When a patient is diagnosed with primary headache or craniofacial neuralgia in the emergency department or in primary care, and is referred to a neurologist due to the complexity of the case, it is useful to know whether additional examination should be sought and the priority (urgent, preferential, or normal) with which the patient should be seen. This will avoid unnecessary delays in patients with disabling headache and where organic causes are suspected.
In order to issue recommendations on this matter, the Spanish Society of Neurology's Headache Study Group has decided to create a series of agreed recommendations constituting a referral protocol for patients with headache and/or craniofacial neuralgia.
DevelopmentYoung neurologists with an interest and experience in headache were invited to draft a series of practical guidelines in collaboration with the Spanish Society of Neurology's Headache Study Group Executive Committee. For practical reasons, the document was divided into 2 articles: this first article focuses on primary headaches and craniofacial neuralgias and the second on secondary headaches. In order for the recommendations to be helpful for daily practice they follow a practical approach, with tables summarising referral criteria, examinations to be performed, and referral to other specialists.
ConclusionsWe hope to offer a guide and tools to improve decision-making regarding patients with headache, identifying complementary tests to prioritise and referral pathways to be followed, in order to avoid duplicated consultations and delayed diagnosis and treatment.
Cuando tras una correcta anamnesis y exploración neurológica se diagnostica a un paciente con una cefalea primaria o una neuralgia craneofacial en urgencias o atención primaria y se decide derivar a neurología por complejidad es útil conocer si además se deberían solicitar exploraciones complementarias y la preferencia (urgente, preferente o normal) con la que se debería derivar para que el paciente llegue a la consulta del neurólogo sin demoras innecesarias en pacientes con dolores incapacitantes o con sospecha de organicidad.
Por este motivo, el Grupo de Estudio de Cefalea de la Sociedad Española de Neurología, ha decidido crear unas recomendaciones consensuadas que establezcan un protocolo de derivación de pacientes con cefalea y/o neuralgias craneofaciales.
DesarrolloSe ha contactado con neurólogos jóvenes con interés y experiencia en cefalea y con la Junta Directiva del Grupo de Estudio de Cefalea de la Sociedad Española de Neurología que han desarrollado este documento que, por razones prácticas, se ha dividido en 2 artículos. Esta primera centrada en las cefaleas o neuralgias craneofaciales primarias y una segunda que se focaliza en las cefaleas secundarias. El enfoque es práctico con tablas que resumen los criterios de derivación con exploraciones complementarias y otros especialistas a los que derivar, para que sea útil y facilite su uso en nuestra práctica asistencial diaria.
ConclusionesEsperamos ofrecer una guía y herramientas para mejorar la toma de decisiones ante un paciente con cefalea, valorando exploraciones a priorizar y qué circuitos seguir para así evitar la duplicación de consultas y retrasos en el diagnóstico y en el tratamiento.
The Spanish Society of Neurology's Headache Study Group (GECSEN) has detected that patients are attending consultation for headache without having undergone the necessary complementary tests or followed the appropriate care circuits, and are sometimes referred at an inopportune time or without the necessary level of urgency/priority.
We have therefore drafted a series of consensus recommendations based on published scientific evidence and our own experience, establishing protocols for the referral of patients with primary headache and/or craniofacial neuralgias from emergency or primary care (PC) departments. These recommendations are general and will require adaptation to the specific circumstances of each centre.
These are practical guidelines addressing differential diagnosis, studies to be requested, and how/when to refer. For a more detailed study of the different types of headache, we recommend consulting GECSEN's Official Clinical Practice Guidelines for Headache,1 which is available online at the study group's webpage (gecsen.sen.es).
These guidelines were drafted with the collaboration of young neurologists with experience in treating headaches. For practical reasons, the recommendations are divided into 2 publications: the present work, focusing on primary headache and craniofacial neuralgias, and another which addresses secondary headache and neuralgias.
The primary headaches addressed are: migraine, tension-type headaches, trigeminal autonomic cephalalgias, cough headaches, exercise headaches, headaches associated with sexual activity, stabbing headaches, nummular headaches, hypnic headaches, new daily persistent headaches, and craniofacial neuralgias. We present each type of headache, with a brief description of the diagnostic criteria according to the International Headache Society's International Classification of Headache Disorders (ICHD-3 beta),2 the most important differential diagnoses to be considered, and tables illustrating the protocols for action and referral from emergency departments and PC.
