The COVID-19 epidemic has led to the need for unprecedented decisions to be made to maintain the provision of neurological care. This article addresses operational decision-making during the epidemic.
DevelopmentWe report the measures taken, including the preparation of a functional reorganisation plan, strategies for hospitalisation and emergency management, the use of telephone consultations to maintain neurological care, provision of care at a unit outside the hospital for priority patients, decisions about complementary testing and periodic in-hospital treatments, and the use of a specific telephone service to prioritise patients with epileptic seizures.
ConclusionDespite the situation of confinement, neurology departments must continue to provide patient care through different means of operation. Like all elements of management, these must be evaluated.
La pandemia de Covid-19 ha supuesto la necesidad de tomar decisiones para mantener la asistencia neurológica, sin precedentes. En este artículo se analiza esa toma de decisiones operativas.
DesarrolloLos autores refieren las fórmulas empleadas como son la realización de un plan de reorganización funcional, estrategias para la hospitalización y urgencias, la realización de consultas telefónicas para el mantenimiento de la atención neurológica, la asistencia en un área externa al hospital para pacientes preferentes, las decisiones sobre exploraciones complementarias y tratamientos intrahospitalarios periódicos o implantar un teléfono para la priorización de crisis epilépticas.
ConclusiónA pesar de la situación de aislamiento, los servicios de neurología deben mantener la atención de sus pacientes a través de distintas fórmulas operativas, que como cualquier elemento de gestión, deberán evaluarse.
Throughout history, epidemics have given rise to demographic and social change. The bubonic plague brought about a different era in the Middle Ages: besides the deaths of many people, it slowed the rate of social progress. The new coronavirus, SARS-CoV-2, has changed our perception of the world in just a few weeks. While social isolation is a necessary objective, its repercussions have led to decisions that just weeks ago would have been unthinkable.1 Healthcare systems have been forced to respond rapidly to the new reality, making decisions for the benefit of their patients, but which are not exempt from indirect consequences.
One of the threats associated with the COVID-19 epidemic is what oncologists have referred to as the “distraction effect,” whereby the prioritisation of patients with SARS-CoV-2 infection has led to reductions in the care provided to patients with other diseases, especially due to the allocation of resources to this urgent problem, perceived as decisive. Therefore, the distraction effect may have negative repercussions for many patients, which we must endeavour to prevent.2 The prevalence of neurological symptoms appears to be low among patients with COVID-19, according to patient series,3–8 specific studies of hospitalised patients,9 and case reports,10 and the medium- and long-term effects on the central nervous system are not known.11–13 However, the epidemic may have negative consequences for other neurological patients if they do not receive specific care, as neurological diseases are the leading cause of disability worldwide. This article does not discuss the implementation or adaptation of diagnostic and/or treatment protocols for different neurological diseases, which have already been addressed by various neurology societies and expert groups. Rather, we describe the operational decisions made in response to the new situation, in line with the experience reported in other specialties14–16 and the proposals made after the analysis of similar situations.17
Confinement, which has been part of the strategy to reduce the spread of the disease, has impacted on the provision of medical care. This is particularly relevant for neurological patients, as many present such risk factors as older age and disability, which increase the likelihood of poorer prognosis in the event of infection. Furthermore, these patients are usually accompanied when they attend consultations; this has become very difficult during the pandemic, affecting the traditional methods of neurological care used in consultations. While telemedicine has become a necessity for healthcare team management and for maintaining the provision of neurological care while avoiding the transmission of SARS-CoV-2 between patients, their relatives, neurologists, nurses, and researchers,18–21 its implementation in patient care is challenging, despite the availability of the necessary resources. Telemedicine has previously been proposed as a response in the event of a disaster22,23; the issue is whether it can be applied for extended periods to serve large numbers of patients.
The situation of the pandemic gave rise to the need for adaptation of patients’ access to neurological care, such as stroke programmes and in-hospital and pre-hospital code stroke protocols, and to protect the personnel attending these patients24–26; it has also been necessary to make decisions regarding patients with stroke who also present SARS-CoV-2 infection, despite the existence of tele-stroke programmes prior to the pandemic. The response to emergency situations, the follow-up of patients with chronic but changing conditions, and the continuation of treatment provision have led to the use of tools that were previously employed only rarely, such as email and other electronic tools.27 The limitation of these technologies is that patients often do not use them due to older age or the characteristics of their disease. Photographs or video footage recorded by patients or their family members may enable neurologists to assess clinical changes remotely; for example, oculomotor alterations, gait, and balance may be assessed using video. All these methods have enabled neurology departments to maintain the provision of care and patient follow-up despite the circumstances.
