Smartphone use in biomedical research is becoming more prevalent in different clinical settings. We performed a pilot study to obtain information on smartphone use by patients with essential tremor (ET) and healthy controls, with a view to determining whether performance of touchscreen tasks is different between these groups and describing touchscreen interaction factors.
MethodA total of 31 patients with ET and 40 sex- and age-matched healthy controls completed a descriptive questionnaire about the use of smartphones. Participants subsequently interacted with an under-development Android application, and performed 4 tests evaluating typical touchscreen interaction gestures; each test was performed 5 times.
ResultThe type of smartphone use and touchscreen interaction were not significantly different between patients and controls. Age and frequency of smartphone use are key factors in touchscreen interaction.
ConclusionOur results support the use of smartphone touchscreens for research into ET, although further studies are required.
El uso de smartphones en investigación biomédica está creciendo rápidamente en diferentes entornos clínicos. Realizamos un estudio piloto para obtener información sobre el uso de smartphones en pacientes con temblor esencial (TE) y en sujetos sanos, con el objetivo de evaluar si la realización de diversas tareas con las pantallas táctiles difiere entre grupos y describir factores de esta interacción.
MétodoSe administró un cuestionario sobre el uso de smartphones a 31 pacientes con TE y 40 sujetos control apareados por edad y sexo. Acto seguido, los participantes interactuaron con una aplicación Android en desarrollo y realizaron 4 test basados en diferentes modos de interacción típicos con pantallas táctiles, con 5 repeticiones de cada tarea.
ResultadoLos tipos de uso de smartphones así como su interacción no fueron significativamente diferentes entre pacientes y controles. La edad y el número de usos del smartphone son factores clave en esta interacción con pantallas táctiles.
ConclusiónEstas observaciones apoyan el uso de las pantallas táctiles de los smartphones para investigación en TE, pero se requieren más estudios.
The growth in the number of smartphone users1,2 and health-related mobile applications (mHealth)3 presents opportunities for the rapid collection of relevant user lifestyle data over wireless connections.4 This field is particularly promising for research as it may provide large quantities of instantly-accessible medical information on numerous diseases.5 These data may be purely informative, but could also be used for interactive management.1,6 Research is being conducted in various fields of medicine to personalise patient care through a number of technological platforms. There is growing interest in the use of smartphones in public health. However, most of these platforms require users to interact in some way with these devices. The technical characteristics of smartphone touchscreens (size, interface, programs, etc.) vary greatly. Another line of research revolves around the characteristics of user interaction.7 Numerous technical characteristics have been evaluated in various user populations; the majority of studies include healthy individuals from a variety of age groups,8,9 as well as disabled people.10–12 For example, Parkinson's disease has been shown to affect interaction with smartphone screens by tapping.13
Essential tremor (ET) is one of the most prevalent movement disorders in adults, affecting 5% of people aged over 65.14 Tremor is affected by posture and limb movements.15 Tremor intensity is evaluated with such tools as the Fahn–Tolosa–Marin Tremor Rating Scale (FTM-TRS).16 However, these tools do not assess the ability to use smart devices, which are ubiquitous in today's society. Several methods have been developed to assist patients with tremor and other movement disorders in interacting with touchscreens.5,17,18 However, no previous study has used an application to compare between touchscreen interaction in patients with ET and in controls.
This pilot study aims to describe these patients’ use of smartphones and the factors influencing interaction with touchscreens in patients with ET and in a group of age- and sex-matched controls. We also aim to assess whether the 2 groups may behave differently in tasks involving touchscreen interaction, indicating poor interaction in patients with ET.
Material and methodsStudy designWe performed a case–control study of consecutively recruited patients with ET and healthy individuals; participants were recruited at our neurology outpatient clinic. We used written questionnaires for data collection, and tested an Android smartphone application requiring users to perform 4 touch interaction tasks.
The study was approved by the bioethics committee of Hospital Universitario 12 de Octubre (Madrid, Spain). All participants gave written informed consent.