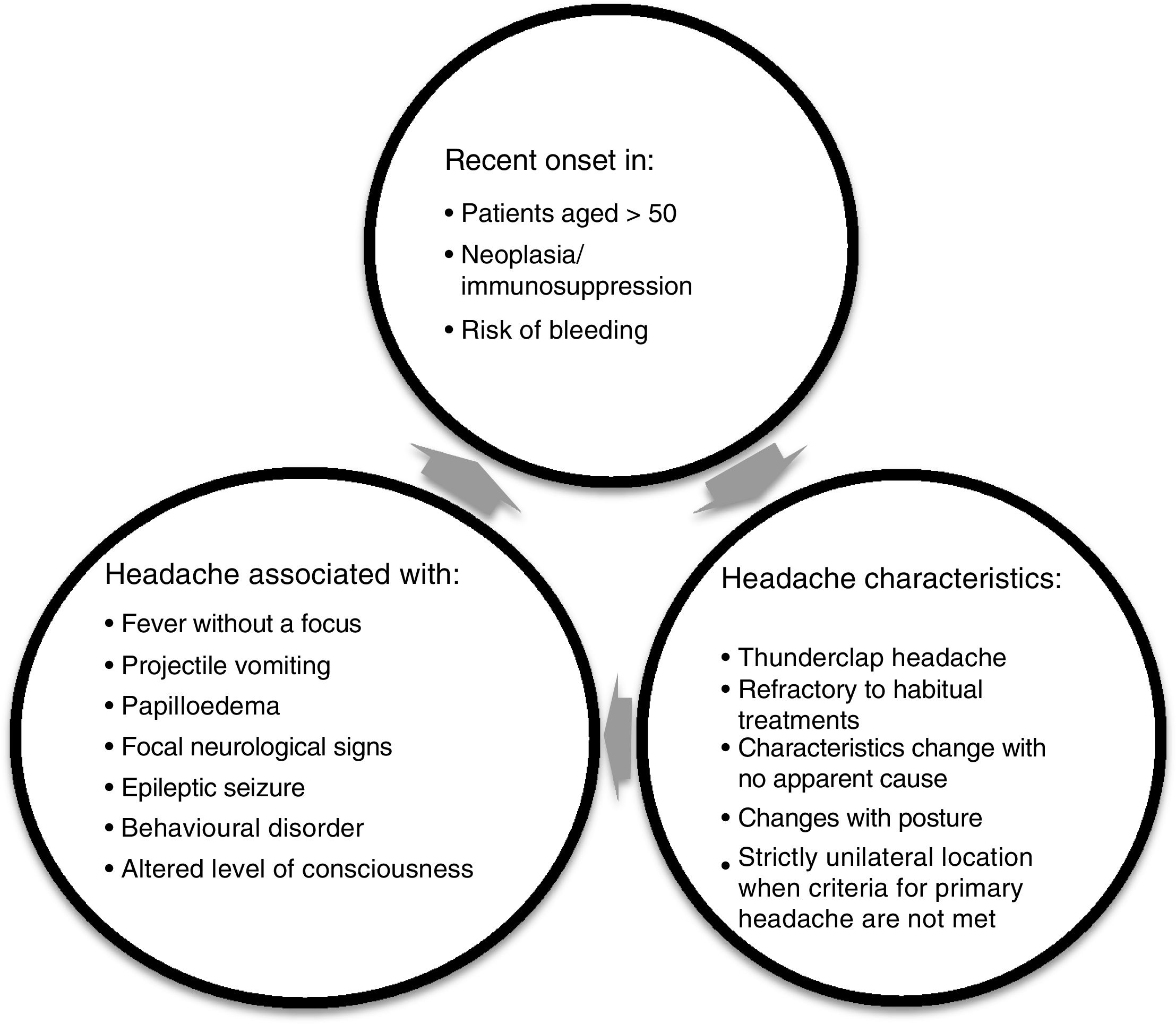
RecommendationsThe most important task when assessing patients with headache, whether in PC or at the emergency department, is to confirm that the patient has no alarm symptoms (Fig. 1). Following this, we can continue assessing the patient and determining how to approach treatment.
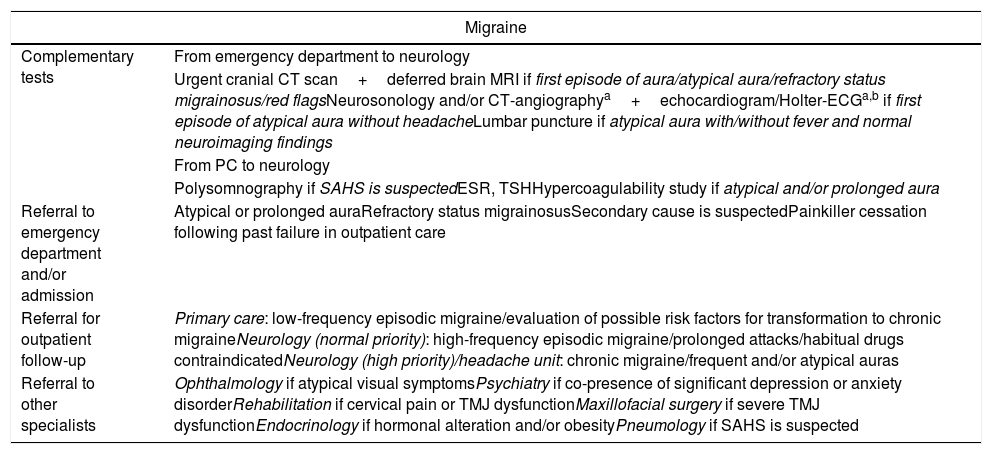
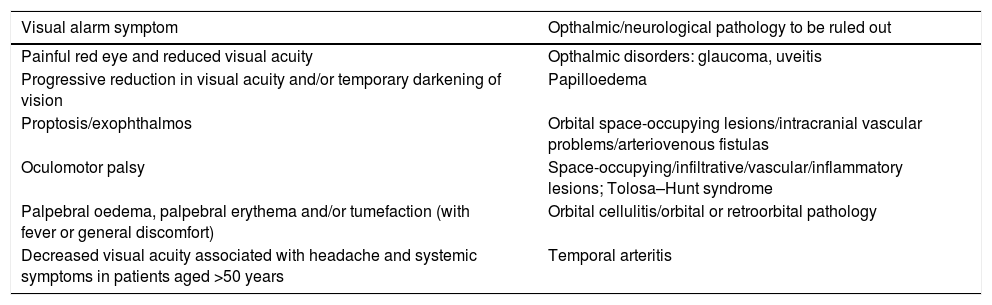
According to the IHCD-3 beta criteria, episodic migraine is a recurring headache with episodes lasting 4-72hours, and is unilateral, pulsatile, of moderate or severe intensity, aggravated by physical activity, and associated with nausea/vomiting and/or photo- or phonophobia, and manifests on fewer than 15 days per month.2 Status migrainosus is defined as a migraine attack lasting more than 72hours and which is refractory to intravenous pharmacological treatment.2 Symptoms may or may not be associated with the presence of aura. The following are grounds to suspect atypical aura: sudden onset, predominance of symptoms of motor involvement (hemiparesis) or negative visual symptoms (loss of sight/hemianopsia), duration greater than 60min, first episode suggestive of aura but not accompanied by headache or visual symptoms, first episode at later ages (>50), history of vascular risk factors and/or absence of a family history of migraine (Table 1).1–6 Patients attending the emergency department for headaches may present a wide range of visual symptoms; both neurological and ophthalmic pathologies must be ruled out (Table 2).
Protocol for action and referral from emergency departments and PC for migraine and aura without headache.
| Migraine | |
|---|---|
| Complementary tests | From emergency department to neurology |
