Relapses are a hallmark of multiple sclerosis, being a characteristic feature of relapsing-remitting multiple sclerosis (RRMS). The occurrence of a relapse constitutes a source of significant discomfort that impacts all domains of daily life of patients with multiple sclerosis (PwMS). In this study we first explored the psychometric properties of the Spanish version of the Fear of Relapse Scale (FoR) in a sample of patients with RRMS. Besides, we explored the relationship between the Fear of Relapse Scale with fatigue and cognitive perceived deficits in our PwMS sample.
MethodsAn online cross-sectional survey was conducted on 173 MS patients from 12 Spanish-speaking countries (Argentina, Mexico, Uruguay, Dominican Republic, Spain, Cuba, Colombia, Guatemala, Chile, Paraguay, Peru, and El Salvador). Confirmatory factor analysis (CFA) was performed to assess the factor structure of the scale. Multiple linear regression was used to evaluate the effects of health self-perception, fatigue, and perceived cognitive deficits over fear of relapse.
ResultsThe three-factor model in the CFA yielded a good model fit (χ2/df = 2.25, P < .001, RMSEA = .078, CFI = .91). McDonalds’ Omega of the FoR (Spanish version) was .91. There was a statistically significant inverse correlation between FoR and health self-perception, and a positive correlation between FoR, fatigue, and perceived cognitive deficits. Finally, level of fatigue was a predictor of fear of relapse.
ConclusionsThe Spanish version of the Fear of Relapse Scale is a valid and reliable instrument to explore the experience of fear of relapse in patients with RRMS.
Las recaídas son un sello distintivo de la esclerosis múltiple, siendo un rasgo característico de la esclerosis múltiple remitente-recurrente (EMRR). La ocurrencia de una recaída constituye una fuente de malestar significativo que impacta todos los dominios de la vida diaria de los pacientes con esclerosis múltiple (PcEM). En este estudio primero exploramos las propiedades psicométricas de la versión en español de la Escala de Miedo a la Recaída (FoR) en una muestra de pacientes con EMRR. Además, exploramos la relación entre la Escala de Miedo a la Recaída con la fatiga y los déficits cognitivos percibidos en nuestra muestra de PcEM.
MétodosSe realizó una encuesta transversal en línea a 173 pacientes con EM de 12 países de habla hispana (Argentina, México, Uruguay, República Dominicana, España, Cuba, Colombia, Guatemala, Chile, Paraguay, Perú y El Salvador). Se realizó un análisis factorial confirmatorio (AFC) para evaluar la estructura factorial de la escala. Se utilizó regresión lineal múltiple para evaluar los efectos de la autopercepción de la salud, la fatiga y los déficits cognitivos percibidos sobre el miedo a la recaída.
ResultadosEl modelo de tres factores en el CFA arrojó un buen ajuste del modelo (χ2/df = 2.25, P < .001, RMSEA = .078, CFI = .91). El valor de Omega de la escala (versión en español) fue de .91. Hubo una correlación estadísticamente significativa e inversa entre la FoR y la autopercepción de salud, y una correlación positiva entre la FoR, la fatiga y los déficits cognitivos percibidos. Finalmente, el nivel de fatiga fue predictores del miedo a la recaída.
ConclusionesLa versión española de la Escala de Miedo a la Recaída es un instrumento válido y fiable para explorar la experiencia de miedo a la recaída en pacientes con EMRR.
