Levodopa continues to be the most effective pharmacological treatment for Parkinson’s disease (PD).1 In fact, diagnosis of PD is based on patient response to dopaminergic treatment; lack of response constitutes a warning sign for atypical parkinsonism.2 Furthermore, response to levodopa constitutes the best predictor of response to deep brain stimulation (DBS). Patients with high-quality “on” states present better and more sustained response to DBS.3
Some patients with PD are intolerant to levodopa, particularly in early stages of treatment. This is usually solved with slow, progressive dose adjustment and the use of peripherally-acting prokinetics, such as domperidone.
We present the cases of 3 women with PD treated with bilateral subthalamic DBS despite intolerance to dopaminergic treatment (different formulations of levodopa and oral or transdermal dopaminergic agonists) and such other antiparkinsonian drugs as rasagiline. Intolerance to the drug prevented us from performing the levodopa challenge test in all 3 cases. While patient 3 partially tolerated the apomorphine test, none of the patients tolerated treatment with continuous infusion of apomorphine.
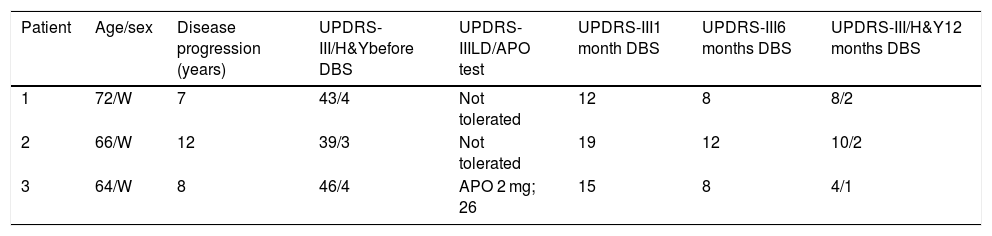
In all cases, DBS achieved marked improvements in parkinsonian symptoms, especially in patients 1 and 3, who also presented severe resting tremor in the limbs. Our patients’ clinical characteristics and progression data are summarised in Table 1. None of the patients presented any immediate complications of surgery or adverse reactions to DBS.
Patient characteristics and progression after deep brain stimulation.
| Patient | Age/sex | Disease progression (years) | UPDRS-III/H&Ybefore DBS | UPDRS-IIILD/APO test | UPDRS-III1 month DBS | UPDRS-III6 months DBS | UPDRS-III/H&Y12 months DBS |
|---|---|---|---|---|---|---|---|
| 1 | 72/W | 7 | 43/4 | Not tolerated | 12 | 8 | 8/2 |
| 2 | 66/W | 12 | 39/3 | Not tolerated | 19 | 12 | 10/2 |
| 3 | 64/W | 8 | 46/4 | APO 2 mg; 26 | 15 | 8 | 4/1 |
APO: apomorphine; DBS: deep brain stimulation; H&Y: Hoehn and Yahr scale; LD: levodopa; UPDRS: Unified Parkinson’s Disease Rating Scale; W: woman.
DBS was the only viable treatment option in our patients. Despite potential doubts arising due to the lack of response to dopaminergic treatment, diagnosis of PD was clear in all 3 patients. All 3 met the United Kingdom Parkinson’s Disease Society Brain Bank diagnostic criteria; according to the more recent criteria established by Postuma et al.,2 a diagnosis of clinically probable PD could be established in all cases. Presence of parkinsonian tremor and the lack of signs compatible with postsynaptic parkinsonism after several years of progression did not suggest any alternative diagnosis. During the initial stages of diagnosis, patients 2 and 3 underwent DaTSCAN studies, which revealed bilateral, asymmetric reduced tracer uptake. Strictly speaking, none of our patients was in an advanced stage of the disease since they did not present fluctuations or complications associated with treatment, nor did they present axial or cognitive symptoms, which may have represented a contraindication for DBS.
Lack of response to dopaminergic treatment is not only a warning sign but also an exclusion criterion for DBS.4 Furthermore, lack of response prevents us from predicting the clinical benefits of DBS, since the purpose of the treatment is to achieve the best and most stable pharmacological “on” state.
The interest of cases 1 and 2 lies in the fact that both patients underwent surgery for DBS despite never having shown response to dopaminergic agents, either as treatment or in a responsiveness test.5 Although lack of response constitutes a formal exclusion criterion, we should bear in mind that it represents intolerance to a particular medication, rather than lack of an actual response. We believe that DBS should not be ruled out in these patients without careful analysis of other relevant factors since this treatment is the only option that may achieve prolonged relief of their symptoms. In the case of patient 3, 4 years have passed since she underwent surgery for DBS electrode placement, and she continues to display an excellent response (UPDRS-III: 8; Hoehn and Yahr: 2).
Please cite this article as: Fernández-Pajarín G, Sesar A, Ares-Pensado B, Castro A. Intolerancia a la medicación dopaminérgica y estimulación cerebral profunda, a propósito de 3 casos. Neurología. 2020;35:664–665.