| Urgent cranial CT scan+deferred brain MRI if first episode of aura/atypical aura/refractory status migrainosus/red flagsNeurosonology and/or CT-angiographya+echocardiogram/Holter-ECGa,b if first episode of atypical aura without headacheLumbar puncture if atypical aura with/without fever and normal neuroimaging findings | |
| From PC to neurology | |
| Polysomnography if SAHS is suspectedESR, TSHHypercoagulability study if atypical and/or prolonged aura | |
| Referral to emergency department and/or admission | Atypical or prolonged auraRefractory status migrainosusSecondary cause is suspectedPainkiller cessation following past failure in outpatient care |
| Referral for outpatient follow-up | Primary care: low-frequency episodic migraine/evaluation of possible risk factors for transformation to chronic migraineNeurology (normal priority): high-frequency episodic migraine/prolonged attacks/habitual drugs contraindicatedNeurology (high priority)/headache unit: chronic migraine/frequent and/or atypical auras |
| Referral to other specialists | Ophthalmology if atypical visual symptomsPsychiatry if co-presence of significant depression or anxiety disorderRehabilitation if cervical pain or TMJ dysfunctionMaxillofacial surgery if severe TMJ dysfunctionEndocrinology if hormonal alteration and/or obesityPneumology if SAHS is suspected |
CT, computed tomography; ECG, electrocardiogram; ESR, erythrocyte sedimentation rate; MRI, magnetic resonance imaging; PC, primary care; SAHS, sleep apnoea-hypopnoea syndrome; TMJ: temporomandibular joint; TSH, thyroid stimulating hormone.
Patient with headache and visual alarm symptoms and associated ophthalmic/neurological pathologies to be ruled out.