Health-related fear reactions (also known as health anxiety [HA]) are common in patients with chronic disease (eg hypertension, diabetes and cancer).1–3 When fear related to the disease is mild or moderate, it can be a factor that favors adherence to treatment and responsible self-care. On the other hand, fear can also become exaggerated, affecting quality of life and daily functioning.4 A recently published systematic review found that clinically significant health-related fear reactions are closely related to post-traumatic stress disorder symptoms, depression, distress, generalized anxiety disorder, and lower cognitive functioning.4 It is important to highlight that fear related to health is closely related to the clinical characteristics of each chronic disease. For example, in cancer patients the most studied construct has been the fear of cancer recurrence5; in patients with heart disease, cardiac anxiety6; in diabetes, the “fear of hypoglycemia” and in Parkinson’s disease and multiple sclerosis (MS), the fear of falling.7,8 However, in the particular case of multiple sclerosis, a neurological disease characterized by areas of demyelination (lesions) within the central nervous system,9 the phenomenon of fear of relapse (FoR) has received practically no attention.10
Relapse (or exacerbation) are a hallmark of multiple sclerosis, being a characteristic feature of relapsing-remitting multiple sclerosis (RRMS), the most prevalent MS phenotype (85%).11,12 A relapse is characterized by a worsening of the symptoms of the disease (or the appearance of new symptoms) during an episode of acute disease activity which lasts for more than 24 hours, followed by a period of partial or complete recovery.12,13
The occurrence of a relapse constitutes a source of significant discomfort that impacts all domains of the daily life of patients with multiple sclerosis (PwMS). There is evidence that during a relapse, levels of anxiety, depression, and fatigue increase significantly, causing a deterioration in mental health and general well-being.14–16 In addition, the occurrence of relapses reduces the independence of patients and compromises their ability to perform housework, care for children, or perform successfully at work, causing an increase in reactions of anger, frustration and guilt.17
On the other hand, the unpredictable nature of relapses, the expectation of their severity, and their potential consequences can represent an important source of stress in PwMS, increasing fear of the next relapse.18 The experience of fear of relapse can also affect the perceived quality of life in PwMS,10 affecting their general well-being.
To explore FoR, Khatibi et al.10 developed the Fear of Relapse Scale for relapsing-remitting multiple sclerosis patients. The scale is made up of 26 items grouped into three factors (fear of disability following a relapse, fear of the psychological and physiological consequences of a relapse, and limitation resulting from fear). The scale was validated in a sample of 168 patients with RRMS, showing adequate psychometric properties, becoming a valuable instrument to explore the impact of uncertainty caused by the disease on quality of life in PwMS.
As far as we know, the scale is only available in Farsi and English. For example, to date there is no version of the scale in Spanish, which limits its use in the Ibero-American region. In this sense, the main objective of this study is to explore the psychometric properties of the Spanish version of the Fear of Relapse Scale (FoRs-SV) in a sample of patients with RRMS. Additionally, in this research we will explore the relationship between FoR and fatigue and perceived cognitive deficits.
This is the first study that explores the psychometric properties of the Fear of Relapse Scale in a Spanish-speaking population, which opens up new opportunities for its use in Ibero-American countries and especially in the Latin American and Caribbean region.
MethodsStudy design and participantsThis cross-sectional study was developed online. Google Forms® was used to disseminate the survey. Potential patients were invited to participate in the study through telephone calls and Instagram, WhatsApp, and Facebook groups. In the case of telephone calls, the telephone numbers were extracted from the medical records of the patients by their neurologist. In addition, administrators and influencers of Instagram, WhatsApp, and Facebook groups specifically dedicated to PwMS were contacted. Presidents of patient associations were also contacted; they received an explanation of the purpose of the research and subsequently shared the survey link among their members. As part of the study’s dissemination strategy, one of the researchers (RMJM) participated in dissemination actions in mass media and social networks (radio program and dissemination on Instagram), where he explained the objective of the research and patients with multiple sclerosis were invited to participate.
The research was developed between August 13 and October 13, 2021. A total of 229 PwMS voluntarily completed the questionnaire. Of the initial total sample, 12 patients were excluded for having a relapse of the disease during the last 1 month or at the time of survey completion. On the other hand, 43 patients were excluded for presenting a disease phenotype that did not correspond to relapsing-remitting multiple sclerosis (RRMS). Finally, one participant under 18 years of age was excluded from the final sample, which was made up of 173 patients with RRMS. The study included patients from 12 Spanish-speaking countries (Argentina, Mexico, Uruguay, Dominican Republic, Spain, Cuba, Colombia, Guatemala, Chile, Paraguay, Peru, and El Salvador).
