Palliative care in neurodegenerative diseases is useful but underused. The objective of this study is to know how palliative care (PC) is applied in Spain in order to identify limitations and unmet needs.
Materials and MethodsIt is a descriptive, observational, cross-sectional study, anonymous survey type of 20 questions, directed and answered by neurologists dedicated to movement disorders (MD) in Spain.
Results58 responses were obtained from neurologists from 15 autonomous communities. 69% answered that they did not have a specialised MD nursing facility but did have a PC team in their centre (81%). No specific protocol for PC in MD was identified. All except one neurologist stated that they lacked sufficient training in PC, the main training need being the “advance directives explanation”. Only 1 in 4 neurologists answered routinely explaining advance healthcare planning to their patients, recognising up to 84.5% of neurologists not knowing how to assess the patient's competence. 60.3% of those surveyed answered that between 10% and 30% of their patients would be candidates for PC, although 1 in 3 said they were not clear when to refer the patient to PC. 100% of neurologists affirmed the priority need to implement PC protocols in MD.
ConclusionsOur study shows a formative deficit in PC in this area and in the care of the patient with movement disorders and their environment, and should serve as a starting point to develop consensual care protocols.
La atención paliativa en enfermedades neurodegenerativas es útil pero infrautilizada. El objetivo de este estudio es conocer cómo se aplican en nuestro país los cuidados paliativos (CP) en los pacientes con trastornos del movimiento (TM) de cara a identificar posibles limitaciones y necesidades no cubiertas.
Material y métodosSe trata de un estudio descriptivo, observacional, transversal, tipo encuesta anónima de 20 preguntas, dirigida y contestada por neurólogos dedicados a los TM en España.
ResultadosSe obtuvieron 58 respuestas de neurólogos de 15 comunidades autónomas. El 69% contestó no disponer de enfermería especializada en TM pero sí de equipo de CP en su centro (81%). No se identificó ningún protocolo específico para CP en TM. Todos salvo un neurólogo afirmaron carecer de formación suficiente en CP, siendo la principal necesidad formativa la “explicación de voluntades anticipadas”. Sólo 1 de cada 4 neurólogos contestó explicar rutinariamente la planificación anticipada de la asistencia sanitaria a sus pacientes, reconociendo hasta el 84.5% de los neurólogos desconocer cómo evaluar la competencia del paciente. El 60.3% de los encuestados respondió que entre el 10% y 30% de sus pacientes serían candidatos a CP, aunque 1 de cada 3 afirmó no tener claro en qué momento derivar al paciente a CP. El 100% de los neurólogos afirmó la necesidad prioritaria de implementar protocolos de CP en TM.
ConclusionesNuestro estudio evidencia un déficit formativo en CP en TM y en la asistencia al paciente con TM y su entorno, debiéndonos servir como punto de partida para elaborar protocolos de atención consensuados.
Parkinson’s disease (PD) is the second most frequent neurodegenerative disease after Alzheimer disease. In Western countries, the prevalence rate of PD is 1% in the population over 60 years of age, and 3% in those aged 80 years or older1; incidence ranges from 9 to 22 cases per 100000 person-years.2 In Spain, around 300000 people have PD,3 although this figure is expected to increase in the coming years due to increased life expectancy. Despite the great variability in functional outcomes, the vast majority of patients will present some degree of disability, including cognitive impairment and a wide range of non-motor symptoms, which are difficult to control. The complexity of treatment for PD and other degenerative diseases causing movement disorders is compounded by the lack of specific training and experience of healthcare professionals providing palliative care (PC).
Although we typically associate PC with cancer, the needs of patients with neurodegenerative diseases and their families are similar to those of oncological patients. In both cases, the disease presents with symptoms that cause suffering for patients and their families, and which can be relieved. The World Health Organization defines PC as an approach that improves quality of life for patients and families facing the problems associated with life-threatening diseases. This approach focuses on the prevention and relief of suffering using early identification and strict evaluation and treatment of pain and other physical, psychosocial, and spiritual problems.4
In Europe, a set of common values is acknowledged among PC experts, including the value of patient autonomy and dignity, the need for individual planning and decision-making, and the holistic approach.5 Respecting patient autonomy implies proactively listening to their wishes, values, and expectations throughout the course of the disease. This is known as advance care planning, defined as a structured process that enables reflection and understanding of the experience of disease and the associated care among the persons involved, with a focus on the patient, who should be able to identify and express their preferences and expectations about the management of their disease.6 In Spain, advance directives are legal documents drafted by patients, which vary depending on the autonomous community where the patient lives.