| Visual alarm symptom | Opthalmic/neurological pathology to be ruled out |
|---|---|
| Painful red eye and reduced visual acuity | Opthalmic disorders: glaucoma, uveitis |
| Progressive reduction in visual acuity and/or temporary darkening of vision | Papilloedema |
| Proptosis/exophthalmos | Orbital space-occupying lesions/intracranial vascular problems/arteriovenous fistulas |
| Oculomotor palsy | Space-occupying/infiltrative/vascular/inflammatory lesions; Tolosa–Hunt syndrome |
| Palpebral oedema, palpebral erythema and/or tumefaction (with fever or general discomfort) | Orbital cellulitis/orbital or retroorbital pathology |
| Decreased visual acuity associated with headache and systemic symptoms in patients aged >50 years | Temporal arteritis |
A headache manifesting 15 or more days per month for over 3 months, showing characteristics of migraine headache with or without aura on at least 8days/month. The patient may also meet diagnostic criteria for medication-overuse headache.2 It is very important to consider modifiable risk factors for transformation to chronic migraine, such as overuse of analgesics or caffeine, mood disorders, sleep apnoea, hormonal disorders, or overweight and obesity (Table 1).1
Tension-type headacheEpisodic tension-type headacheHeadache manifesting fewer than 15 days per month, which is bilateral, oppressive, of mild to moderate intensity, lasts from minutes to days, is not aggravated by physical activity, and which may be associated with mild nausea or photo- or phonophobia (Table 3).2
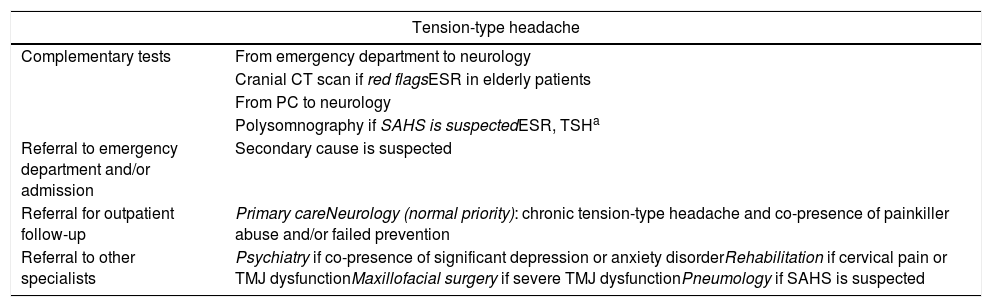
Protocol for action and referral from emergency departments and PC for tension-type headache.
| Tension-type headache | |
|---|---|
| Complementary tests | From emergency department to neurology |
| Cranial CT scan if red flagsESR in elderly patients | |
| From PC to neurology | |
| Polysomnography if SAHS is suspectedESR, TSHa | |
| Referral to emergency department and/or admission | Secondary cause is suspected |
| Referral for outpatient follow-up | Primary careNeurology (normal priority): chronic tension-type headache and co-presence of painkiller abuse and/or failed prevention |
| Referral to other specialists | Psychiatry if co-presence of significant depression or anxiety disorderRehabilitation if cervical pain or TMJ dysfunctionMaxillofacial surgery if severe TMJ dysfunctionPneumology if SAHS is suspected |
CT, computed tomography; ESR, erythrocyte sedimentation rate; SAHS, sleep apnoea and hypopnoea syndrome; TMJ, temporomandibular joint; TSH, thyroid stimulating hormone.
Headache with the characteristics described above, but presenting on 15 or more days per month, for over 3 months (Table 3).2
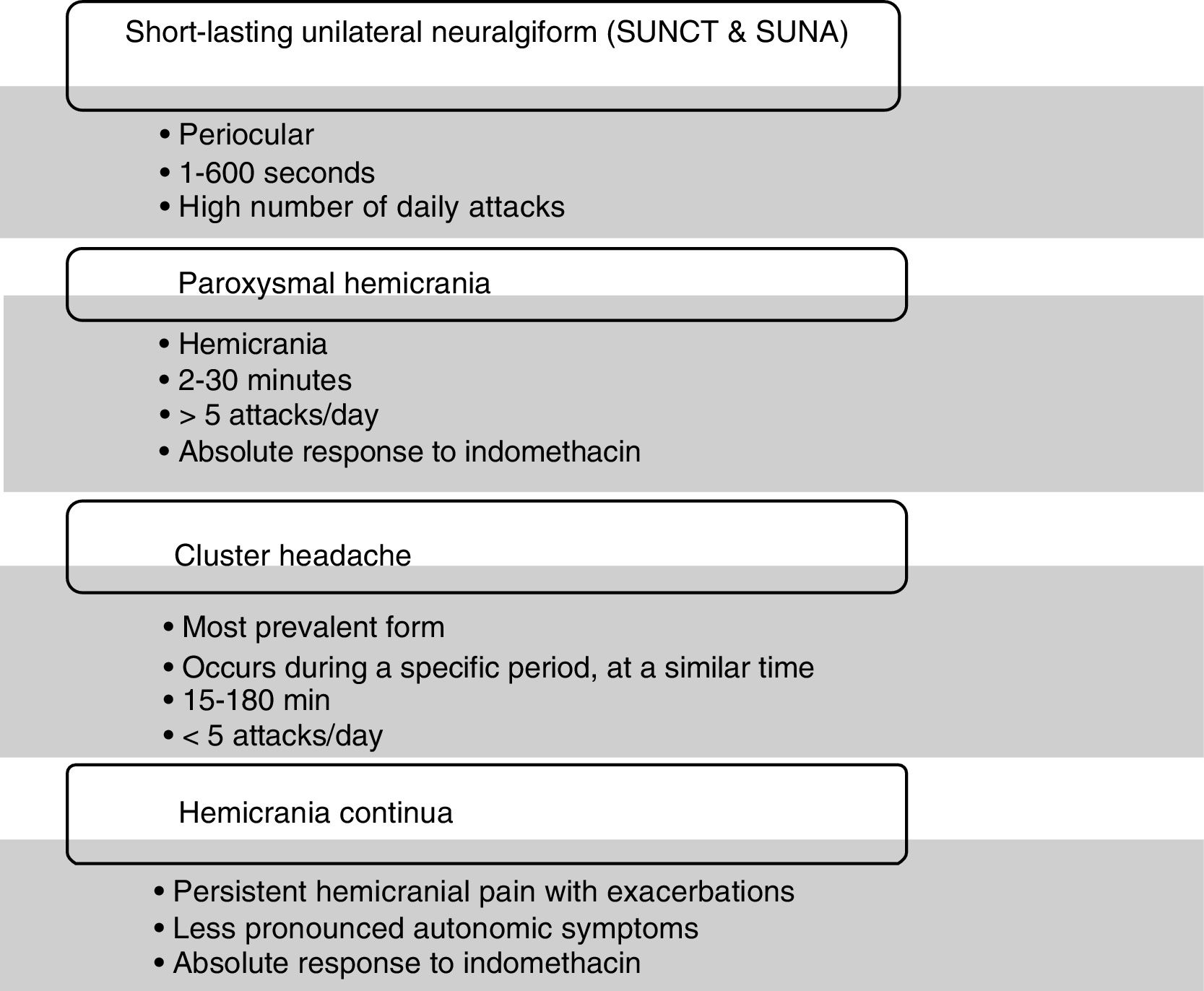
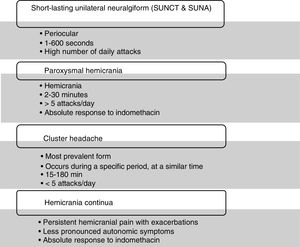
