The COVID-19 pandemic will give rise to long-term changes in neurological care, which are not easily predictable.
Material and methodsA key informant survey was used to enquire about the changes expected in the specialty over the next 5 years. The survey was completed by heads of neurology departments with broad knowledge of the situation, having been active during the pandemic.
ResultsDespite a low level of consensus between participants, there was strong (85%) and moderate consensus (70%) about certain subjects, mainly the increase in precautions to be taken, the use of telemedicine and teleconsultations, the reduction of care provided in in-person consultations to avoid the presence of large numbers of people in waiting rooms, the development of remote training solutions, and the changes in monitoring visits during clinical trials. There was consensus that there would be no changes to the indication of complementary testing or neurological examination.
ConclusionThe key informant survey identified the foreseeable changes in neurological care after the pandemic.
La pandemia de COVID-19 va a conllevar cambios en la asistencia neurológica, que no se pueden prever fácilmente a largo plazo.
Material y métodosA través de un modelo de informadores clave se busca el consenso de cómo va a ser la especialidad en un plazo de 5 años, siendo los encuestados jefes de servicio de neurología con conocimiento amplio de la situación al haber actuado durante la pandemia.
ResultadosAunque se obtiene un grado de acuerdo bajo entre los encuestados, sí se describen acuerdos por consenso a nivel mayor (85%) y menor (70%). Los principales acuerdos se refieren al incremento de precauciones, al uso de la telemedicina, al mantenimiento de las consultas telefónicas, a la reducción de asistencia a las consultas evitando que hayan salas de espera con un número alto de personas, al desarrollo de técnicas docentes no presenciales y a la adaptación en el desarrollo de ensayos clínicos en relación con la visita de los monitores. Sin embargo, no se acuerda que haya cambios en la indicación de exploraciones complementarias, ni en la propia exploración neurológica.
ConclusiónEl método de informadores clave ha permitido conocer qué cambios se pueden prever tras la pandemia.
In a matter of weeks, the COVID-19 epidemic has significantly changed the capacity to provide healthcare. Confinement measures1 and the frequent saturation of hospitals in Spain are giving rise to a new scenario in healthcare, and neurology departments are no exception.2 While early patient series report low prevalence of neurological symptoms among patients with COVID-19,3–9 reports of patients with neurological manifestations are becoming more frequent10–12 and it has been suggested that the infection may have medium- or long-term effects on the central nervous system13–17 and influence the course of other neurological diseases.18 One threat associated with the pandemic is what some oncologists have referred to as the “distraction effect,”19 whereby the prioritisation of patients with COVID-19 has led to a decrease or absence of care provision for other patients, particularly given the allocation of resources to an urgent problem that is perceived to be decisive. Neurological patients are not exempt from this situation. While it is difficult to foresee future events, this study aims to predict the changes in neurological care provision after the pandemic through a key informant survey.20
Material and methodsThe key informants consulted in this study are 14 heads of neurology departments from different Spanish autonomous communities, who have held these positions for at least 3 years and have managed their departments during the pandemic. The survey (Supplementary material 1) comprised 132 items divided into 10 sections addressing respondents’ opinions about the consequences of the pandemic for neurology as a specialty; care activity and clinical practice; the performance of complementary tests; precautions to be taken; the organisation of neurology departments; new resources needed after the pandemic; neurological nursing care and the role of nurse case managers in patient care; stroke care; training; and research. Respondents were asked to score their level of agreement with each statement from 1 (strongly disagree) to 5 (strongly agree). Each section also included an open-ended question, inviting the experts consulted to provide any other observations. Four redundant statements were included for quality control purposes. The survey was distributed to the respondents on 10 April 2020 and returned before 12 April 2020. According to official sources, there were 152446 confirmed cases of COVID-19 in Spain on 9 April, with incidence rates varying between autonomous communities. Data were analysed with the SPSS statistics package (version 20), and agreement scores (from 1 to 5) are presented as means with standard deviations. We also established a qualitative classification of results, as follows: (1) strong consensus, for statements for which one of 2 consecutive scores was given by at least 85% of respondents (12 experts) and (2) moderate consensus, when one of 2 consecutive scores was given by at least 71% of respondents (10 experts). For those statements for which not all experts gave a response, the thresholds were set at 84.6% (11 responses) for strong consensus and 69% (9 responses) for moderate consensus. We also analysed the degree of consensus between informants for the survey as a whole and for each section, using the “rel” package in the RStudio software (version 1.2.5033-1).