The right to equitable access to PC is recognised by the United Nations; therefore, administrations should promote and allocate material and human resources to healthcare centres in order to implement these therapies.6 In 2019, the European Association for Palliative Care published an atlas of the situation of PC in Europe.7 This document showed that Spain is lagging in terms of number of PC services per capita; this undoubtedly represents a great opportunity for improvement for the healthcare professionals and institutions involved.
Given the lack of a curative treatment for movement disorders and the loss of quality of life associated with these diseases, PC should be an integral part of their management. In recent years, it has become increasingly apparent that PC must play an essential role in the management of patients with chronic, non-cancer disorders, with amyotrophic lateral sclerosis representing the paradigm of a neurological disease requiring PC by a multidisciplinary team. This approach has proved to be beneficial not only to patients and their families, but also to the healthcare system, with lower rates of hospital admissions.8,9 In Spain, however, PC for other neurodegenerative diseases, including movement disorders, is lacking. Several studies have underscored the severity of advanced PD and the need to implement PC strategies for these patients, which may be highly beneficial.10–12 A recent clinical trial conducted in the United States, including 225 patients and their caregivers, found that PC in patients with advanced PD achieved greater improvements in patient quality of life and symptoms than conventional treatment.13 This underscores the need to analyse the provision of PC to patients with movement disorders in Spain, aiming to identify areas for improvement.
ObjectiveThe aim of this study was to understand the structure of PC for movement disorders in Spain. More specifically, we aimed to identify the limitations and needs of PC, in terms of both resources and the training of healthcare professionals attending these patients.
Our conclusions will subsequently be used to develop an action protocol for PC in patients with movement disorders, aiming to improve care provision and quality of life among patients and their families.
Material and methodsWe conducted a descriptive, observational, cross-sectional study based on an anonymous survey of neurologists attending patients with movement disorders in Spain.
The project was developed by the Spanish Society of Neurology’s movement disorders study group (GETM, for its Spanish initials). We created a working group of 6 neurologists with an interest in PC from different Spanish autonomous communities, a nurse specialising in movement disorders, and a PC specialist. A meeting was held by videoconference on January 2021, where the working group agreed to perform the following actions: 1) a review of the literature on PC for movement disorders; 2) a survey of neurologists attending patients with movement disorders in Spain, enquiring about the application of PC in their practice; and 3) drafting of a consensus statement on PC of movement disorders in Spain, based on survey responses. The working group also decided to publish at least 2 studies; the first should report the results of the survey and the second would present the consensus statement and a set of recommendations.
The survey was created using Google Forms, and included 20 questions, in 4 sections: 1) care activity and type of healthcare centre of the respondent, 2) PC resources available at the centre, 3) training in PC, and 4) management of PC. The survey was e-mailed to all members of the GETM on 3 occasions between February and March 2021. Participation was voluntary and anonymous. The survey took approximately 5minutes to complete. Although data were anonymised, we considered the possibility of contacting certain centres after the survey was conducted, depending on the responses received, to request further information from movement disorders experts working at those centres.
Protocol approval and informed consentThe study did not require approval by the research ethics committee as no patient data were gathered and surveys were completed anonymously.
Data availabilityThe data gathered and analysed are available from the authors on reasonable request.
Data analysisData were analysed using the R software package, version 4.0.3. Quantitative variables are expressed as mean or median, depending on whether data were normally distributed, whereas qualitative variables are expressed as frequencies and percentages. Differences between variables were analysed with the t test, Mann-Whitney U test, chi-square test, or Fisher exact test, as appropriate. The threshold for statistical significance was set at P<.05.
ResultsThe survey was e-mailed to a total of 291 neurologists from the GETM. The e-mail was opened by 182 (62.5%), and the survey was completed by 58 neurologists (31.9%). Responses were submitted between 11 February and 15 March 2021. All responses were considered valid for analysis.