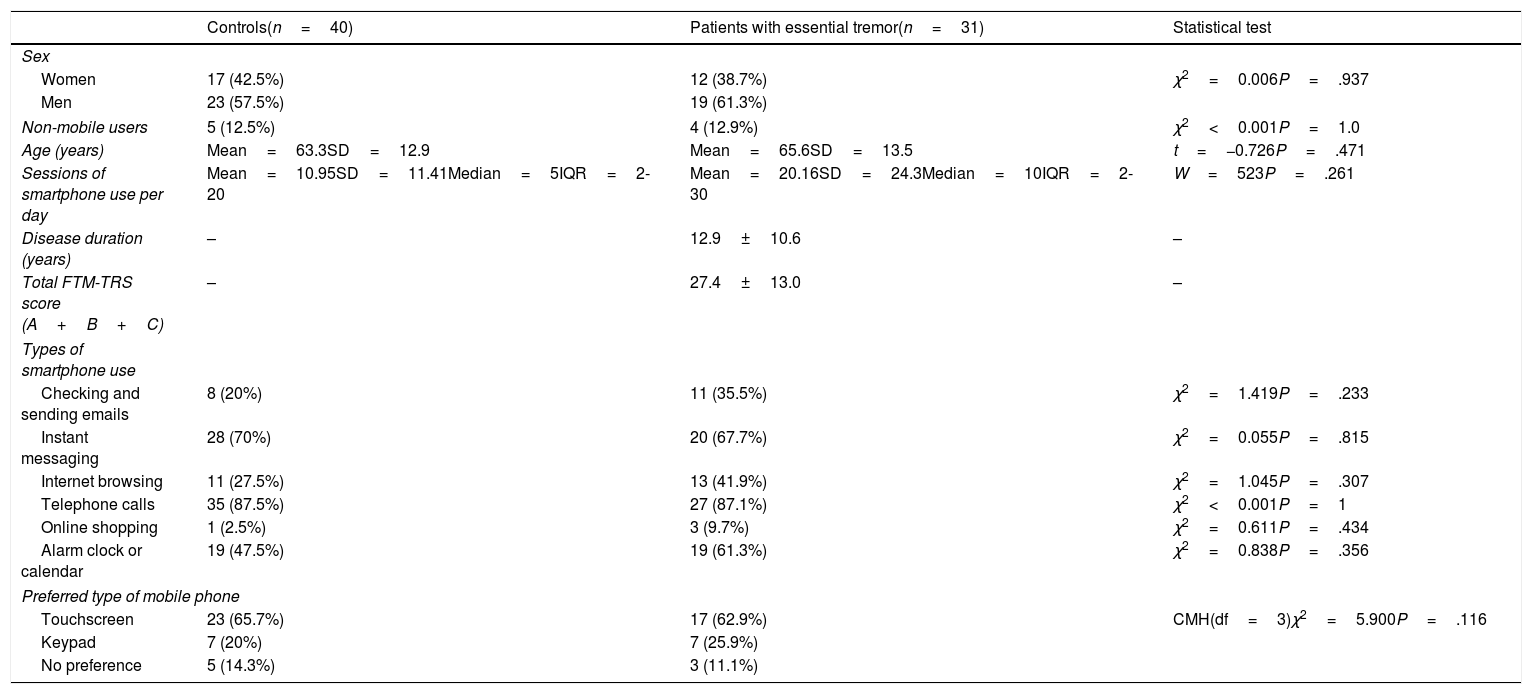
Study population and procedureThirty-one patients with ET and 40 healthy individuals, all aged between 18 and 85, met the study inclusion criteria and agreed to participate. Table 1 lists participants’ demographic characteristics and questionnaire results. A brief description of the patients with ET is provided as supplementary material. Tremor intensity was mild to moderate, scoring between 1 and 60 on the FTM-TRS.
Participants’ demographic characteristics at baseline, including questionnaire results and the statistical tests used.
| Controls(n=40) | Patients with essential tremor(n=31) | Statistical test | |
|---|---|---|---|
| Sex | |||
| Women | 17 (42.5%) | 12 (38.7%) | χ2=0.006P=.937 |
| Men | 23 (57.5%) | 19 (61.3%) | |
| Non-mobile users | 5 (12.5%) | 4 (12.9%) | χ2<0.001P=1.0 |
| Age (years) | Mean=63.3SD=12.9 | Mean=65.6SD=13.5 | t=−0.726P=.471 |
| Sessions of smartphone use per day | Mean=10.95SD=11.41Median=5IQR=2-20 | Mean=20.16SD=24.3Median=10IQR=2-30 | W=523P=.261 |
| Disease duration (years) | – | 12.9±10.6 | – |
| Total FTM-TRS score (A+B+C) | – | 27.4±13.0 | – |
| Types of smartphone use | |||
| Checking and sending emails | 8 (20%) | 11 (35.5%) | χ2=1.419P=.233 |
| Instant messaging | 28 (70%) | 20 (67.7%) | χ2=0.055P=.815 |
| Internet browsing | 11 (27.5%) | 13 (41.9%) | χ2=1.045P=.307 |
| Telephone calls | 35 (87.5%) | 27 (87.1%) | χ2<0.001P=1 |
| Online shopping | 1 (2.5%) | 3 (9.7%) | χ2=0.611P=.434 |
| Alarm clock or calendar | 19 (47.5%) | 19 (61.3%) | χ2=0.838P=.356 |
| Preferred type of mobile phone | |||
| Touchscreen | 23 (65.7%) | 17 (62.9%) | CMH(df=3)χ2=5.900P=.116 |
| Keypad | 7 (20%) | 7 (25.9%) | |
| No preference | 5 (14.3%) | 3 (11.1%) | |
CMH: Cochran-Mantel-Haenszel test; df: degrees of freedom; FTM-TRS: Fahn-Tolosa-Marin Tremor Rating Scale; IQR: interquartile range; SD: standard deviation; W: Wilcoxon test.
