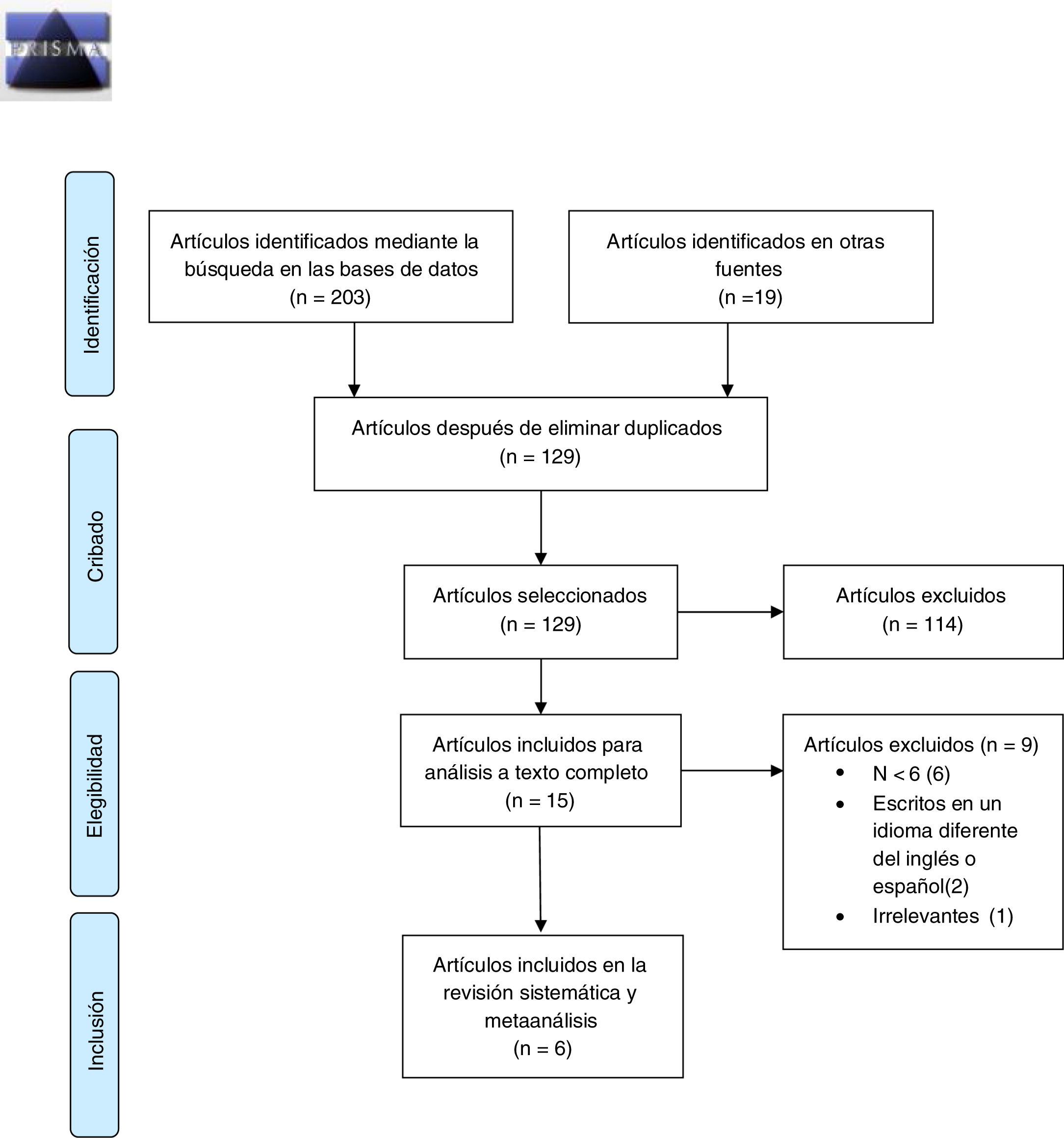
MethodsWe conducted a systematic review of the literature, including prospective studies (with or without randomisation) and retrospective case series of patients with CSDH (recurrent or otherwise) treated with selective embolisation of the MMA. We searched the PubMed and MEDLINE databases for articles containing combinations of the following MESH terms: subdural hematoma, hematoma, embolization, meningeal artery, endovascular, and recurrence. The studies included in the review were identified and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.17
We searched for studies published in English or Spanish between 2000 (when selective embolisation of the MMA to treat CSDH was first described) and September 2019. To mitigate the risk of publication bias, we excluded case reports and series of 5 or fewer patients from the analysis.
