Headache is a frequent reason for consultation with primary care (PC) physicians. However, the condition is underdiagnosed and undertreated. One reason for this may be the lack of specific training on headache in PC.
MethodsWe conducted a descriptive cross-sectional study of data gathered with a self-administered survey that was completed by PC physicians from our health district. We collected sociodemographic data and information on previous training in neurology and headache, and training needs.
ResultsThe survey was completed by 104 PC physicians, 53% of whom were women; mean age was 49 years. Most respondents worked in urban settings (42.3%) and had been trained via residency (77.9%). Although 65.4% spent more time with patients with headache than with other patients, only 32.7% used the International Classification of Headache Disorders. In our sample, 68.3% of respondents reported a high or very high interest in headache, and 75.9% wished to receive further training on the condition; theoretical and practical courses and update lectures were regarded as the most useful tools. In clinical practice, 90% used triptans and 78% used preventive treatments. The most frequently used drug was amitriptyline; only 22.1% choose topiramate.
ConclusionsPC physicians are in frequent contact with patients with headache and show interest in receiving training on this condition. This could be helpful in designing training programmes aimed at improving quality of care in this area.
La cefalea es un motivo de consulta frecuente en atención primaria (AP), sin embargo, se trata de una patología infradiagnosticada e infratratada. Uno de los posibles factores es la falta de formación de los profesionales de AP en cefaleas.
MétodosEstudio descriptivo transversal mediante encuesta auto-administrada a los médicos de AP de nuestro sector sanitario. Se recogieron variables sociodemográficas, variables relacionadas con la formación previa en neurología y cefaleas y variables en relación con sus necesidades formativas.
ResultadosCompletaron la encuesta 104 médicos de atención primaria, de los cuales el 53% fueron mujeres y la edad media fue 49 años. La mayoría de los encuestados trabajan en un centro de salud urbano (42,3%) y se han formado vía MIR (77,9%). El 65,4% dedican más tiempo a una consulta de cefaleas que a otras consultas y sólo un 32,7% utilizan la Clasificación Internacional de Cefaleas. El 68,3% declaran tener un interés alto o muy alto en cefaleas y al 75,9% les gustaría mejorar su formación, eligiendo cursos teórico-prácticos y ponencias de actualización como la herramienta más útil. Un 90% utiliza triptanes en su práctica clínica diaria y el 78% emplea tratamientos preventivos. El fármaco más utilizado es amitriptilina y sólo un 22,1% elige topiramato.
ConclusionesLos profesionales de AP están en contacto constante con pacientes con cefaleas y muestran interés en la formación en esta patología, lo que podría ayudarnos a diseñar programas docentes dirigidos a mejorar la calidad asistencial en este ámbito.
Headache is one of the main reasons for patient referral to neurology departments by primary care physicians1 and the fifth most common reason for referral by emergency departments, accounting for over 10 million medical appointments per year.2 According to data from the 2006 National Health Survey of Spain, the estimated prevalence of migraine is 11.02%. In Spain, migraine affects approximately 12% of the general population, with 2.4% of the population presenting chronic migraine.3 The PALM study, conducted in 2006, aimed to characterise all aspects of migraine, to raise awareness of the impact of the condition, and to train the professionals involved in order to improve treatment and patient quality of life.4,5
Primary care frequently constitutes the initial point of contact for patients with headache; only a minority are referred to and treated in headache units.6 However, the care received at this level may be suboptimal and has been associated with a high rate of misdiagnosis, inadequate treatment of acute episodes, and delayed initiation of preventive treatment.7 According to the American Migraine Prevalence and Prevention Study,8 38% of patients with migraine are eligible for preventive treatment, but only 11% actually receive it.
However, few studies have attempted to improve integrated care for migraine in our setting. Furthermore, few data are available on primary care physicians’ knowledge of migraine and their training needs.
This study aimed to analyse primary care physicians’ understanding of neurological diseases in general and headache in particular, using objective (use of symptomatic and preventive treatments for migraine) and subjective parameters (confidence in their ability to perform a neurological examination and assess patients with headache). As a secondary objective, we aimed to determine the training needs of primary care physicians and which training methods they consider most attractive.