ET was diagnosed according to the consensus criteria established by the Movement Disorder Society.15 We excluded patients with history of dementia, stroke, epilepsy, brain injury, or visual/auditory alterations. No patient had a pacemaker or brain stimulation device. Healthy controls were recruited from among the companions (friends and family members) of patients visiting the clinic for reasons unrelated to ET (eg, dizziness, headache). Controls had no relatives with ET within 2 degrees of consanguinity. Controls were matched to patients by age and sex. Candidates for inclusion as controls underwent a neurological examination (conducted by RLB, SLV, or JPR) to rule out any relevant neurological diseases or other disorders; the examination considered other movement disorders, dementia, stroke, epilepsy, and brain injury. Participants completed a questionnaire on smartphone use (Table 1), then completed 4 tasks using an under-development mobile application (Supplementary Material).
DeviceTests were performed on a BQ Aquaris E4.5 Android smartphone with a 4.5-inch screen (67.00×137.00mm; 540×960pixels) with 24-bit colour depth and in-plane switching technology. Screen brightness was set to maximum to ensure content was properly displayed. The exercises included in the Android application were designed by Experis IT and comprised 4 tasks based on finger touches (each task was repeated 5 times). These tasks were intended to reflect the most common types of interaction with touchscreen interfaces (Supplementary Material).
- 1.
Basic tapping: participants had to touch a circle of 15mm diameter, which appeared at a random location on the screen.
- 2.
Sequential tapping: participants had to type numbers appearing on-screen using the virtual keypad.
- 3.
Double-tapping: participants had to switch off an alarm by tapping twice on a 15-mm circle.
- 4.
Unlocking/dragging: participants had to switch off an alarm by touching a 15-mm circle and dragging it across the screen to a target.
Tests were performed with participants holding the smartphone in their hands, on top of a table. All participants received several minutes of training before performing the test. They were asked to use their dominant hand and to begin each repeat of the tasks with their hand resting on the table near the smartphone.
Outcome variablesA closed questionnaire was used to collect data on participants’ smartphone use (Table 1).
Interaction with touchscreens was estimated based on 2 parameters: (1) accuracy in tasks 1 and 2 (measured on a 6-level ordinal scale [0%, 20%, …, 100%]), and (2) mean time taken to complete tasks 3 (3A: time taken to switch off alarm with 2 taps; 3B: time between taps) and 4 (time taken to perform dragging task).
Statistical analysisStatistical analysis was performed using the RStudio software (RStudio: Integrated development environment for R [Version 1.0.136]; Boston, MA, USA; retrieved 21 December 2016). Quantitative variables were tested for normal distribution using the Shapiro–Wilk test. We performed a descriptive analysis of questionnaire results. The t test, Wilcoxon test (W), chi-square test (χ2), and Cochran-Mantel-Haenszel test were used to detect differences between groups. Correlations between quantitative measures were determined with the Spearman correlation coefficient (Rho).
ResultsDescriptive statisticsAge at the time of study inclusion ranged from 19 to 82 years (mean, 65.6±13.5) in the ET group and from 30 to 83 (63.3±12.9) in the control group; both groups were made up of approximately 40% women and 60% men. A similar percentage of individuals in both groups (12%) reported no mobile phone use. The ET group's estimate of the number of times they used a smartphone per day was around twice the figure estimated by members of the control group; this difference was not statistically significant, however (W=523; P=.261). In the questionnaire, both groups reported similar preferences in terms of smartphone use. Cases and controls were matched by age and sex (Table 1).