MeasuresDemographic and Clinical Information: the demographic variables explored included age, gender, education, marital status, and country. To evaluate health self-perception, we use the ad hoc question “how do you consider your general health to be?” (from 1 [“very poor”] to 5 [“excellent”]). The clinical variables included MS phenotype and disease duration.
The Fear of Relapse Scale10: The Fear of Relapse Scale is a 26-item scale grouped into three factors. The first factor (“Fear of disability following a relapse”) is composed of 13 items (items 1, 2, 3, 6, 7, 8, 9, 10, 11, 17, 24, 25, and 26), the second factor (“Fear of the psychological and physiological consequences of a relapse”) is composed of 8 items (12, 13, 14, 15, 16, 18, 20, 21) and the third factor (“Limitation resulting from fear”) groups items 4, 5, 19, 22, and 23.10 The Cronbach alpha coefficient of the original version of the scale was 0.94.
Scale translation procedureBefore starting the translation process, the authors of this study requested authorization from the lead author of the Fear of Relapse Scale to carry out the translation and adaptation of the scale. After obtaining authorization the Fear of Relapse Scale was translated taking into account international standards for the adaptation of psychological tests.19 The forward-backward translation method was applied to adapt the scale into Spanish. In the first stage, two independent translators conducted the forward translation of the scale into Spanish. One of the translators was a specialist in international variations of the Spanish language, which favored the linguistic adaptation of the scale, taking into account the diversity of countries involved. In the back-translation stage, both versions were translated back into English by a professional translator with experience in psychological research and by one bilingual neuropsychology professor (blind to the original version of the Fear of Relapse Scale). Before having a final version, three experts suggested minor changes and approved the final version shown in Appendix 1, Supplementary data.
Modified Fatigue Impact Scale 5-item version (MFIS-5): The MFIS-5 is a brief, validated self-reported measure of fatigue in MS, including five of the 21 items from the original Modified Fatigue Impact Scale.20 The MFIS-5 is made up of 2 items from the physical subscale (items 10 and 17), 2 items from the cognitive subscale (items 1 and 19), and one item from the psychosocial subscale (item 9). The MFIS-5 scores each item on a 5-point Likert scale from 0 (never) to 4 (almost always). Total scores range from 0 to 20, with a higher score indicating more severe fatigue.20 The 5-item version of the scale has shown excellent psychometric properties.21,22 The validated Spanish version of the instrument was used.23
Perceived deficits questionnaire 5-item version (PDQ-5): The PDQ-5 is a brief, self-reported measure of perceived cognitive dysfunction in MS, including 5 of the 20 items from the original Perceived Deficits Questionnaire (PDQ).20 The PDQ-5 scores each item on a 5-point Likert scale from 0 (never) to 4 (almost always). The PDQ-5 is made up of 2 items from the planning/organization subscale (items 4 and 19), one item from the attention/concentration subscale (item 9), one item from the prospective memory subscale (item 11), and one item from the retrospective memory subscale (item 14). The PDQ-5 scores each item on a 5-point Likert scale from 0 (never) to 4 (almost always). Total scores range from 0 to 20. Higher scores indicate greater perceived cognitive impairment.20
ProcedureThe study protocol was approved by the ethics committee of the Department of Psychology of the Universidad Central “Marta Abreu” de Las Villas. All procedures performed in this study were in accordance with the ethical standards of the 1964 Helsinki Declaration. Informed consent was obtained from all participants included in the study.