Trigeminal autonomic cephalalgiasTrigeminal autonomic cephalalgias (TACs) are a group of conditions which typically cause a very intense, unilateral pain associated with ipsilateral autonomic symptoms in the face. Symptoms include tearing, conjunctival hyperaemia, ptosis, miosis, rhinorrhoea, a sensation of nasal congestion, perspiration, rubefaction, and a sensation of the ears being blocked. Another characteristic symptom may be anxiety during the episode, particularly in cluster headaches.2,7 All types of TAC present as attacks alternating with periods of remission, with the exception of chronic forms and hemicrania continua, in which there is a persistent, hemicranial background pain.
The group includes various conditions which are clinically differentiated by the duration and frequency of episodes, with each condition showing a specific response to different treatments.8 This group also includes headaches: short-lasting unilateral neuralgiform headache,9–11 paroxysmal hemicrania,12,13 cluster headache,14 and hemicranea continua15,16 (Fig. 2).
These conditions are so disabling that an “open doors” approach is recommended for these patients, as early intervention at the beginning of a new period of episodes can prevent it from becoming chronic and improve the patient's quality of life.
Although they are considered to be primary headaches, in all TACs, cases have been described with symptoms such as trigeminal vascular compression in SUNCT.9 In new-onset headache, generally associated with other neurological symptoms, there are published cases of such vascular pathologies as dissection and perivascular tumours, sinusitis, pituitary gland tumours, sinus thrombosis, vascular fistulas, and ophthalmic pathologies (Table 4).
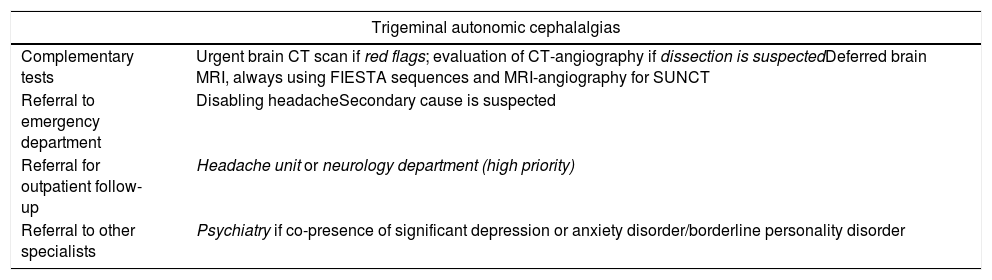
Protocol for action and referral from emergency departments and PC for trigeminal autonomic cephalalgias.
| Trigeminal autonomic cephalalgias | |
|---|---|
| Complementary tests | Urgent brain CT scan if red flags; evaluation of CT-angiography if dissection is suspectedDeferred brain MRI, always using FIESTA sequences and MRI-angiography for SUNCT |
| Referral to emergency department | Disabling headacheSecondary cause is suspected |
| Referral for outpatient follow-up | Headache unit or neurology department (high priority) |
| Referral to other specialists | Psychiatry if co-presence of significant depression or anxiety disorder/borderline personality disorder |
This group is heterogeneous. In a patient's first episode, urgent neuroimaging study is recommended in order to rule out severe secondary headache. Patients attending consultation for recurring episodes and not presenting alarm signs can be prioritised for neurology studies (Table 5).