The search was performed independently by 2 researchers (RMP and NR); 2 researchers (RMP and AT) critically analysed potentially eligible articles and extracted relevant data after reading the full texts of the selected articles. We gathered data on study characteristics (prospective, retrospective, case series, cohort study, case-control study), the mean age of patients, sample size, the embolisation material used, whether CSDH was recurrent or non-recurrent, and the rates of recurrence and complications. Any disagreement between the researchers responsible for extracting data was resolved by consensus.
ResultsThe initial search yielded 222 results (Fig. 1). After the exclusion of duplicate articles and an initial screening, 15 articles were read in full text and analysed in detail; of these, 6 met the inclusion and exclusion criteria and were considered eligible for inclusion in the analysis (Table 1).11,18–22 Two of the included articles were non-randomised prospective studies employing historical series of patients treated with burr-hole evacuation as control groups,19–21 and the remaining 4 were retrospective series of patients with CSDH undergoing endovascular embolisation.11,18,20,22
Flow diagram as specified by Moher et al.17
Summary of the studies included in the qualitative analysis, showing indications for endovascular embolisation and treatment outcomes.
| Country | Type of study | No. patients | Age (mean) | Indication | Follow-up (months) | Recurrence (%) | Complications (%) | |
|---|---|---|---|---|---|---|---|---|
| Waqas et al.,18 2019 | USA | Retrospective case series | 8 | 63 | Recurrence: 2; primary treatment: 6 | > 2 | 0 | 0 |
| Saito et al.,11 2019 | Japan | Retrospective case series | 8 | 79 | Recurrence | 28.3 | 12.5 | 0 |
| Link et al.,20 2019 | USA | Retrospective case series | 49 | 69 | Recurrence: 42; primary treatment: 8; prophylaxis: 10 | NR | 8.1 | 0 |
| Ban et al.,19 2018 | Korea | Non-randomised prospective study | 72 | 69 | Primary treatment | > 6 | 6.9 | 0 |
| Kim,21 2017 | Korea | Non-randomised prospective study | 20 | 74 | Recurrence or high surgical risk | NR | 1.3 | 10 |
| Ishihara et al.,22 2007 | Japan | Retrospective case series | 7 | NR | Recurrence | > 15 | 0 | 0 |
| 164 | 69.8 | 6.70731707 | 6% |
NR: not reported.
The selected studies included a total of 164 patients, with a mean age of 69.8 years. The most frequent indication for endovascular treatment was recurrence of CSDH, although there were also cases in which the procedure was the primary treatment (with no previous surgical intervention).18,20,21 Four studies reported the duration of follow-up, which ranged from 2 to 28.3 months.11,18,19,22
The mean recurrence rate was 6.7% (range, 0%-12.5%). Studies with longer follow-up periods report higher rates of recurrence.11,19 Only Kim21 reports complications associated with MMA embolisation, although the type of complications is not indicated. Overall, complications were reported in 6% of patients. Only one study reports patient deaths during the follow-up period.
DiscussionPresent situationThe literature on the surgical outcomes of MMA embolisation to treat CSDH is scarce, and mainly includes case reports and clinical series lacking randomisation or long-term follow-up. These preliminary results are encouraging in that the endovascular procedure shows lower rates of recurrence than those reported for the invasive surgical treatment, and lower rates of complications.