Data analysisThe data were processed using SPSS/Windows (version 21) and AMOS (version 22). Descriptive statistics was used to explore patients’ characteristics and confirmatory factor analysis (CFA) was performed to assess the factor structure of the Fear of Relapse Scale (Spanish version). In this study, CFA was used to test the 3-factor structure proposed by the author of the original scale.10 To estimate the presence of multivariate normality in the data, the Mardia coefficient was calculated. Maximum likelihood estimate was used for the hypothetical model’s goodness-of-fit and hypothesis validation. Model fits were assessed through the χ2/df value (value < 3), comparative fit index (CFI) (≥ 0.90), and root mean square error of approximation (RMSEA) (value ≤ 0.10).24,25 The Pearson correlation coefficient was performed to assess the convergent validity of the Fear of Relapse Scale (Spanish version). We also investigated the reliability of the scale with McDonalds’ omega coefficient. Multiple linear regression was used to evaluate the effects of health self-perception, fatigue, and perceived cognitive deficits over FoR.
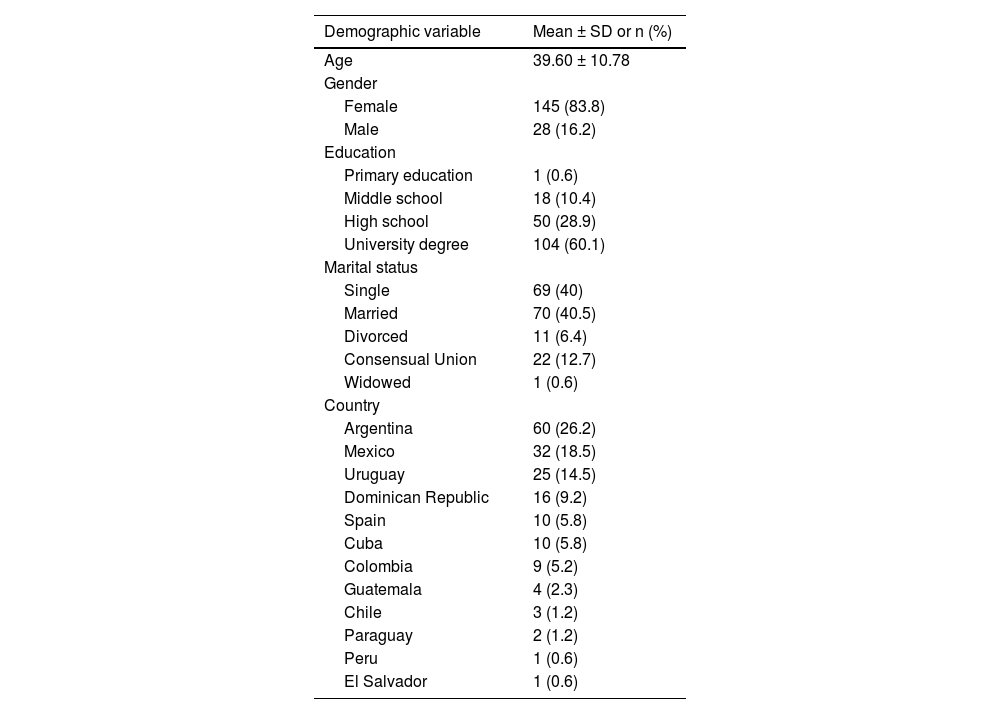
ResultsCharacteristics of the sampleDemographic information for 173 PwMS is summarized in Table 1. The mean age of participants (n = 173) was 39.60 years with a range between 18 and 65 years old, and female gender predominated in the sample (83.8%). In our sample, most of the participants had a university-level degree (60.1%). Additionally, the 40.5% of patients were married. In the sample, patients from Argentina (26.2%), Mexico (18.5%), and Uruguay (14.5%) predominated. The least represented countries were Peru (0.6%), El Salvador (0.6%), and Paraguay (1.2%). Clinical information for patients and the global results of the scales used are summarized in Table 2.