Material and methodsOur hospital’s headache unit designed a self-administered cross-sectional survey including semi-open questions; closed, multiple-choice questions; and open-ended questions. The survey was distributed at our hospital’s emergency department and at several referring primary care centres from our health district. We categorised healthcare professionals according to whether they worked in an urban or a rural setting, or at the emergency department of a tertiary hospital with a 24-h on-call neurologist. The study was conducted between December 2016 and December 2017. Participants remained anonymous at all times. We gathered the following information:
- a)
Sociodemographic variables and variables related to the professional activity of primary care physicians: sex, age, workplace (hospital emergency departments, pre-hospital emergency services, urban primary care centre, rural primary care centre), workload, and personal history of migraine.
- b)
Variables related to physicians’ knowledge of general neurology: perceived level of knowledge and expertise with neurological examination.
- c)
Variables related to physicians’ knowledge of headache: time dedicated to a patient with headache as compared to other types of consultations; knowledge and application of the third edition of the International Classification of Headache Disorders (ICHD-3),9 percentage of patients treated with triptans/preventive drugs, and the most frequently prescribed active ingredient.
- d)
Variables related to physicians’ training needs: type of activity deemed most appropriate to increase their knowledge of general neurology and of headache.
Qualitative variables are expressed as percentages and quantitative variables as means (standard deviation). Comparisons were made using the chi-square test. Statistical analysis was performed using the SPSS statistical software, version 23.0.
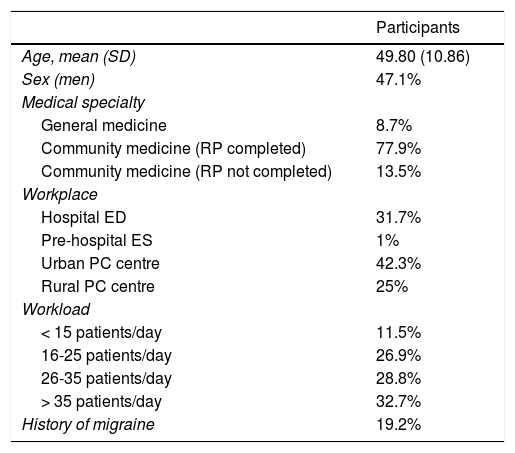
ResultsWe distributed a total of 110 surveys, 104 of which were completed (response rate of 94.5%). The first part of the survey gathered data on participants’ sociodemographic characteristics. Survey respondents’ mean age was 49.8 years (10.86); 47.1% were men. We also gathered information on the type of medical training received and whether professionals had completed Spain’s residency programme for specialisation (77.9%). Regarding workload, 32.7% of primary care physicians attended a mean of over 35 patients per day. The survey also enquired about the physician’s personal history of migraine (19.2%), as this factor may have an impact on their interest in the condition. No statistically significant association was observed between personal history of migraine and prescription of triptans (P = .948) or preventive treatment (P = .344), or workplace (P = .752). Table 1 summarises the results of the first part of the survey.
Sociodemographic variables of our sample of primary care physicians.
| Participants | |
|---|---|
| Age, mean (SD) | 49.80 (10.86) |
| Sex (men) | 47.1% |
| Medical specialty | |
| General medicine | 8.7% |
| Community medicine (RP completed) | 77.9% |
| Community medicine (RP not completed) | 13.5% |
| Workplace | |
| Hospital ED | 31.7% |
| Pre-hospital ES | 1% |
| Urban PC centre | 42.3% |
| Rural PC centre | 25% |
| Workload | |
| < 15 patients/day | 11.5% |
| 16-25 patients/day | 26.9% |
| 26-35 patients/day | 28.8% |
| > 35 patients/day | 32.7% |
| History of migraine | 19.2% |
ED: emergency department; ES: emergency services; PC: primary care; RP: residency programme; SD: standard deviation.