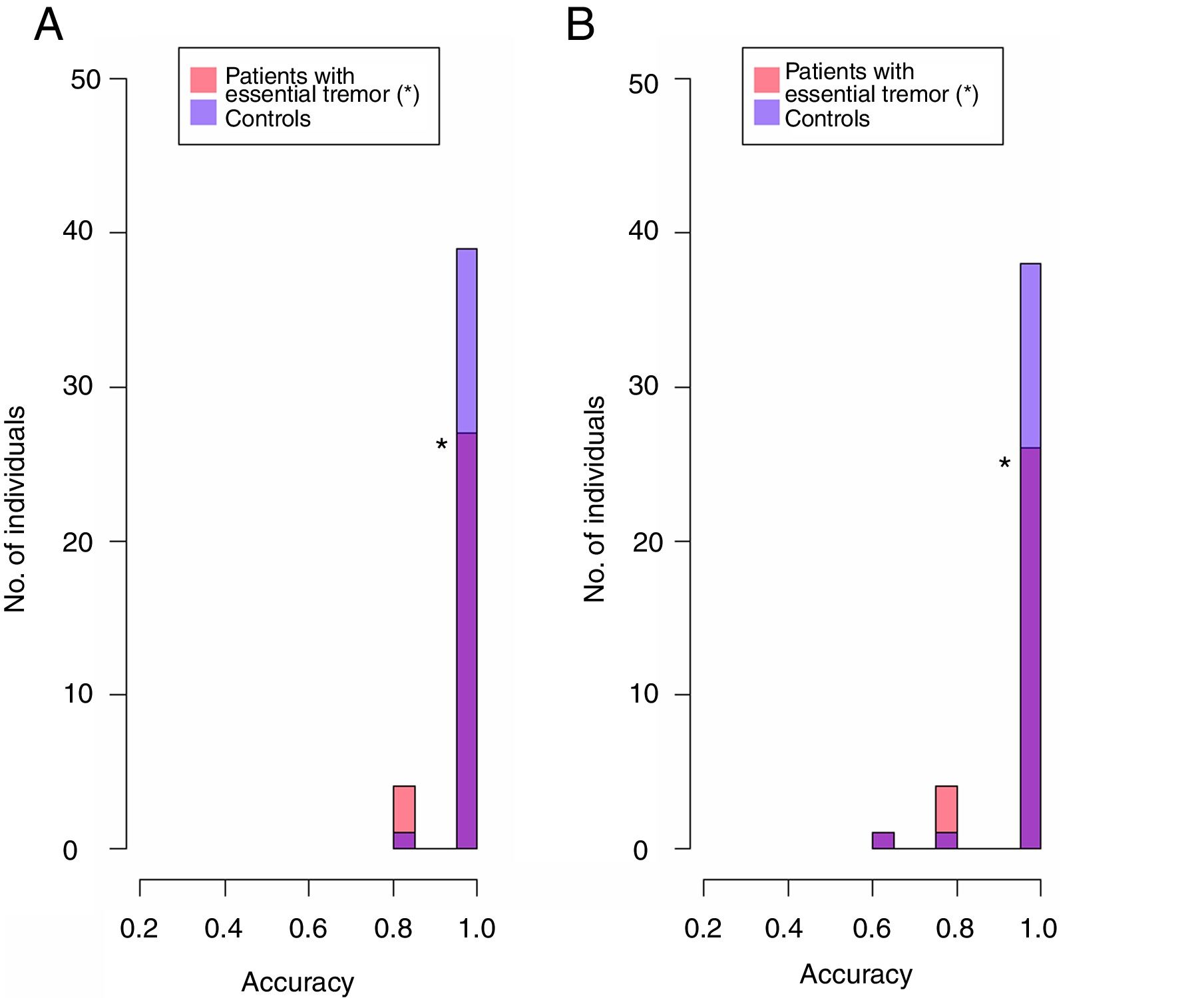
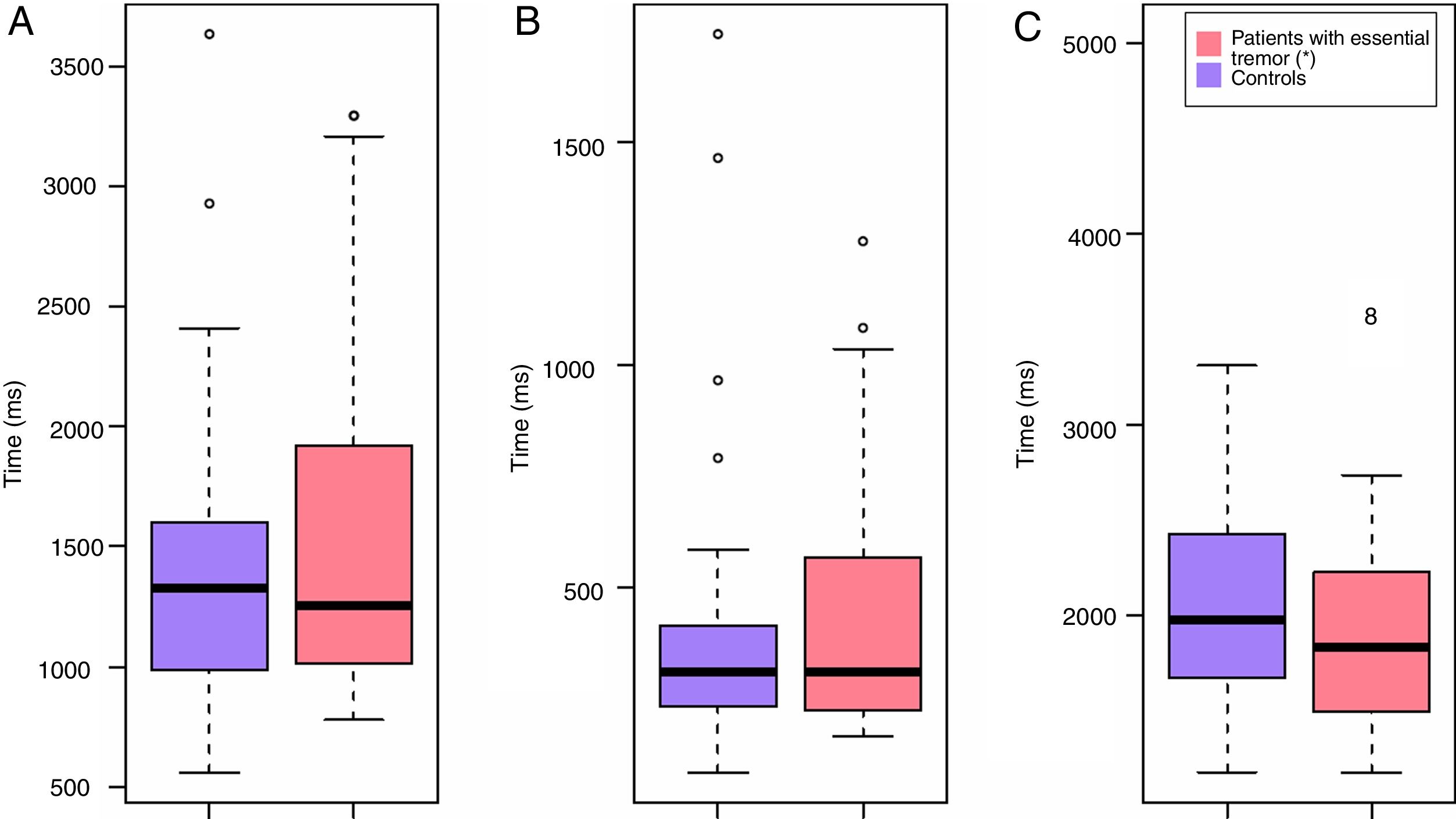
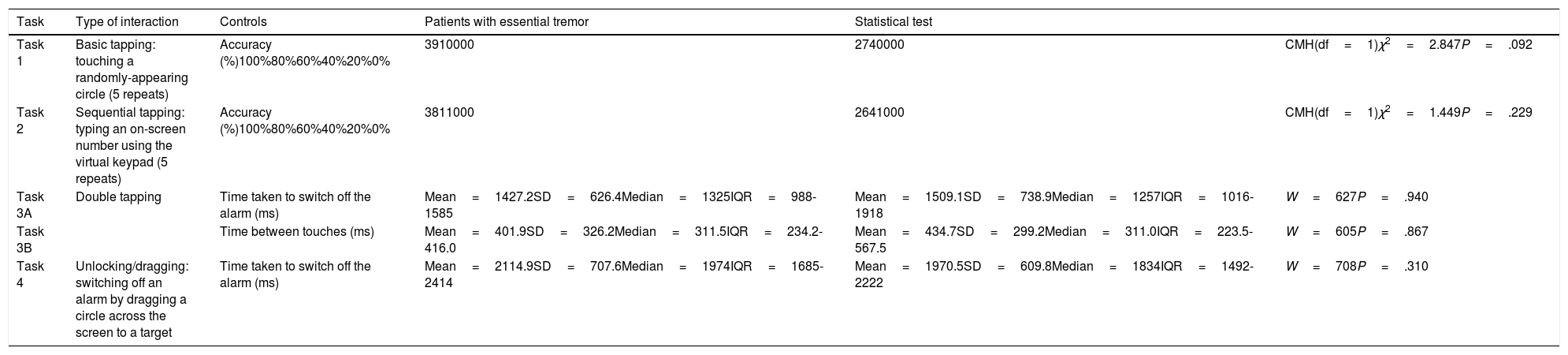
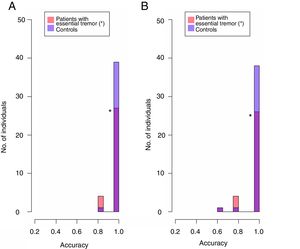
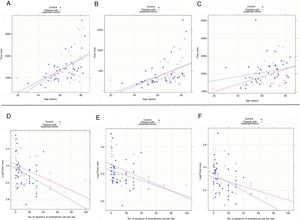
Task performanceFigs. 1 and 2 and Table 2 show results from touchscreen tasks. No differences were observed between patients and controls for any task.
Performance in smartphone application tasks.
| Task | Type of interaction | Controls | Patients with essential tremor | Statistical test | |
|---|---|---|---|---|---|
| Task 1 | Basic tapping: touching a randomly-appearing circle (5 repeats) | Accuracy (%)100%80%60%40%20%0% | 3910000 | 2740000 | CMH(df=1)χ2=2.847P=.092 |
| Task 2 | Sequential tapping: typing an on-screen number using the virtual keypad (5 repeats) | Accuracy (%)100%80%60%40%20%0% | 3811000 | 2641000 | CMH(df=1)χ2=1.449P=.229 |
| Task 3A | Double tapping | Time taken to switch off the alarm (ms) | Mean=1427.2SD=626.4Median=1325IQR=988-1585 | Mean=1509.1SD=738.9Median=1257IQR=1016-1918 | W=627P=.940 |
| Task 3B | Time between touches (ms) | Mean=401.9SD=326.2Median=311.5IQR=234.2-416.0 | Mean=434.7SD=299.2Median=311.0IQR=223.5-567.5 | W=605P=.867 | |
| Task 4 | Unlocking/dragging: switching off an alarm by dragging a circle across the screen to a target | Time taken to switch off the alarm (ms) | Mean=2114.9SD=707.6Median=1974IQR=1685-2414 | Mean=1970.5SD=609.8Median=1834IQR=1492-2222 | W=708P=.310 |
CMH: Cochran-Mantel-Haenszel test; df: degrees of freedom; IQR: interquartile range; SD: standard deviation; W: Wilcoxon test.