Among the studies reviewed, only 2 were prospective19,21; neither of these was randomised. Therefore, it is difficult to evaluate the true role of endovascular treatment compared to the natural history of CSDH in patients not requiring emergency burr-hole evacuation. A randomised, prospective clinical study is currently underway to evaluate the effectiveness and safety profile of endovascular treatment of CSDH.23 Until that study is published, we may only infer conclusions from previous research. With regard to non-controlled clinical studies and to case reports, authors are more likely to publish positive findings, and to provide an incomplete summary of complications. Another limitation of this systematic review is the heterogeneity of the studies included11,18–22: differences in the indication for the treatment, the techniques used, and the duration of follow-up periods further hinder analysis. Despite all these limitations, our comprehensive review of the available literature does indicate a certain consensus and trends that constitute the pillars of future clinical research into the treatment of CSDH with endovascular embolisation.
Indications, effectiveness, and safety profileThe complex pathophysiological processes involved in the development and progression of CSDH begin with inflammatory processes and the response to an external insult, such as head trauma, even in minor cases.19 Furthermore, the separation of the dura mater from the cerebral cortex can damage vascular (mainly venous) structures located between the dura mater and the cortex.24–26 Inflammatory processes induce the formation of granulation tissue and macrophage proliferation, leading to the proliferation of vascular membranes around the haematoma.26–28 Simultaneously with the formation of this membrane, local inflammation leads to fibrinolysis of the haematoma,29 which increases the production of angiogenic factors, leading to bleeding and microfiltration of small capillaries in the membranes covering the CSDH.24
Various non-surgical treatments based on these pathophysiological mechanisms have been proposed, which have shown limited effects for a small number of patients.30–33 However, burr-hole evacuation continues to be the treatment option of first choice in most cases.9
MMA embolisation has recently emerged as an alternative to surgery in patients with recurrent CSDH.10,13–16,22 The MMA is a branch of the internal maxillary artery, and supplies the frontal, temporal, and parietal bones and the dura mater in these areas. Several advanced imaging and microbiological studies have found evidence that the fibrovascular membranes of the CSDH, which are responsible for the perpetuation and recurrence of the haematoma, are supplied by meningeal branches, primarily those arising from the MMA.11,12,19,34,35 Therefore, the aim of embolisation of MMA branches is to devascularise these membranes in order to tip the balance between the production and reabsorption of the haematoma towards reabsorption, leading to the subsequent resolution of the haematoma.5 Based on the initial positive results, endovascular treatment was soon indicated as the primary treatment for patients with CSDH (with no previous surgical evacuation) and for patients presenting high risk for surgery and general anaesthesia.9,19–21 Nonetheless, we do not currently know the true safety profile of the treatment or which patients stand to benefit the most.36
The most comprehensive study conducted to date is that published by Ban et al.19 The authors compare the outcomes from a prospective series of 72 patients with CSDH treated with endovascular embolisation against a historical series of patients from the same hospital who received the conventional treatment (burr-hole evacuation) or conservative management. These authors report favourable outcomes for endovascular embolisation of the MMA, with a success rate of 99% at 6 months, compared to 82% and 17% for burr-hole evacuation and conservative management, respectively. The prospective series by Kim21 shows similar results, with a significantly lower rate of recurrence in patients receiving the endovascular treatment than in those undergoing burr-hole evacuation (34% vs 5%). A recent meta-analysis reported that the rate of recurrence was nearly 10 times higher in patients undergoing surgical treatment.37
In any case, the definitions of success and recurrence vary between studies, and are often confusing. For example, Waqas et al.18 report that the endovascular technique was completely successful as no recurrences were observed during follow-up, despite the fact that resolution of the haematoma was partial in 2 of the 8 patients included and complete in only 3 patients.18 Ban et al.19 define treatment success as the absence of recurrence at 6 months. Several of the studies reviewed also present certain asymmetries in the baseline characteristics of the patient samples,19,21 particularly with regard to the percentage of patients receiving antiplatelet treatment and the percentage with bilateral haematomas. Due to this heterogeneity, the results should be interpreted with caution. Similarly, follow-up periods vary greatly between studies and are not always reported; in some cases, follow-up periods are insufficient, particularly for the purpose of analysing rates of recurrence.20,21 For instance, Waqas et al.18 followed up their patients for a minimum of 2 months. While the methodology may be appropriate from a statistical perspective, it is not suitable for evaluating CSDH recurrence, as recurrence most frequently occurs in the first 6 months.38
A particularly striking detail was the low rate of complications associated with endovascular embolisation (6%). In fact, complications directly linked to the procedure were only reported by Kim,21 in 2 patients. This finding seems doubtful, especially if we take into account the rate of complications, which even in patients undergoing diagnostic angiography studies reaches 2.6% in some studies,39,40 and the fact that mortality rates among patients with CSDH are 32% at 30 days and 26.3% at 6 months.41,42 This disparity may be explained by the short follow-up period or the inherent risk of publication bias. For instance, it is striking that Link et al.20 report a mortality rate of 6%, but do not account for these deaths as complications or mortality related to the procedure as the patients died after the first 30 days.