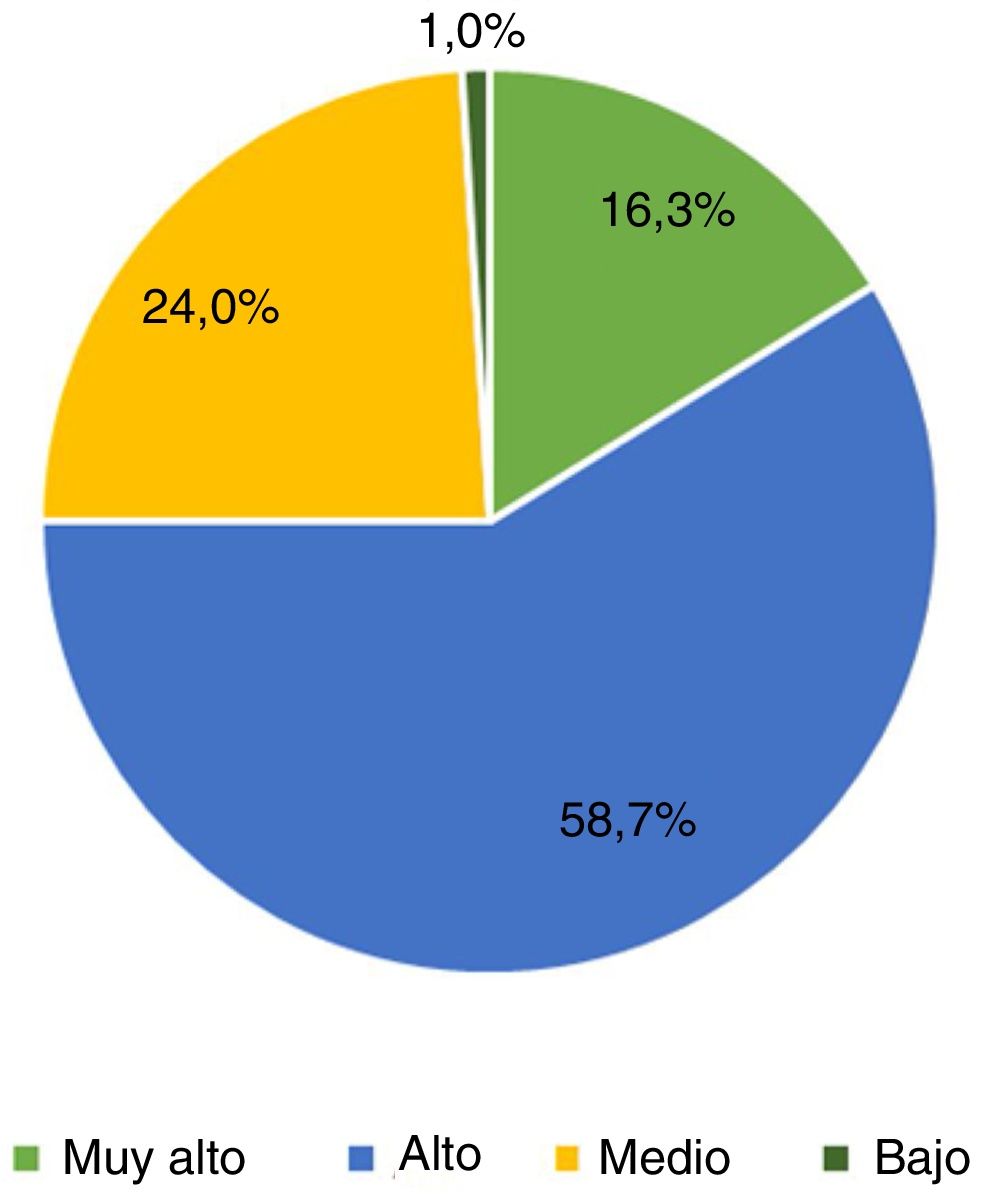
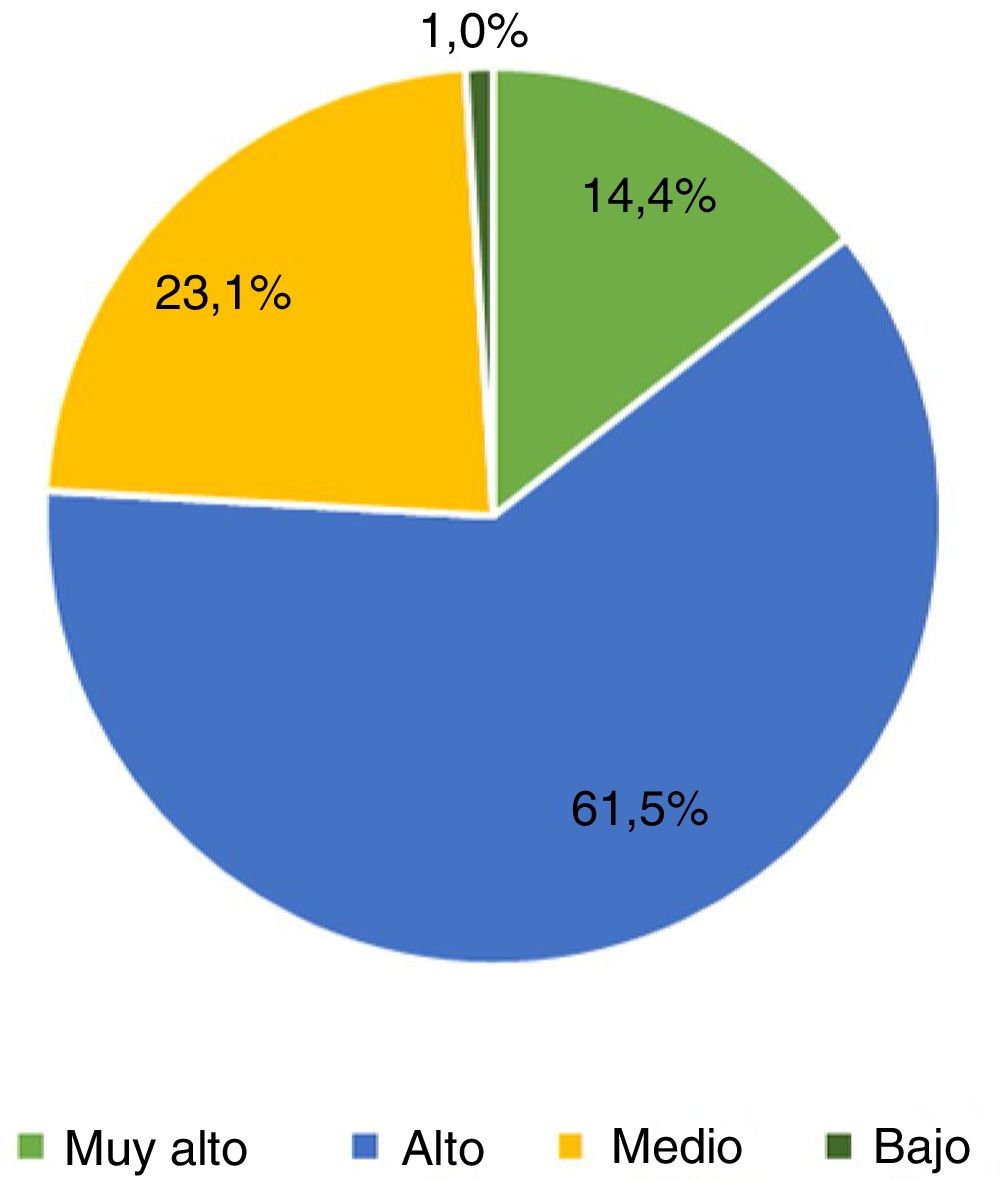
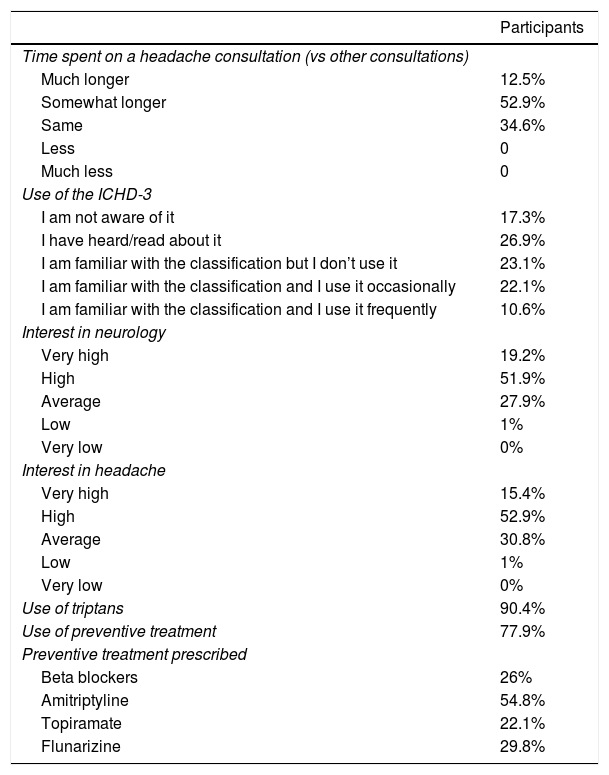
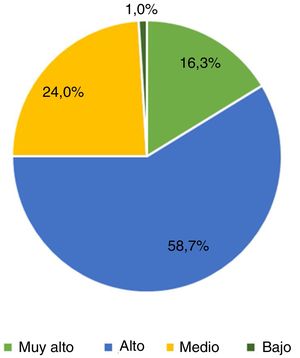
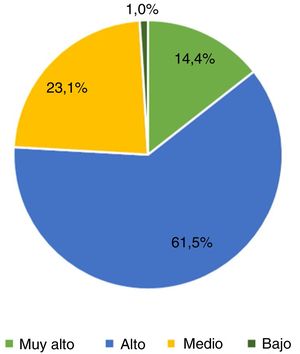
The second part of the survey focuses on primary care physicians’ knowledge of general neurology and of headache. Interestingly, 16.3% of respondents did not feel confident in performing a neurological examination, and 9.6% were unsure about how to complete it. Respondents were highly interested (52.9%) or very highly interested (15.4%) in headache. Primary care physicians were highly interested (61.5%) or very highly interested (14.4%) in receiving specific training about headache (Fig. 1 and 2). The ICHD-3 was used by 32.7% of primary care physicians (22.1%, occasionally; 10.6%, frequently)9; however, a high percentage of respondents did not use it or were not aware of it. Most primary care physicians spent longer with patients with headache than with those consulting for other reasons (12.5% reported “much longer” consultations and 52.9% “somewhat longer”).