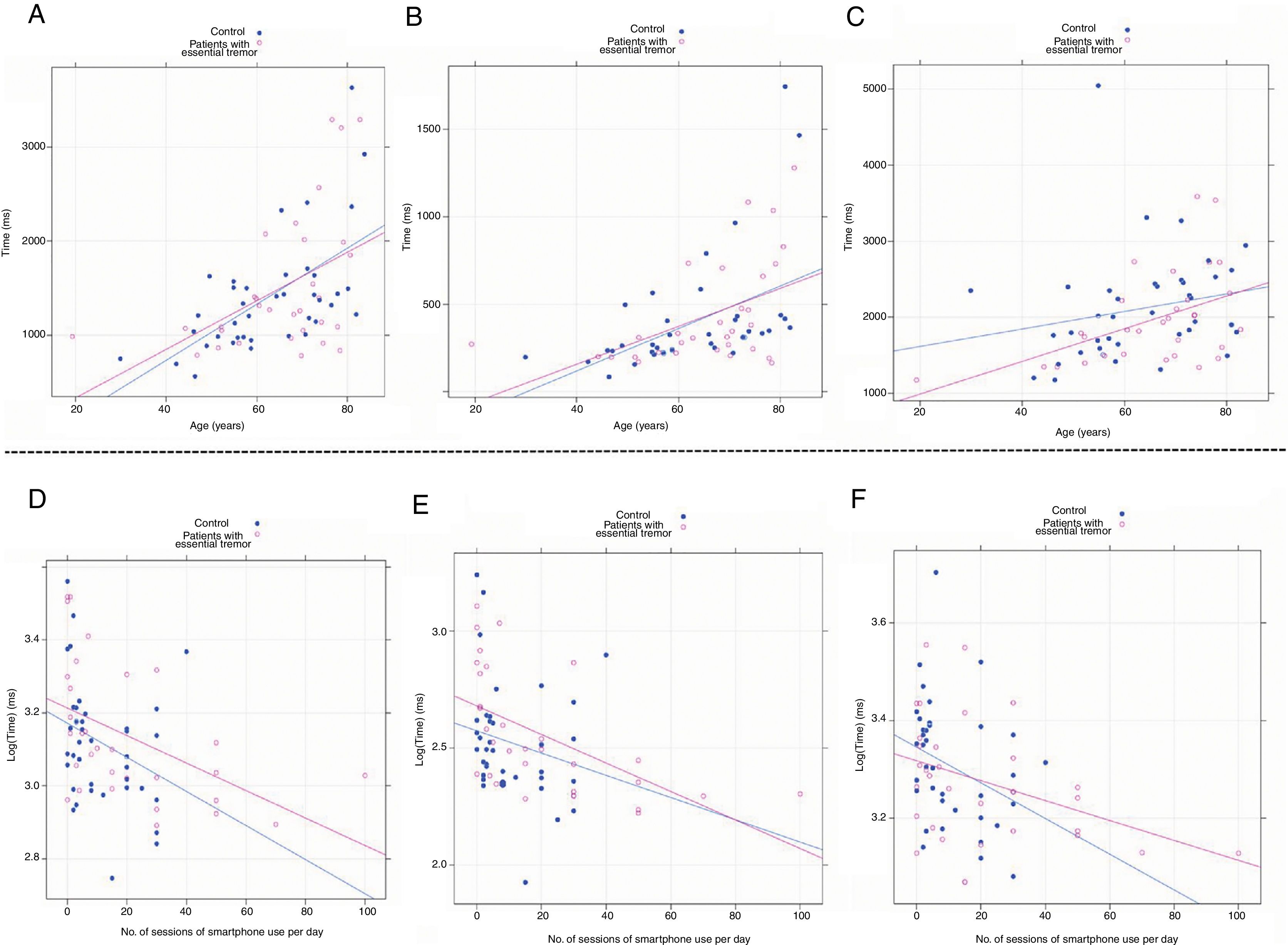
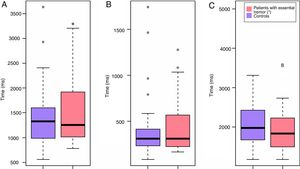
Age was directly correlated with the time taken to perform the task. Estimated smartphone use showed an inverse relation with time taken approaching a logarithmic scale (Fig. 3).