ResultsThe analysis of the degree of consensus is shown in Supplementary material 2. Supplementary material 3 shows mean scores and standard deviations. Tables 1–4 show the conclusions drawn from statements for which there was strong or moderate consensus. Despite consensus about these statements, the degree of inter-rater agreement was low. Responses to the open-ended questions generally gave more detailed information on the consensus.
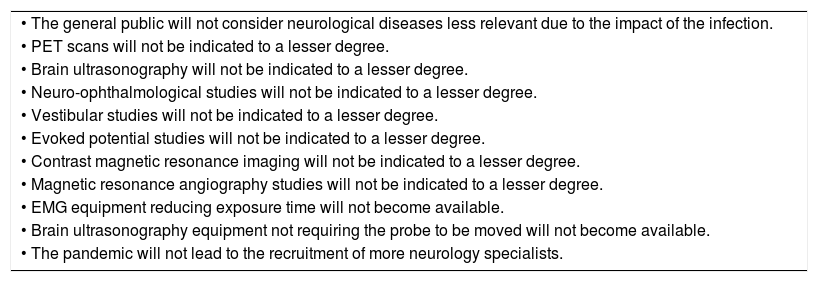
Conclusions drawn from moderate consensus (disagreement with survey items, > 71%).
| • The general public will not consider neurological diseases less relevant due to the impact of the infection. |
| • PET scans will not be indicated to a lesser degree. |
| • Brain ultrasonography will not be indicated to a lesser degree. |
| • Neuro-ophthalmological studies will not be indicated to a lesser degree. |
| • Vestibular studies will not be indicated to a lesser degree. |
| • Evoked potential studies will not be indicated to a lesser degree. |
| • Contrast magnetic resonance imaging will not be indicated to a lesser degree. |
| • Magnetic resonance angiography studies will not be indicated to a lesser degree. |
| • EMG equipment reducing exposure time will not become available. |
| • Brain ultrasonography equipment not requiring the probe to be moved will not become available. |
| • The pandemic will not lead to the recruitment of more neurology specialists. |
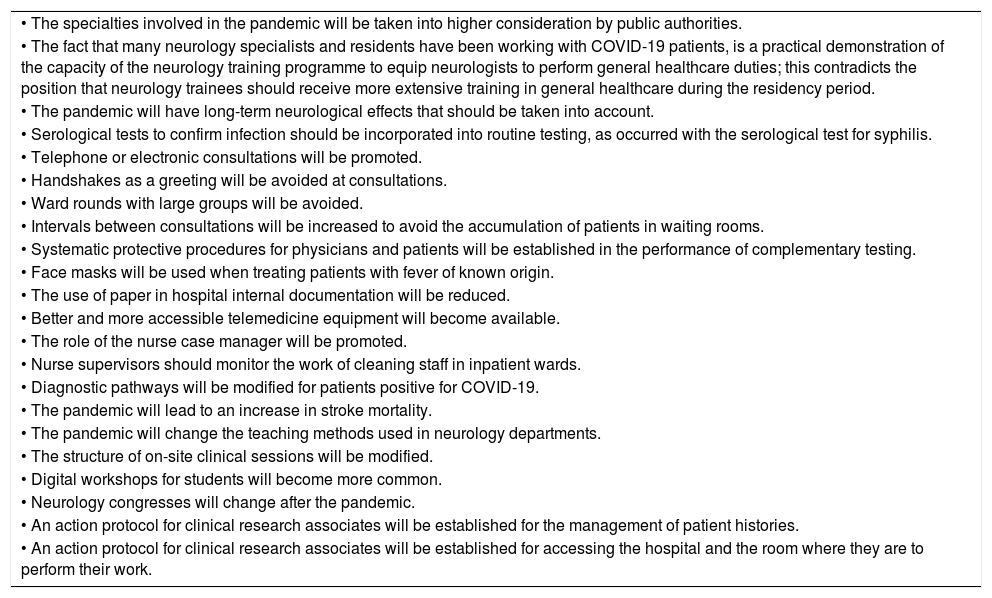
Conclusions drawn from moderate consensus (agreement with survey items, > 71%).