Some 90.4% of survey respondents frequently prescribed (ie, prescribed to over 75% of patients) triptans for preventive treatment of migraine and 77.9% prescribed preventive treatment, with the most frequently prescribed active ingredients being amitriptyline (54.8%), flunarizine (29.8%), and beta blockers (26%). Topiramate was prescribed by 22.1% of survey respondents. These results are summarised in Table 2.
Variables related to primary care physicians’ training on neurology and headache.
| Participants | |
|---|---|
| Time spent on a headache consultation (vs other consultations) | |
| Much longer | 12.5% |
| Somewhat longer | 52.9% |
| Same | 34.6% |
| Less | 0 |
| Much less | 0 |
| Use of the ICHD-3 | |
| I am not aware of it | 17.3% |
| I have heard/read about it | 26.9% |
| I am familiar with the classification but I don’t use it | 23.1% |
| I am familiar with the classification and I use it occasionally | 22.1% |
| I am familiar with the classification and I use it frequently | 10.6% |
| Interest in neurology | |
| Very high | 19.2% |
| High | 51.9% |
| Average | 27.9% |
| Low | 1% |
| Very low | 0% |
| Interest in headache | |
| Very high | 15.4% |
| High | 52.9% |
| Average | 30.8% |
| Low | 1% |
| Very low | 0% |
| Use of triptans | 90.4% |
| Use of preventive treatment | 77.9% |
| Preventive treatment prescribed | |
| Beta blockers | 26% |
| Amitriptyline | 54.8% |
| Topiramate | 22.1% |
| Flunarizine | 29.8% |
ICHD: International Classification of Headache Disorders.
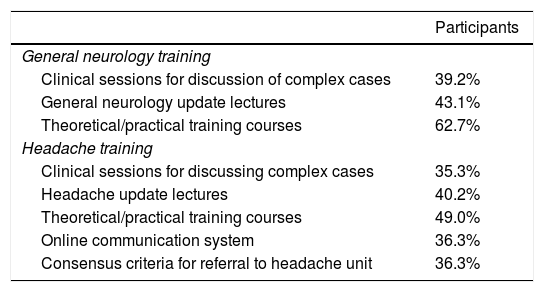
The purpose of our survey was to understand the training needs of primary care physicians and to determine the tools they consider most appropriate to increase their knowledge of headache. Participants were mainly interested in theoretical/practical training courses about neurology (62.7%) and headache (49.0%). This survey question was open-ended. Other suggestions were courses and workshops on neurological examination (n = 3), feedback sessions between neurologists and primary care physicians (n = 1), telephone consultations with the neurology department (n = 2), and documents and guidelines specifically designed for primary care physicians (n = 1). The results of this part of the survey are summarised in Table 3.
Variables related to primary care physicians’ training needs.
| Participants | |
|---|---|
| General neurology training | |
| Clinical sessions for discussion of complex cases | 39.2% |
| General neurology update lectures | 43.1% |
| Theoretical/practical training courses | 62.7% |
| Headache training | |
| Clinical sessions for discussing complex cases | 35.3% |
| Headache update lectures | 40.2% |
| Theoretical/practical training courses | 49.0% |
| Online communication system | 36.3% |
| Consensus criteria for referral to headache unit | 36.3% |
Patients with headache represent 15% of all patients referred to general neurologists by primary care physicians.10 According to Huerta et al.,11 patients with headache represent nearly 25% of all primary care referrals. More specifically, migraine is the most frequent diagnosis at headache units12 and the main reason for referral from primary care.13 However, the condition is underdiagnosed and undertreated.