Participant demographic data (n = 173).
| Demographic variable | Mean ± SD or n (%) |
|---|---|
| Age | 39.60 ± 10.78 |
| Gender | |
| Female | 145 (83.8) |
| Male | 28 (16.2) |
| Education | |
| Primary education | 1 (0.6) |
| Middle school | 18 (10.4) |
| High school | 50 (28.9) |
| University degree | 104 (60.1) |
| Marital status | |
| Single | 69 (40) |
| Married | 70 (40.5) |
| Divorced | 11 (6.4) |
| Consensual Union | 22 (12.7) |
| Widowed | 1 (0.6) |
| Country | |
| Argentina | 60 (26.2) |
| Mexico | 32 (18.5) |
| Uruguay | 25 (14.5) |
| Dominican Republic | 16 (9.2) |
| Spain | 10 (5.8) |
| Cuba | 10 (5.8) |
| Colombia | 9 (5.2) |
| Guatemala | 4 (2.3) |
| Chile | 3 (1.2) |
| Paraguay | 2 (1.2) |
| Peru | 1 (0.6) |
| El Salvador | 1 (0.6) |
SD: Standard Deviation.
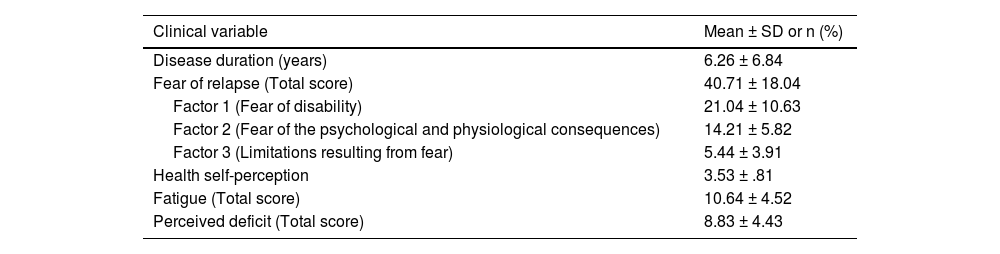
Participant clinical and psychological data (n = 173).
| Clinical variable | Mean ± SD or n (%) |
|---|---|
| Disease duration (years) | 6.26 ± 6.84 |
| Fear of relapse (Total score) | 40.71 ± 18.04 |
| Factor 1 (Fear of disability) | 21.04 ± 10.63 |
| Factor 2 (Fear of the psychological and physiological consequences) | 14.21 ± 5.82 |
| Factor 3 (Limitations resulting from fear) | 5.44 ± 3.91 |
| Health self-perception | 3.53 ± .81 |
| Fatigue (Total score) | 10.64 ± 4.52 |
| Perceived deficit (Total score) | 8.83 ± 4.43 |
SD: Standard Deviation.
We conducted a CFA using the Amos 22 software. The 3-factor model in the CFA yielded a good model fit (χ2/df = 2.25, P < .001; RMSEA = 0.078; CFI = 0.91) (Fig. 1). McDonalds’ 0mega of the Fear of Relapse Scale (Spanish version) was 0.91. The first factor (fear of disability following a relapse) showed an internal consistency of 0.87, the second factor (fear of the psychological and physiological consequences of a relapse) showed an internal consistency of 0.78, and the third factor (limitation resulting from fear) showed a McDonalds’ omega of 0.68.