Technical properties, advantages, and limitations of endovascular embolisation of the middle meningeal arteryOne finding that does appear consistent is that the benefit of the endovascular treatment, insofar as its therapeutic effect is based on reducing the supply to and production of the CSDH, only becomes clinically and radiologically apparent after a certain period of time. Ban et al.19 treated 27 asymptomatic cases of CSDH of over 1 cm thickness. At 6 months of follow-up, haematoma had fully resolved in 97.8% of patients.19 On the contrary, burr-hole evacuation can alleviate the mass effect immediately.1 Therefore, it seems logical to consider that endovascular embolisation of the MMA alone may not be the best treatment option in patients displaying a considerable mass effect and rapidly progressive neurological impairment; other more effective techniques would be needed in the short term, such as burr-hole evacuation. However, MMA embolisation can be particularly beneficial for neurologically stable patients presenting recurrence of CSDH.21,43 In order to reduce the risk of recurrence, endovascular embolisation of the MMA has also been performed as prophylaxis in patients who have previously undergone surgical evacuation of CSDH.18,20
Furthermore, the procedure may be performed under light sedation if polyvinyl alcohol is used as the embolic agent; this reduces the risk of complications of anaesthesia in patients with multiple comorbidities.5,20,21,43 Another advantage of this technique over conventional surgery is the fact that there is no need for patients undergoing the procedure to reverse anticoagulation treatment: these patients may continue to receive anticoagulants and antiplatelets.5 In the study by Ban et al.,19 the majority of surgery-related complications were caused by ischaemic events, which presented more frequently in patients who had stopped receiving anticoagulation.
OutlookThere is a clear need for an evidence-based evaluation of the true effectiveness of MMA embolisation and its potential complications and limitations.36 It is also necessary to establish which patients will benefit most from the technique, with limited risk.
With the introduction of endovascular therapy, the treatment of CSDH has become multidisciplinary: rather than following a “one size fits all” approach, we must seek to select the most appropriate treatment in each case, taking into account the personal situation of each patient. The numerous variables at play and the advanced age and potential comorbidities of this patient group make it difficult to establish homogeneous clinical guidelines; rather, each case must be evaluated on an individual basis. In any case, endovascular treatment paves the way for effective treatment of CSDH, which we hope will be further clarified in the near future.
ConclusionWhile burr-hole evacuation remains the gold standard treatment for CSDH, the findings of our literature review suggest that embolisation of the MMA is a valid treatment approach in selected cases. Pending the completion of randomised clinical studies, and despite the possibility that some of our conclusions may be subject to publication bias, the clinical series available indicate relatively low rates of recurrence and complications.
Therefore, we must establish the indications and limitations of the techniques currently available, taking into account the patient’s functional status, previous general health, tolerance to anaesthesia, and neurological function, among other considerations. Endovascular embolisation of the MMA is an effective alternative for patients with few neurological symptoms and poor previous health status (as the procedure may be performed under mild sedation), and in patients presenting CSDH recurrence.
FundingNo personal or institutional funding was received for this study or for the medication, equipment, or devices described.
Conflicts of interestThe authors have no conflicts of interest to declare.