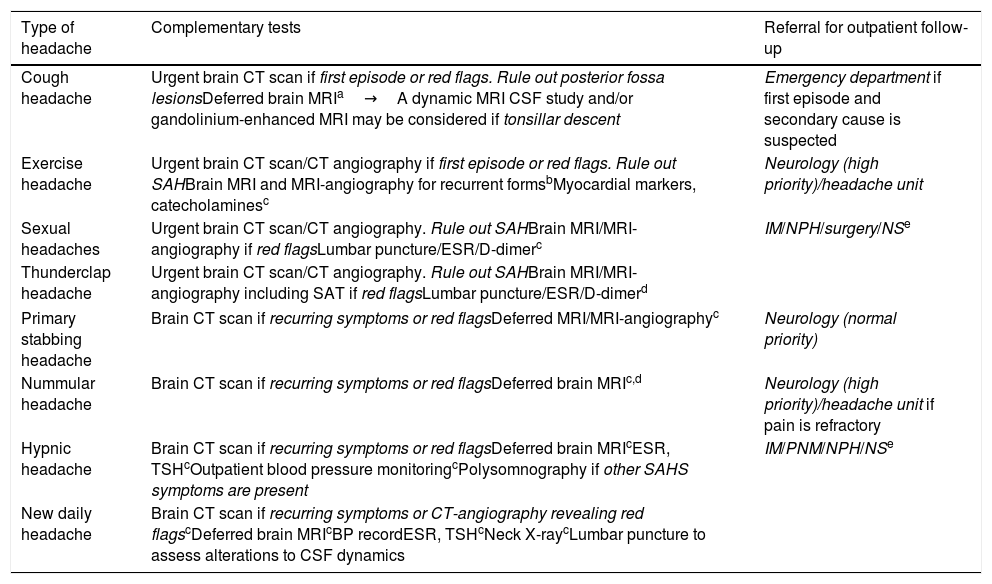
Protocol for action and referral from emergency departments and PC for other primary headaches.
| Type of headache | Complementary tests | Referral for outpatient follow-up |
|---|---|---|
| Cough headache | Urgent brain CT scan if first episode or red flags. Rule out posterior fossa lesionsDeferred brain MRIa→A dynamic MRI CSF study and/or gandolinium-enhanced MRI may be considered if tonsillar descent | Emergency department if first episode and secondary cause is suspected |
| Exercise headache | Urgent brain CT scan/CT angiography if first episode or red flags. Rule out SAHBrain MRI and MRI-angiography for recurrent formsbMyocardial markers, catecholaminesc | Neurology (high priority)/headache unit |
| Sexual headaches | Urgent brain CT scan/CT angiography. Rule out SAHBrain MRI/MRI-angiography if red flagsLumbar puncture/ESR/D-dimerc | IM/NPH/surgery/NSe |
| Thunderclap headache | Urgent brain CT scan/CT angiography. Rule out SAHBrain MRI/MRI-angiography including SAT if red flagsLumbar puncture/ESR/D-dimerd | |
| Primary stabbing headache | Brain CT scan if recurring symptoms or red flagsDeferred MRI/MRI-angiographyc | Neurology (normal priority) |
| Nummular headache | Brain CT scan if recurring symptoms or red flagsDeferred brain MRIc,d | Neurology (high priority)/headache unit if pain is refractory |
| Hypnic headache | Brain CT scan if recurring symptoms or red flagsDeferred brain MRIcESR, TSHcOutpatient blood pressure monitoringcPolysomnography if other SAHS symptoms are present | IM/PNM/NPH/NSe |
| New daily headache | Brain CT scan if recurring symptoms or CT-angiography revealing red flagscDeferred brain MRIcBP recordESR, TSHcNeck X-raycLumbar puncture to assess alterations to CSF dynamics | |
BP, blood pressure; CSF, cerebrospinal fluid; CT, computed tomography; ESR, erythrocyte sedimentation rate; IM, internal medicine; MRI, magnetic resonance imaging; NPH, nephrology; NS, neurosurgery; PNM, pneumology; SAT, supra-aortic trunks; TSH, thyroid stimulating hormone.
A primary headache caused by coughing, with no other intracranial structural abnormalities. People aged below 40 are rarely affected. It predominantly affects men, and is responsive to indomethacin. Duration is short (seconds to minutes), with onset immediately or a few seconds after coughing or other Valsalva manoeuvres, such as when lifting weights. It is typically bilateral and occipital or frontal, acute with moderate to severe intensity, and stabbing or explosive (Table 6).2,17
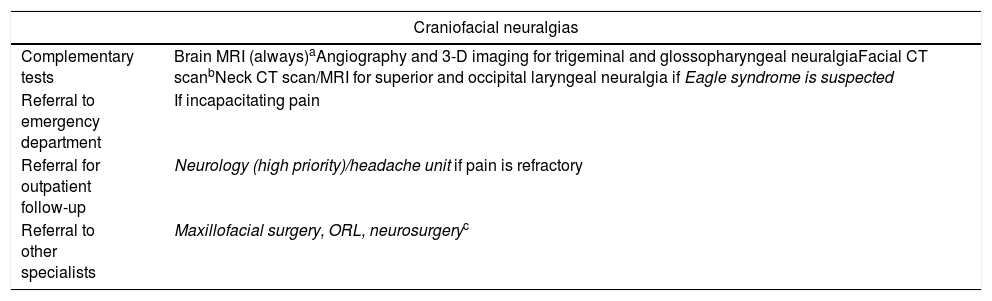
Protocol for action and referral from emergency departments and PC for the main craniofacial neuralgias.