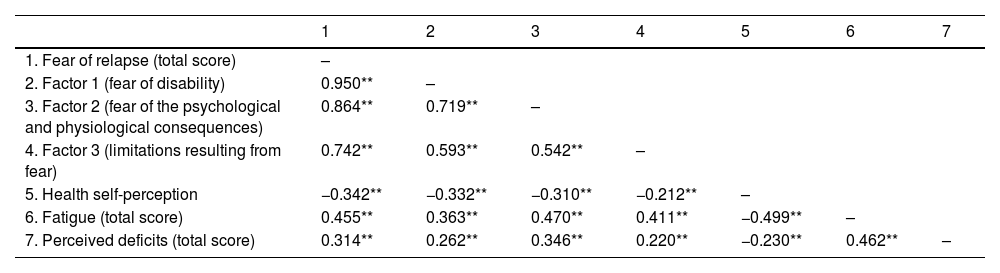
A concurrent validity analysis was also conducted. There was a statistically significant and inverse correlation between the Fear of Relapse Scale and health self-perception (high scores on the FoRs-SV scale correlate with low scores on the self-perceived health question). The 3 factors of the scale, independently, also showed a significant inverse association with health self-perception. We also found a positive correlation between the Fear of Relapse Scale (and its 3 factors) and fatigue, with high levels of FoR associated with high levels of fatigue (high scores on the FoRs-SV correlate with high scores on the MFIS-5 scale). We also found a strong (positive) correlation between the Fear of Relapse Scale and perceived deficits (high scores on the FoRs-SV scale correlate with high scores on the scales PDQ-5) (Table 3).
Correlation between fear of relapse (total score and subscales) with health self-perception, fatigue (total score), and perceived deficit (total score) (n = 173).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Fear of relapse (total score) | – | ||||||
| 2. Factor 1 (fear of disability) | 0.950** | – | |||||
| 3. Factor 2 (fear of the psychological and physiological consequences) | 0.864** | 0.719** | – | ||||
| 4. Factor 3 (limitations resulting from fear) | 0.742** | 0.593** | 0.542** | – | |||
| 5. Health self-perception | −0.342** | −0.332** | −0.310** | −0.212** | – | ||
| 6. Fatigue (total score) | 0.455** | 0.363** | 0.470** | 0.411** | −0.499** | – | |
| 7. Perceived deficits (total score) | 0.314** | 0.262** | 0.346** | 0.220** | −0.230** | 0.462** | – |
A multiple regression analysis was run to explore the effects of health self-perception, fatigue and perceived deficits on FoR. (Table 4). The overall regression model was significant (F[3.172] = 17.61, P < .001), accounting for 22.5% of the variance in FoR scores. Only fatigue showed a significant association with higher levels of FoR, explaining 31.8% of the variance in FoR scores.
Association between fear of relapse (total score), health self-perception, fatigue (total score), and perceived deficit (total score).
| B | SE | β | t | P | |
|---|---|---|---|---|---|
| (Constant) | 34.392 | 8.368 | 4.110 | .000 | |
| Health self-perception | −3.337 | 1.709 | −0.153 | 1.975 | .050 |
| Fatigue (total score) | 1.268 | 0.339 | 0.318 | 3.737 | .000 |
| Perceived deficits (total score) | 0.537 | 0.308 | 0.132 | 1.744 | .083 |
Dependent variable: Fear of Relapse (total score); SE: standard error.
The objective of this study was to explore the psychometric properties of the Spanish version of the Fear of Relapse Scale in a sample of Spanish-speaking patients with RRMS. In addition, the relationship between the Fear of Relapse Scale and fatigue and cognitive perceived deficits was explored.
Our results confirm a 3-factor structure of the Spanish version of the Fear of Relapse Scale (FoRs-SV), coinciding with the factor structure proposed by the authors of the original version.10 In addition, the FoRs-SV showed very good internal consistency (ω = 0.91), considering that the Cronbach’s alpha reported in the original study was 94.
Our results also showed a significant positive association between the FoRs-SV, fatigue, and cognitive perceived deficit, as well as a negative association with self-perceived health (worse self-perceived health is related with higher levels of fear of relapse). Additionally, the 3 factors of the scale independently (fear of disability following a relapse, fear of the psychological and physiological consequences of a relapse, and limitation resulting from fear) also showed strong correlations with the variables fatigue, cognitive perceived deficit, and self -perceived health. Finally, level of fatigue was a predictor of level ofFoR.