| • The specialties involved in the pandemic will be taken into higher consideration by public authorities. |
| • The fact that many neurology specialists and residents have been working with COVID-19 patients, is a practical demonstration of the capacity of the neurology training programme to equip neurologists to perform general healthcare duties; this contradicts the position that neurology trainees should receive more extensive training in general healthcare during the residency period. |
| • The pandemic will have long-term neurological effects that should be taken into account. |
| • Serological tests to confirm infection should be incorporated into routine testing, as occurred with the serological test for syphilis. |
| • Telephone or electronic consultations will be promoted. |
| • Handshakes as a greeting will be avoided at consultations. |
| • Ward rounds with large groups will be avoided. |
| • Intervals between consultations will be increased to avoid the accumulation of patients in waiting rooms. |
| • Systematic protective procedures for physicians and patients will be established in the performance of complementary testing. |
| • Face masks will be used when treating patients with fever of known origin. |
| • The use of paper in hospital internal documentation will be reduced. |
| • Better and more accessible telemedicine equipment will become available. |
| • The role of the nurse case manager will be promoted. |
| • Nurse supervisors should monitor the work of cleaning staff in inpatient wards. |
| • Diagnostic pathways will be modified for patients positive for COVID-19. |
| • The pandemic will lead to an increase in stroke mortality. |
| • The pandemic will change the teaching methods used in neurology departments. |
| • The structure of on-site clinical sessions will be modified. |
| • Digital workshops for students will become more common. |
| • Neurology congresses will change after the pandemic. |
| • An action protocol for clinical research associates will be established for the management of patient histories. |
| • An action protocol for clinical research associates will be established for accessing the hospital and the room where they are to perform their work. |
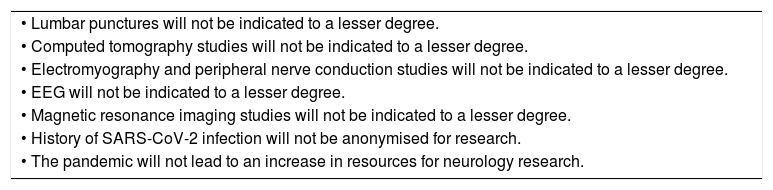
Conclusions drawn from strong consensus (disagreement with survey items, > 85%).
| • Lumbar punctures will not be indicated to a lesser degree. |
| • Computed tomography studies will not be indicated to a lesser degree. |
| • Electromyography and peripheral nerve conduction studies will not be indicated to a lesser degree. |
| • EEG will not be indicated to a lesser degree. |
| • Magnetic resonance imaging studies will not be indicated to a lesser degree. |
| • History of SARS-CoV-2 infection will not be anonymised for research. |
| • The pandemic will not lead to an increase in resources for neurology research. |
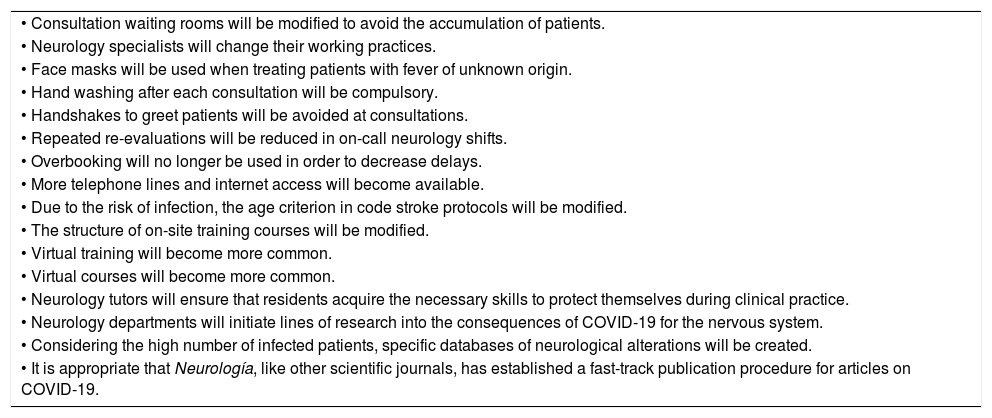
Conclusions drawn from strong consensus (agreement with survey items, > 85%).
