Paragangliomas are tumours formed by chromaffin cells from the neural crest. They are further classified as sympathetic paragangliomas, which usually secrete norepinephrine, and parasympathetic paragangliomas, which are usually nonfunctioning and are located in the head and neck.1 Most parasympathetic paragangliomas are benign, although they may cause symptoms due to compression of nearby nerves or blood vessels.2 We report the unusual case of a patient with a jugular paraganglioma clinically manifesting as Tapia syndrome.
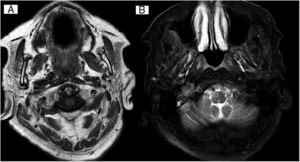
Our patient was an 80-year-old woman with history of dyslipidaemia, arterial hypertension, chronic obstructive pulmonary disease, chronic ischaemic heart disease, and motor and visual functional limitations. She was admitted to the internal medicine department due to pulmonary infiltrate in the right middle lobe, which was initially attributed to bronchoaspiration. The patient reported a 6-month history of subacute, progressive dysphonia and dysphagia for solids and liquids; symptoms were stable at the time of history taking. The physical examination revealed rightward tongue deviation and atrophy of the right side of the tongue (Fig. 1), compatible with paralysis of the right cranial nerve XII, as well as dysphagia for solids and hypophonia, with persistent gag reflex bilaterally, compatible with involvement of the laryngeal branch of cranial nerve X. Fibreoptic laryngoscopy revealed paralysis of the right vocal cord with adduction. A brain MRI study was performed due to suspicion of a structural lesion. The scan revealed a tumour in the right jugular foramen, located lateral to the internal jugular vein, anterior to the internal carotid artery, and posterior to the sigmoid sinus; all structures were patent. Signal was hypointense on T1-weighted sequences and heterogeneous on T2-weighted sequences, with tubular structures inside the tumour showing signal void (Fig. 2A and B). The scan also revealed signs of atrophy of the right side of the tongue, probably secondary to denervation, and glottic asymmetry, probably associated with paralysis of the right vocal cord. These radiological findings are suggestive of jugular paraganglioma. The patient had no family history of paraganglioma. No alterations were detected in urine and blood catecholamine levels. A chest and abdomen CT scan showed no relevant findings. The patient was unwilling to undergo surgery or radiation therapy. We therefore opted for conservative treatment, with rehabilitation therapy and close follow-up.
Head and neck paragangliomas are rare, accounting for 0.012% to 6% of all tumours appearing in these locations.3,4 Only 1%-3% of these tumours secrete catecholamines.1 They usually expand to areas of lower resistance, such as vascular spaces or foramina,2 and may cause jugular foramen syndromes, such as Vernet syndrome (involvement of cranial nerves IX, X, and XI) or Collet-Sicard syndrome (cranial nerves IX, X, XI, and XII). Metastasis is the main cause of jugular foramen tumours; paragangliomas are the type of primary tumour most frequently affecting this structure.5 In fact, simultaneous involvement of multiple lower cranial nerves may occur in up to 10% of paragangliomas.6 However, these usually involve the jugular foramen exclusively; in a review of 51 cases of Collet-Sicard syndrome, only 2 patients had jugular paragangliomas.7
In our patient, simultaneous involvement of the right cranial nerve XII and the laryngeal branch of the right cranial nerve X are suggestive of a jugular foramen syndrome known by the eponym Tapia syndrome; the condition was first described in 1904 by Spanish otorhinolaryngologist Antonio García Tapia.8 Most published cases of Tapia syndrome are caused by orotracheal intubation,9,10 although isolated cases of Tapia syndrome secondary to inflammatory pseudotumor have also been reported.11
As our patient had not undergone orotracheal intubation, the neurological examination led us to suspect involvement of the poststyloid space, where cranial nerves X and XII are anatomically connected.12 The radiological findings and the expansion of the lesion to nearby structures in our patient pointed to jugular paraganglioma.13–15 To our knowledge, this is the first reported case of simultaneous involvement of cranial nerves X and XII due to a paraganglioma.
In conclusion, presence of a tumour should be suspected in patients with neurological symptoms compatible with Tapia syndrome and no recent history of orotracheal intubation. Paragangliomas are the primary tumour most frequently affecting the jugular foramen. A radiological study should be performed to determine the structures affected, and catecholamine levels should be measured to determine whether the tumour is functional.
FundingNo funding was received for this study.
Please cite this article as: Sánchez-Soblechero A, Martín Gómez MÁ, Contreras Chicote A. Síndrome de Tapia como forma de presentación de paraganglioma yugular. Neurología. 2020;35:590–591.