Recent studies that have used the Fear of Relapse Scale in patients with RRMS have also verified an association between level of FoR and poorer quality of life in these patients. The original study where the scale was presented found that in the participants (168 RRMS patients), the increase in fear levels was related to an increase in the levels of anxiety, depression, and stress. The authors also verified a positive association between intolerance to uncertainty reported by patients (fear of the unknown) and levels of FoR.10
Other recent research explored FoR in a sample of 165 patients during the COVID-19 pandemic (85% were RRMS patients). In this study, the authors explored, in addition to FoR, psychological well-being and social support. According to the results, there was a significant negative correlation between social support and FoR, and also significant positive correlations between FoR and anxiety, depression, and stress.26
Our results are also supported by a study conducted by Khatibi et al.18 that explored FoR and its association with quality of life, in a sample of 70 RRMS patients. Additionally, other variables were considered, including HA, number of relapses, duration of disease, type of medication,and perceived level of side effects. All these variables were included in a regression model, verifying that quality of life was most strongly associated with disease severity, number of relapses, and disease duration. However, after incorporating FoR into the model (in the presence of the other covariates), this association between disease severity and quality of life was attenuated, and FoR remained the only covariate significantly associated with quality of life.18
The authors also want to draw attention to the poor factor loading shown by item 12 (“A severe relapse with intense symptoms can lead to death”) to the second factor (“fear of the psychological and physiological consequences of a relapse”). In this sense, there are possible explanations that help us understand this result. The most parsimonious explanation would be related to the clinical form presented by the participants included in the study (RRMS) and the knowledge that patients have about their disease. There is evidence that, in terms of disease course and mortality, a higher mortality rate among patients with progressive forms of the disease has been shown with respect to patients with RRMS.27,28 In this way, the patients who participated in our study selected very low scores on this item, considering it unlikely. This would be an aspect that could be explored further in future studies.
We agree with Khatibi et al.10 when they state that FoR in MS is a neglected phenomenon in the studies investigating the psychological aspects of the diagnosis and living with MS. However, if we consider the preliminary evidence available to date, we will understand the importance that this category (FoR) is beginning to gain when it comes to understanding the self-perceived quality of life in PwMS from a multidimensional perspective.
This study has some limitations that we have to address. First, in our investigation the divergent validity of the Fear of Relapse Scale was not analyzed. In future studies, this type of analysis should be included. On the other hand, our results did not explore the link between the years of progression of the disease, the degree of disability of the patients, and the experience of FoR. Both aspects (onset of the disease and level of disability) are important variables to consider in future studies. Another aspect that we consider a limitation of our research is that the number of relapses that the patients had experienced during the progression of the disease was not taken into account. It is reasonable to anticipate that patients who have experienced more relapses of the disease will also have a FoR and consequently experience poorer quality of life. Finally, it is important to point out that in our study, the cut-off point for the CFI was larger than 0.90. However, some authors suggest taking a value larger than 0.95 as a reference, which must be taken into consideration when interpreting our results.29
Despite these limitations, we consider that the translation into Spanish of the Fear of Relapse Scale and its validation in patients with RRMS constitutes an important step in exploring the impact of FoR on the psychological well-being and quality of life of patients with MS in the Ibero-American context.
Ethical standardsAll procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained for all patients for being included in the study.
Declaration of competing interestThe authors have no conflicts of interest.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
First of all, we want to express our infinite gratitude to all the people with MS who participated in the study. We especially thank the coordinators and patients of the EMA (Esclerosis Múltiple Argentina) and ALCEM (Asociación de Lucha Contra la Esclerosis Múltiple) associations, as well as the patient associations of Mexico, Uruguay, Cuba, and the Dominican Republic. We also thank Rocio Seijas (Escleroamigos) and Fernando Champomier (Emstrongs), who, from their projects, supported our research from the beginning. Finally, we especially thank Nicolás Edgardo Costa, coordinator of the program “The game does not end” (ALCEM podcast series made by people living with MS).