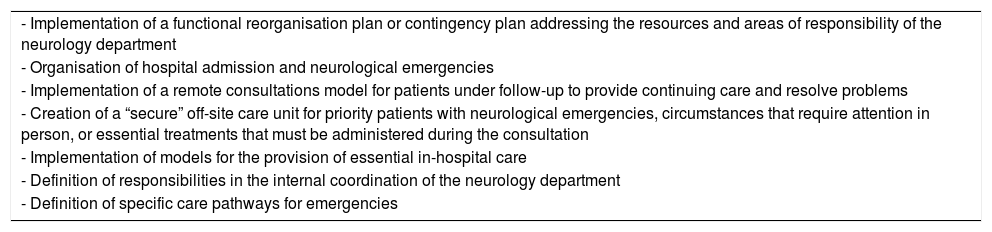
Operative decisionsOperative decisions must always be taken in accordance with the directives of hospital management, giving priority to infected patients. Nonetheless, departments are responsible for decisions regarding their own functioning; these are summarised in Table 1. The impact of the pandemic on hospitals requires functional reorganisation of departments, setting new objectives and reallocating resources and responsibilities; this process must involve the participation of members of the department to ensure they are aware of and take on specific duties. Furthermore, the impossibility of holding in-person departmental meetings has led to the implementation of new forms of coordination and liaison. The organisation of neurological emergencies and admissions is particularly challenging at a time when a high number of patients are infected with the virus. The initial aim of hospitalised patients being attended by teams of physicians that rotate each week could not be maintained because neurologists, admirably, wished to support the infectious diseases and internal medicine departments. Unfortunately, some colleagues also had to be quarantined. Nonetheless, the model of rotating care teams for potentially exposed patients seems to be a reasonable approach. One basic action is to maintain the continuity of care, albeit remotely, ideally through the use of telephone consultations28 and electronic resources.29,30 This necessity arises from the role of social isolation in reducing the spread of the disease, which has affected medical care; however, the rapid propagation of the virus has turned healthcare facilities and transport31 into potential sources of infection. Therefore, it has become essential to centre care around telephone consultations, which have represented the central element of neurological care. These calls are technical and must be informative both for the patient and for the physician, who must make clinical decisions based on limited information. Due to the situation of confinement, it is nearly always possible to speak with patients immediately, and follow-up consultations are often held much more regularly than before the pandemic. Patients report high satisfaction and perceive this highly personalised care as having a positive impact on their health. Neurologists will also be aware if one of their patients is infected with the virus and will be able to contribute to decisions about the patient, whose underlying neurological condition may affect prognosis. If patients present new symptoms or progression of the neurological disease, neurologists will make the appropriate decision in each case, analysing the risk/benefit balance of the patient visiting hospital, which should be avoided where possible. Remote follow-up involves making decisions about whether to perform or postpone routine complementary studies requiring a hospital visit, which must be assessed individually. Neurologists must also consider whether in-hospital treatments should be postponed; again, these decisions should be considered on an individual basis and account for the impact of delaying or suspending treatment on the progression of the disease and possible rebound or withdrawal effects.
Operative decisions regarding neurological care provision during the COVID-19 pandemic.
| - Implementation of a functional reorganisation plan or contingency plan addressing the resources and areas of responsibility of the neurology department |
| - Organisation of hospital admission and neurological emergencies |
| - Implementation of a remote consultations model for patients under follow-up to provide continuing care and resolve problems |
| - Creation of a “secure” off-site care unit for priority patients with neurological emergencies, circumstances that require attention in person, or essential treatments that must be administered during the consultation |
| - Implementation of models for the provision of essential in-hospital care |
| - Definition of responsibilities in the internal coordination of the neurology department |
| - Definition of specific care pathways for emergencies |
One important initiative was the creation of a “secure” off-site care unit for the treatment of priority patients with neurological emergencies or other circumstances requiring care to be given in person, and for the continued administration of treatments that cannot be postponed. This secure care unit also enables the resolution of situations in which telephone consultation is insufficient, guaranteeing that neurologists may assess patients in person. At the secure unit, we have been able to directly schedule patient appointments for essential treatments (eg, for exacerbation of myasthenia gravis symptoms or multiple sclerosis relapses) at the day hospital, perform neurophysiological or imaging studies after telephone consultations, and follow up patients requesting consultation after a recent hospital discharge.
Neurology remains a clinical specialty, and it is unthinkable that any patient should be dismissed without direct examination, even if special precautions must be taken. These scheduled patients must attend the centre alone; caregivers should not accompany them except in cases where this is demonstrably necessary for the patient's continued care. It is important to take into account the need for physical separation of physician and patient; that patients should attend consultations alone where possible; that eye fundus examination should be avoided wherever possible in order to minimise physical proximity between patient and physician; that lumbar puncture should only be performed when essential; and that the clinical examination should target the symptoms motivating consultation, aiming to minimise the duration of the consultation.
Despite these considerations, some patients require complex treatments or essential diagnostic tests, making hospital visits unavoidable. In these cases, new, personalised forms of consultation are needed. Patients’ temperature should be taken prior to consultation, and individuals presenting fever should be seen unaccompanied and all safety protocols observed. The decision involves weighing the risk of transmission of the virus against the potential benefit of the scheduled treatment or examination. We must also seek ways of following up patients in specific circumstances and enabling direct access to the neurology department. For example, epileptic seizures represent a challenge when patients are in isolation. In addition to continuing follow-up of seizures and treatment, we have enhanced the care provided in the event of an emergency or potential emergency in order to optimise treatment outside the hospital. Patients are generally given action plans to follow in the event of unusual seizures and have rescue medications, which may be administered by their family. We have also strengthened these protocols, adding rescue medications that are easily administered at home (oral benzodiazepines and other antiepileptic drugs prepared in solution). We also provided telephone numbers for emergency consultations to minimise trips to hospital, and used telephone consultations to follow up all patients assessed in the emergency department due to new epilepsy starting during the pandemic, adjusting treatment and scheduling essential complementary tests.
Finally, it is evident that the structure of on-call neurology services is an important element in patient care. Neurology departments should maintain care provision for patients under follow-up, and this is only possible with information, proximity, coordination with admitting departments, and capacity to respond to new circumstances. Like all operative decisions in clinical management, those made during the pandemic must be subject to evaluation.
Please cite this article as: Matías-Guiu J, Porta-Etessam J, Lopez-Valdes E, Garcia-Morales I, Guerrero-Solá A, Matias-Guiu JA. La gestión de la asistencia neurológica en tiempos de la pandemia de Covid-19. Neurología. 2020;35:233–237.