| • Consultation waiting rooms will be modified to avoid the accumulation of patients. |
| • Neurology specialists will change their working practices. |
| • Face masks will be used when treating patients with fever of unknown origin. |
| • Hand washing after each consultation will be compulsory. |
| • Handshakes to greet patients will be avoided at consultations. |
| • Repeated re-evaluations will be reduced in on-call neurology shifts. |
| • Overbooking will no longer be used in order to decrease delays. |
| • More telephone lines and internet access will become available. |
| • Due to the risk of infection, the age criterion in code stroke protocols will be modified. |
| • The structure of on-site training courses will be modified. |
| • Virtual training will become more common. |
| • Virtual courses will become more common. |
| • Neurology tutors will ensure that residents acquire the necessary skills to protect themselves during clinical practice. |
| • Neurology departments will initiate lines of research into the consequences of COVID-19 for the nervous system. |
| • Considering the high number of infected patients, specific databases of neurological alterations will be created. |
| • It is appropriate that Neurología, like other scientific journals, has established a fast-track publication procedure for articles on COVID-19. |
This study analysed the opinions of heads of neurology departments on the changes in care provision, training, and research that they thought would be necessary in the coming years as a result of the pandemic, and their opinions on the image of the specialty. While neurologists from other countries have published their opinions in blogs or through the publications of professional associations,21,22 ours is the first study to use a key informant consensus approach to this end. The participants noted in their responses to the survey that their opinions were subject to change due to unknown factors, such as the duration of the pandemic, the potential appearance of a neurological syndrome secondary to COVID-19, or whether the disease would remain latent in the community. The consensus model used is also potentially biased by the fact that consensus is not reached by bringing together different positions, as occurs in the Delphi model; rather, we analysed the responses given and searched for points on which there was consensus. The study found a low degree of consensus, probably because responses depended on the impact of the pandemic, which varies by region. However, we did identify consensus on the statements listed in the tables.
Generally, the respondents foresaw few changes in the medium term, and believed that changes will mainly affect prevention measures and the movement of people, with efforts to reduce the numbers of people in waiting rooms, training sessions, and ward rounds. The majority of respondents agreed that the pandemic will lead to greater use of telemedicine1,23–26 and electronic learning solutions. There was also consensus that patient management times should be reorganised and that new methods will be needed to prevent overcrowding of patients and particularly neurological patients, who are especially vulnerable. The respondents predicted increased use of teleconsultation, which has been widely reported during the pandemic.27,28 However, they did not expect to see changes in clinical examinations or in indications for complementary testing, at least for neurologists. The key informants also did not predict changes in stroke care, although specific pathways may be established for patients testing positive for SARS-CoV-2.29,30 The respondents also suggested that the pandemic would lead to new ways of organising medical conferences and monitoring visits in clinical trials, and the progressive implementation of electronic media instead of paper.
One reason for the low level of consensus may be the difficulty of foreseeing medium-term changes in neurology departments in the context of the de-escalation of confinement measures. There was greater consensus on statements about events that have already happened or are currently underway. Of the changes that have already occurred, some are likely to remain in place, while others will progressively be reverted, depending on the time taken to control the pandemic and the potential for new outbreaks. In any case, despite the negative consequences of the pandemic, the “expectation for change” represents an opportunity to implement changes and improvements in healthcare systems in general, and in neurological care in particular. Such changes may include the generalisation of electronic medical records and the promotion of remote medical care, which in future may provide a foundation for the provision of healthcare to patients with chronic diseases. Similarly, the pandemic has brought to light the need to prioritise important elements of neurological care.
Evidently, the ways in which the necessary changes will be implemented will become apparent with time, particularly given the potential for COVID-19 to affect the progression of neurodegenerative diseases in the long term.31 However, there can be no doubt that the pandemic will increase societal awareness of the great value of healthcare systems in modern states and the responsibility of governments to protect and guarantee these services.
Authors’ contributionsLead investigators: JMG, EDT; study design: JMG, JAMG, EDT; questionnaire design: JMG, JAMG, EDT; questionnaire respondents: JMG, JAS, JRA, JA, ICN, MC, MDJH, JMLA, EM, AM, ARA, TS, PSC, EDT; database: JAMG; data analysis: JAMG; analysis of results: JMG, JAMG, EDT; critical discussion of results: JMG, EDT; drafting of manuscript: JMG, JAMG, EDT; review of manuscript: JMG, JAMG, JAS, JRA, JA, ICN, MC, MDJH, JMLA, EM, AM, ARA, TS, PSC, EDT.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Matías-Guiu J, Matias-Guiu JA, Alvarez-Sabin J, Ramon Ara J, Arenillas J, Casado-Naranjo I, et al. ¿Va a cambiar la neurología tras la pandemia de COVID-19 en los próximos 5 años? Estudio de enfoque mediante informadores clave. Neurología. 2020;35:252–257.