| Craniofacial neuralgias | |
|---|---|
| Complementary tests | Brain MRI (always)aAngiography and 3-D imaging for trigeminal and glossopharyngeal neuralgiaFacial CT scanbNeck CT scan/MRI for superior and occipital laryngeal neuralgia if Eagle syndrome is suspected |
| Referral to emergency department | If incapacitating pain |
| Referral for outpatient follow-up | Neurology (high priority)/headache unit if pain is refractory |
| Referral to other specialists | Maxillofacial surgery, ORL, neurosurgeryc |
CT, computed tomography; IAC, internal auditory canal; MRI, magnetic resonance imaging; ORL, otorhinolaryngology.
Headache triggered by coughing is secondary in 20% of cases, typically caused by Chiari malformation type 1 or posterior fossa lesions.18,19
Primary exercise headachePain is triggered by intense and/or prolonged physical exercise. Young men with migraine are predominantly affected. Headache occurs at peak of exercise and remits with rest. Pain is typically pulsatile or stabbing, lasting less than 48hours, and may be accompanied by migraine symptoms.2,17
In 80% of cases, recurrent headaches associated with exercise are primary.17 Cardiac ischaemia (cardiac cephalalgia) must be ruled out in older patients and patients with cardiovascular risk factors or a history of ischaemic heart disease.20 Cases have been described of exercise headaches secondary to pheochromocytoma, intracranial hyper- or hypotension, or venous sinus thrombosis; clinical judgement should determine the need for investigation.18
Primary headache associated with sexual activityHeadache occurs only during sexual activity. Location is occipital and bilateral; pain is intense and occurs at climax or as sexual excitement increases, improving when the activity stops (within 24h). It typically occurs in middle-aged adults, predominantly in men, and co-presents with migraine.2,17
Primary sexual headache is usually recurrent. Cases have been described of sexual headache secondary to subarachnoid haemorrhage, arterial dissection, reversible cerebral vasoconstriction syndrome, or arterial hypertension. These conditions should particularly be suspected in women, people older than 40-50 years, and patients with prolonged episodes, loss of consciousness, or nuchal rigidity.18,19
Primary thunderclap headacheClinical presentation is similar to that of aneurysm rupture, and occurs repetitively without the presence of any intracranial structural lesion. Onset is sudden, reaching maximum intensity in less than 60seconds, and can last hours or even weeks. Pain is spontaneous or triggered by exercise, sexual activity, or hyperventilation. Location is typically occipital; headache may be accompanied by nausea and vomiting.2,17
Evaluation of potential secondary causes must be swift and exhaustive; it is essential to rule out intracerebral haemorrhage, subarachnoid haemorrhage, cerebral venous thrombosis, vascular malformations, arterial dissection, reversible cerebral vasoconstriction syndrome, pituitary apoplexy, meningitis, colloid cyst of the third ventricle, CSF hypotension, and acute sinusitis.19,21
Primary stabbing headacheHeadache takes the form of transitory stabs of pain, short in duration (seconds), with irregular frequency (one or multiple per day) and variable cranial location, and is not accompanied by autonomic symptoms.2,17 The condition is common, predominantly affecting young women, and co-presents with migraine.21,22
Main differential diagnosis should consider other primary headaches, such as SUNCT, paroxysmal hemicrania, and trigeminal neuralgia.17
Nummular headacheCranial pain in a fixed, sharply contoured, circular or oval area, measuring 1-6cm in diameter. Pain is oppressive or stabbing, mild to moderate in intensity and associated with intense paroxysms. Half of patients show some kind of sensory alteration (allodynia, hypoaesthesia, paraesthesia), or even dermatologic alterations (alopecia, change in hair colour, or skin atrophy). Around 10% of patients have a history of local trauma. Nummular headache can occur at any age and affects women more than men.23
Secondary cases have been described due to: fusiform aneurysm of a branch of the superficial temporal artery, cranial fibrous dysplasia, Paget disease, meningioma, arachnoid cysts, insect bites, and pituitary adenoma resection.24,25
Hypnic headacheThis condition is uncommon, typically presents at older ages and predominantly in women, and is mainly characterised by occurring exclusively during sleep. Patients typically experience one attack per night, lasting from 15minutes to 4hours, 10 or more nights per month; pain commonly occurs at the same time every night (mainly between 2 and 4am). Patients report a moderate, dull pain which is frontotemporal and bilateral or holocranial. It can be associated with mild vegetative symptoms (nausea). Patients often respond to pain by occupying themselves with some peaceful activity, unlike with migraine (where they tend to seek rest) and TACs (which are generally accompanied by agitation).2
Cases have been described of hypnic headache secondary to posterior fossa or brainstem lesions (meningioma, cerebellar haemangioblastoma) and pituitary gland lesions (non-functioning pituitary macroadenoma), sleep apnoea-hypopnoea syndrome (SAHS), nocturnal arterial hypertension, withdrawal from such drugs as lithium or ACE inhibitors, or symptomatic medication overuse.26–28
New persistent daily headacheHeadache occurs every day from onset, for at least 3 months. Patients very frequently remember the precise day and circumstances of pain onset, although it is possible in fewer than half of cases to identify a trigger (infection, stressful event, surgery, substance exposure). Semiological characteristics are not relevant in defining this type of headache. It is more common in women, and can manifest at any age, particularly in the second and third decades of life.