Associations between time taken to complete tasks and age and smartphone use. Patients with ET are shown in red; controls are shown in blue. (A-C) Association with age: tests 3A, 3B, and 4, respectively. (D-F) Association between smartphone use (logarithmic scale) and the time taken to perform tasks 3A, 3B, and 4, respectively.
Spearman correlation coefficients between age and time taken to perform the various tasks were as follows: task 3A, Rho=0.569 (P<.001); task 3B, Rho=0.597 (P<.001); task 4, Rho=0.408 (P<.001) (Fig. 3A-C). Estimated smartphone use showed an inverse correlation with time taken in tasks 3A (Rho=−0.494, P<.001), 3B (Rho=−0.523, P<.001), and 4 (Rho=−0.376, P<.001) (Fig. 3D-F).
The statistical analysis also identified an inverse correlation between age and estimated smartphone use in both groups: Rho=−0.669 (P<.001) among patients and Rho=−0.587 (P<.001) among controls; the correlation was Rho=−0.613 (P<.001) for the sample as a whole.
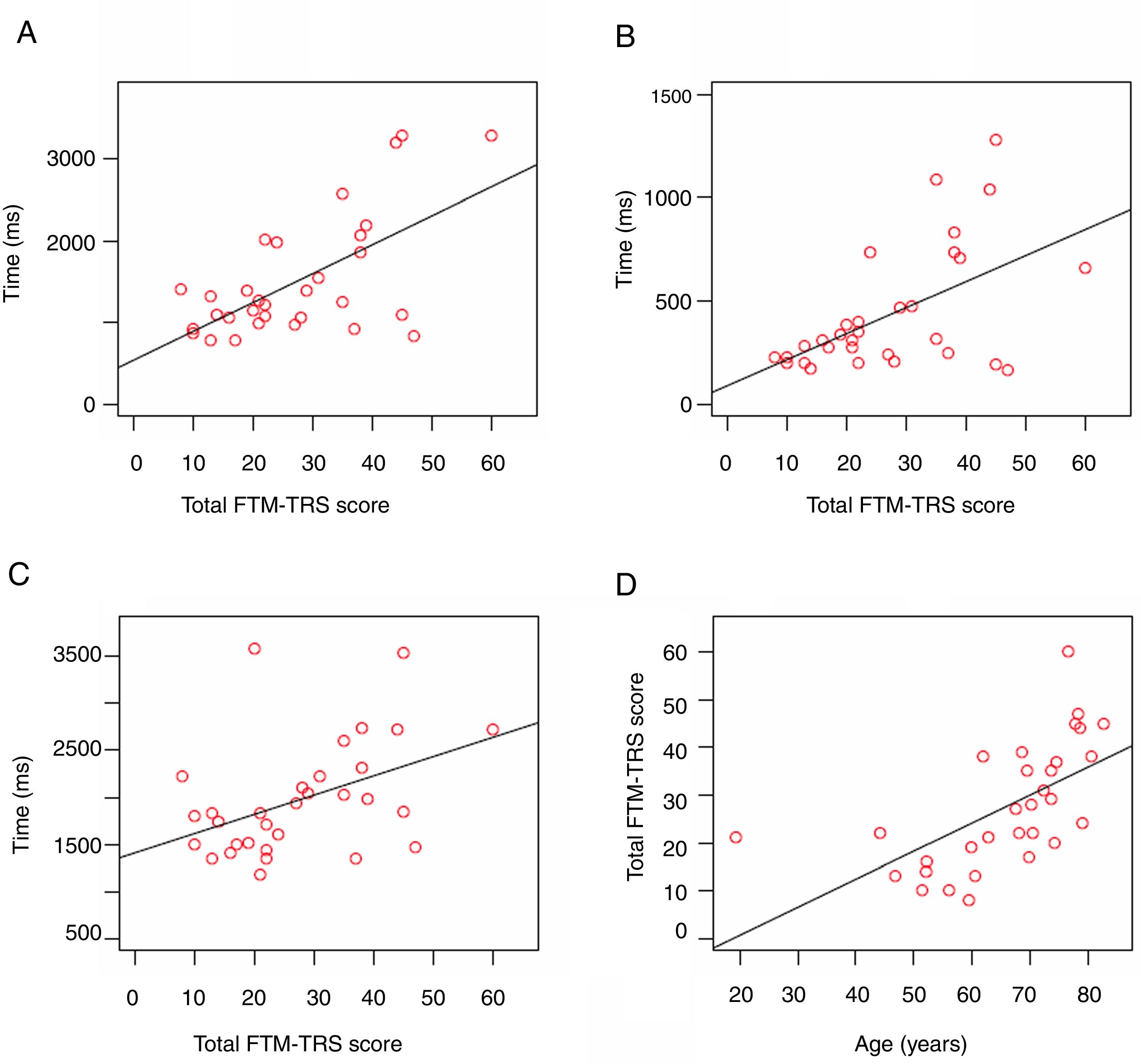
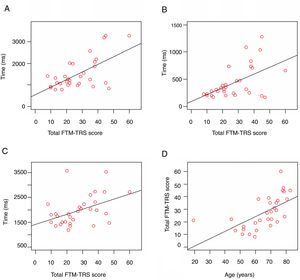
Among patients, tremor intensity (as measured with the FTM-TRS) showed a strong correlation with age (Rho=0.747, P<.001) and was directly correlated with the results of tasks 3A (Rho=0.484, P=.005), 3B (Rho=0.449, P=.011), and 4 (Rho=0.424, P=.017) (Fig. 4).