One of the main reasons for this suboptimal treatment of migraine is the lack of specific training for primary care physicians. In our study, primary care physicians showed considerable interest in headache (“very highly interested” in 15.4% and “highly interested” in 52.9%), although only 32.7% used the ICHD-3.9 Most survey respondents (90.4%) prescribed triptans as a symptomatic treatment to over 75% of patients with migraine, and 77.9% frequently prescribed preventive treatment. The most frequently prescribed drug for migraine was amitriptyline (54.8%), followed by flunarizine (29.8%); only 26% of survey respondents prescribed beta blockers. Topiramate was the least frequently prescribed drug (22.1%). Our results suggest that primary care physicians are familiar with the treatments recommended in the Spanish Society of Neurology’s clinical practice guidelines for migraine. However, 22% do not start preventive treatment in these patients, and the preventive drugs most frequently prescribed are not the recommended first-line treatments for migraine.14 We found no statistically significant association between the physician’s personal history of migraine and prescription of triptans or preventive treatment. A previous study reported differences between neurologists with and without history of migraine in their patients’ mean number of migraine attacks in the previous 3 months and the rate of triptan prescription.15
Interestingly, survey respondents were highly or very highly interested in receiving training on neurology and headache. Our results and the previously reported moderate diagnostic agreement between primary care physicians and neurologists10 underscore the need for specific migraine training programmes for primary care physicians with a view to improving diagnosis and treatment of these patients. For most participants, the most attractive training tools were theoretical/practical training courses on neurology and headache, and update lectures. In our sample, such initiatives as an online consultation service (eg, via e-mail)16 were suggested by only 36% of participants.
Similar initiatives have been implemented in other countries. Minen et al.,17 for example, evaluated primary care physicians’ level of knowledge of headache and training needs through 3 sessions with primary care physicians; these data were used to design specific training programmes. Braschinsky et al.18 designed a training programme in Estonia aimed at improving headache management in primary care. They evaluated rates of referral to the neurology department, diagnoses made, and treatments started before and after the programme, recording favourable results.
One proposal made in Spain is the implementation of an e-mail consultation service to improve communication between primary care physicians and headache units. Pedraza et al.16 put this “shared management” experience into practice, with primary care physicians and neurologists using an e-mail service to determine patients’ need for referral to the headache unit, to monitor their progression, and for training purposes; as a novelty, primary care physicians were also able to use the e-mail service to consult about their own symptoms. Most training-related e-mails enquired about the potential adverse effects of preventive drugs. This initiative enabled integrated care of patients with headache and helped determine which patients required referral to the headache unit and which could be managed by primary care physicians without referral.
Our data show that up to 22.1% of primary care physicians do not prescribe preventive treatment for migraine. Furthermore, beta blockers and topiramate, 2 treatment options widely used in headache units, are rarely prescribed by primary care physicians. None of the participants used other preventive drugs mentioned in the latest edition of the Spanish Society of Neurology’s clinical practice guidelines for migraine (lisinopril, candesartan, zonisamide).
Our secondary objective was to analyse the training needs of primary care physicians; 26% of participants were unsure about how to perform and interpret a neurological examination. Primary care physicians were “highly interested” or “very highly interested” in training on neurology and headache (75% and 76%, respectively). The most popular training tools were theoretical/practical training courses and update lectures; workshops on neurological examination were also frequently mentioned. Few studies have addressed the involvement of primary care physicians in headache management and analysed their concerns. Our results will help design training programmes for primary care physicians and improve headache management at this level of care.
Our study is not without limitations. Firstly, the survey was distributed among primary care physicians from a specific region; therefore, our results cannot be extrapolated to the whole population. Second, some questions were open-ended, which may have introduced recall and retrospective biases. Our results may also be affected by a non-response bias. Finally, the sample size was small due to the high workload of primary care physicians.
In conclusion, primary care physicians show great interest in headache. Our results provide insight into the current situation of headache management in primary care in our setting and may help in designing training programmes to improve the management of patients with headache at this level. Finally, we should acknowledge the commitment of primary care physicians and thank them for participating in this study.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank all the primary care physicians who participated in our study.
Please cite this article as: López-Bravo A, Bellosta-Diago E, Viloria-Alebesque A, Marín-Gracia M, Laguna-Sarriá J, Santos-Lasaosa S. Cefalea como motivo de consulta: la visión desde atención primaria. Neurología. 2021;36:597–602.