It is essential to rule out secondary causes, such as intracranial hypertension (idiopathic or secondary) or CSF hypotension, overuse of symptomatic medication, chronic meningitis, chronic subdural haematoma, cervical artery dissection, cerebral venous thrombosis, arteriovenous malformation, dural arteriovenous fistula, giant cell arteritis, and cervicogenic headache.19–31
Craniofacial neuralgiasNeuralgias have been described both in the main nerve trunks and in the terminal branches of these nerves.1
Trigeminal neuralgiaThis is the most frequent type of neuralgia.32 It is characterised by brief (less than 2minutes), very intensely painful, stabbing or electric-shock-like paroxysms, triggered by stimuli including chewing or local palpation.2 There is usually a refractory period during which a new attack cannot be triggered. The second and third branches are most frequently affected, with first branch involvement being very rare (<5%).1
Classic trigeminal neuralgia accounts for 90% of cases, and is caused by a vascular kink compressing the nerve root.1 In cases where exploration reveals alterations such as local hypoaesthesia, abolished corneal reflex, or alterations in other cranial nerves, secondary causes (slow-growing tumours, cranial base abnormalities, vascular malformations, demyelinating lesions, or brainstem stroke) should be suspected.1
Neuralgia has been described in the terminal branch of the trigeminal nerve, with a burning, stinging pattern of pain. These are supra- and infraorbital neuralgia, mental nerve neuralgia, nasociliary neuralgia, auriculotemporal neuralgia, supra- and infratrochlear neuralgia and lacrimal neuralgia. The possibility of tumoural aetiology should be accounted for, particularly in the case of mental and infraorbital nerve involvement, (numb chin and numb cheek syndrome, respectively).33
Nervus intermedius neuralgiaNeuralgia caused by alterations affecting the seventh cranial nerve and characterised by attacks of acute pain deep in the ear canal.1 Typical triggers include tragal pressure, cold, noise, and chewing.1
Glossopharyngeal neuralgiaGlossopharyngeal neuralgia is caused by irritation of the ninth cranial nerve, in the majority of cases due to a kink in the ipsilateral PICA.1 Patients experience pain in the periauricular region and/or the posterior third of the tongue, the pharynx, and the tonsillar region.1 Typical triggers are coughing, swallowing, sneezing, or yawning. In addition to paroxysms of typically lancinating pain, a burning or dull pain may be experienced between attacks.1 Secondary causes include demyelinating lesions, local tumours, tonsillar abscesses, Chiari malformations and vascular aneurysms. It is important for differential diagnosis to consider Eagle syndrome; this syndrome features pharyngeal pain, which may be paroxysmal and triggered by swallowing, and may be reproduced with pressure on the ipsilateral tonsillar fossa. This syndrome is caused by calcification of the stylohyoid ligament.34
Superior laryngeal neuralgiaThis neuralgia affects the tenth cranial nerve. It is characterised by attacks of lancinating pain in the anterolateral region of the neck, triggered by swallowing, turning of the neck, shouting, or singing.1
Occipital neuralgiasOccipital neuralgias are characterised by continuous or paroxysmal pain in the occipital region, often radiating to the upper parietal or even the frontal region. Typically, there is local sensitivity which reproduces the pain. These neuralgias are often associated with pathologies affecting the neck. They most commonly affect the greater occipital nerve, although cases have also been described in the lesser occipital and third occipital nerves.
ConclusionsBetter understanding of complementary tests, of criteria for referral to emergency departments and for admission, of which specialists should evaluate patients, and of how referral should be sought, will enable better treatment of patients with headache, both from PC physicians and emergency departments. However, this demonstrates many of the shortfalls seen in a great majority of centres at the national level, which lack headache units or the sufficient specialist clinics to guarantee that patients be managed with the necessary level of priority and that the proper tests are requested. Referring to official recommendations in order to optimise these issues will help to improve quality of life for patients with such a debilitating condition as headache, which on occasions also conceals less benign processes.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Gago-Veiga AB, García-Azorín D, Mas-Sala N, Ordás CM, Ruiz-Piñero M, Torres-Ferrús M, et al. Cómo y cuándo derivar un paciente con cefalea primaria y neuralgia craneofacial desde Urgencias y Atención Primaria: recomendaciones del Grupo de Estudio de Cefalea de la Sociedad Española de Neurología. Neurología. 2020;35:176–184.