Regression analysis of tremor severity (Fahn-Tolosa-Marin Tremor Rating Scale) in patients with essential tremor. (A) Test 3A: time taken to switch off the alarm. (B) Test 3B: time between taps. (C) Test 4: time taken to switch off the alarm by dragging a circle across the screen. (D) Correlation between FTM-TRS score and age.
Our study shows similar types of smartphone use in patients with ET and controls, and no significant differences in performance of the most common types of touchscreen interaction. Therefore, ET was not associated with poorer performance in this interaction. However, several other factors do appear to influence basic interaction with touchscreens. Older age, less frequent smartphone use, and greater tremor intensity were associated with longer time taken for task performance.
This is the first study to compare interaction with touchscreens between patients with ET and healthy individuals using a descriptive approach. Previous studies have focused mainly on healthy users and those with other motor disorders.7,13 Some studies analysing interaction with touchscreen computers in patients with tremor report poor accuracy and propose various methods of assistance.17,18 These findings suggest that screen size probably plays an important role in the accuracy of these patients’ interaction with touchscreens.7
Our findings are consistent with those of other studies in the literature, which suggest that the introduction of new technology at older ages, cultural influences,1,19 and limited previous experience with technology in daily life20 influence the implementation of healthcare platforms based on smart devices. All these factors must be taken into account in the design of touchscreen-based patient care networks.
Our findings may therefore support the use of touchscreens in research into ET. However, as this is a pilot study, the absence of significant differences in our results does not rule out their existence. Future research is needed to better characterise touchscreen interaction in patients with ET.
Considerations regarding methodologyThis study is the first to describe the preferences of patients with ET regarding smartphone use and to study basic interaction with touchscreens through an application including tasks frequently used in smartphone user interfaces.
Our study also has several limitations. Firstly, patients with ET estimated their smartphone use at twice the level reported by controls, although this difference was not statistically significant. Therefore, these patients may be more accustomed to using these devices, which would result in an underestimation of the true difference between the 2 groups’ performance. This is a subjective, potentially biased measure; therefore, other means of quantifying daily mobile phone use may be helpful. “Tracker” applications may be useful in addressing this issue.21 Secondly, the time taken to perform tasks was related to age and to estimated smartphone use; however, the hypothesis that longer time taken implies poorer interaction is unconfirmed. Results may be influenced by devices’ technical specifications and settings (eg, screen size, brightness, touch sensitivity, contrast).7,22 The present study tested only one configuration and one screen size. Thirdly, participating patients had mild to moderate tremor. Although we identified no differences between these subgroups, it is possible that a difference may be observed if patients with more intense tremor were included. Finally, the simplicity of the tasks included in the application may conceal potential differences between groups.
ImplicationsThere is a need for additional studies including tasks of increasing difficulty, larger samples, and patients with more severe tremor. Comparison of different screen sizes, interfaces, or devices, and greater focus on age, level of smartphone use, and technical specifications would aid in determining whether patients with ET actually present differences in touchscreen interaction. Our focus on basic touchscreen interactions, combined with future developments, may inform the optimisation of user interfaces for patients with tremor.
ConclusionsNo significant differences were observed in smartphone use or touchscreen interaction between patients with ET and controls. However, several other factors do appear to influence basic interaction with touchscreens. Older age, less frequent smartphone use, and greater tremor intensity were associated with longer time taken for task performance.
Given the growing ubiquity of these devices, future studies should explore their usefulness in medicine.
Ethical considerationsOur study complies with the ethical standards of the Declaration of Helsinki. The study was approved by the bioethics committee of Hospital 12 de Octubre (Madrid, Spain). All participants agreed to be included in the study.
FundingThis study was funded by the Spanish Ministry of Economy and Competitiveness (grant no. RTC-2015-3967-1, “NetMD-Plataforma para el seguimiento de Trastornos del Movimiento”).
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors are grateful to Julia Gómez Vicente and Experis IT for their contribution to the development of the mobile application and to the statistician David Lora Pablos for revising and analysing the data.
Please cite this article as: López-Blanco R, Benito-León J, Llamas-Velasco S, Del Castillo MD, Serrano JI, Rocon E, et al. Interacción con pantalla táctil de smartphone en pacientes con temblor esencial y sujetos sanos. Neurología. 2021;36:657–665.