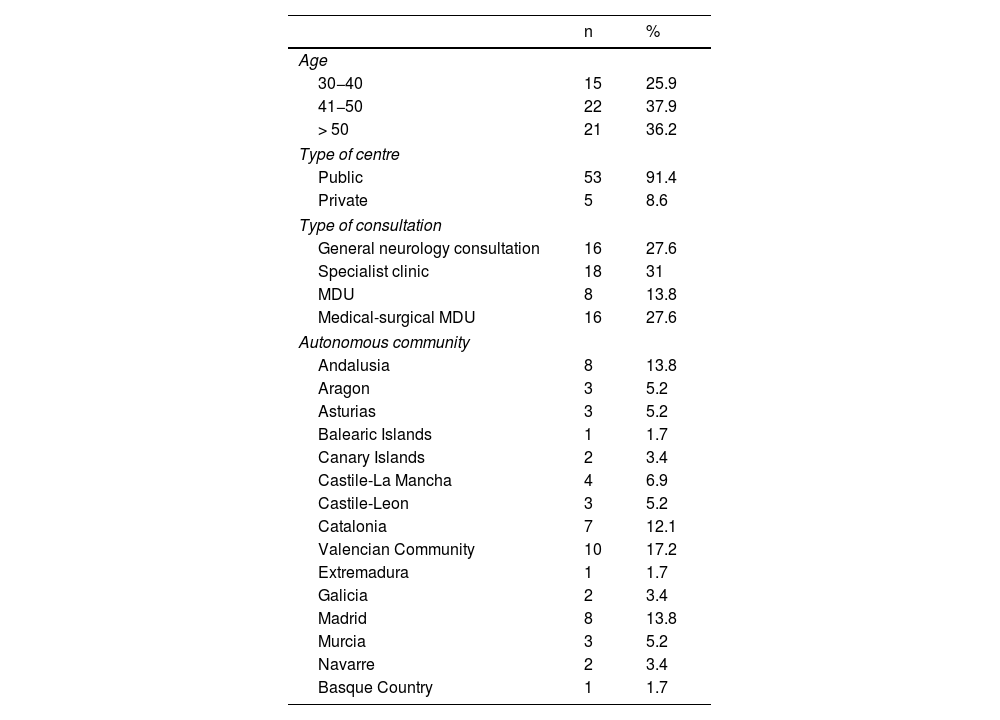
By age group, 25.9% of survey respondents were 30−40 years old, 37.9% were 41−50 years old, and 36.2% were older than 50 years. A total of 41.4% respondents worked at movement disorders units (MDU), which in most cases were located in public hospitals (91.4%) (Table 1). Responses were submitted by neurologists from 15 autonomous communities, with most neurologists working in the Valencian Community (17.2%), Madrid (13.8%), Andalusia (13.8%), and Catalonia (12.1%). By province, the greatest numbers of survey responses correspond to Madrid (13.8%), Barcelona (12.1%), Alicante (10.3%), Seville (6.9%), and Valencia (6.9%). Three responses were received from one hospital, and 2 responses each from another 5 centres.
Characteristics of the neurologists completing the survey.
| n | % | |
|---|---|---|
| Age | ||
| 30−40 | 15 | 25.9 |
| 41−50 | 22 | 37.9 |
| > 50 | 21 | 36.2 |
| Type of centre | ||
| Public | 53 | 91.4 |
| Private | 5 | 8.6 |
| Type of consultation | ||
| General neurology consultation | 16 | 27.6 |
| Specialist clinic | 18 | 31 |
| MDU | 8 | 13.8 |
| Medical-surgical MDU | 16 | 27.6 |
| Autonomous community | ||
| Andalusia | 8 | 13.8 |
| Aragon | 3 | 5.2 |
| Asturias | 3 | 5.2 |
| Balearic Islands | 1 | 1.7 |
| Canary Islands | 2 | 3.4 |
| Castile-La Mancha | 4 | 6.9 |
| Castile-Leon | 3 | 5.2 |
| Catalonia | 7 | 12.1 |
| Valencian Community | 10 | 17.2 |
| Extremadura | 1 | 1.7 |
| Galicia | 2 | 3.4 |
| Madrid | 8 | 13.8 |
| Murcia | 3 | 5.2 |
| Navarre | 2 | 3.4 |
| Basque Country | 1 | 1.7 |
MDU: movement disorders unit.
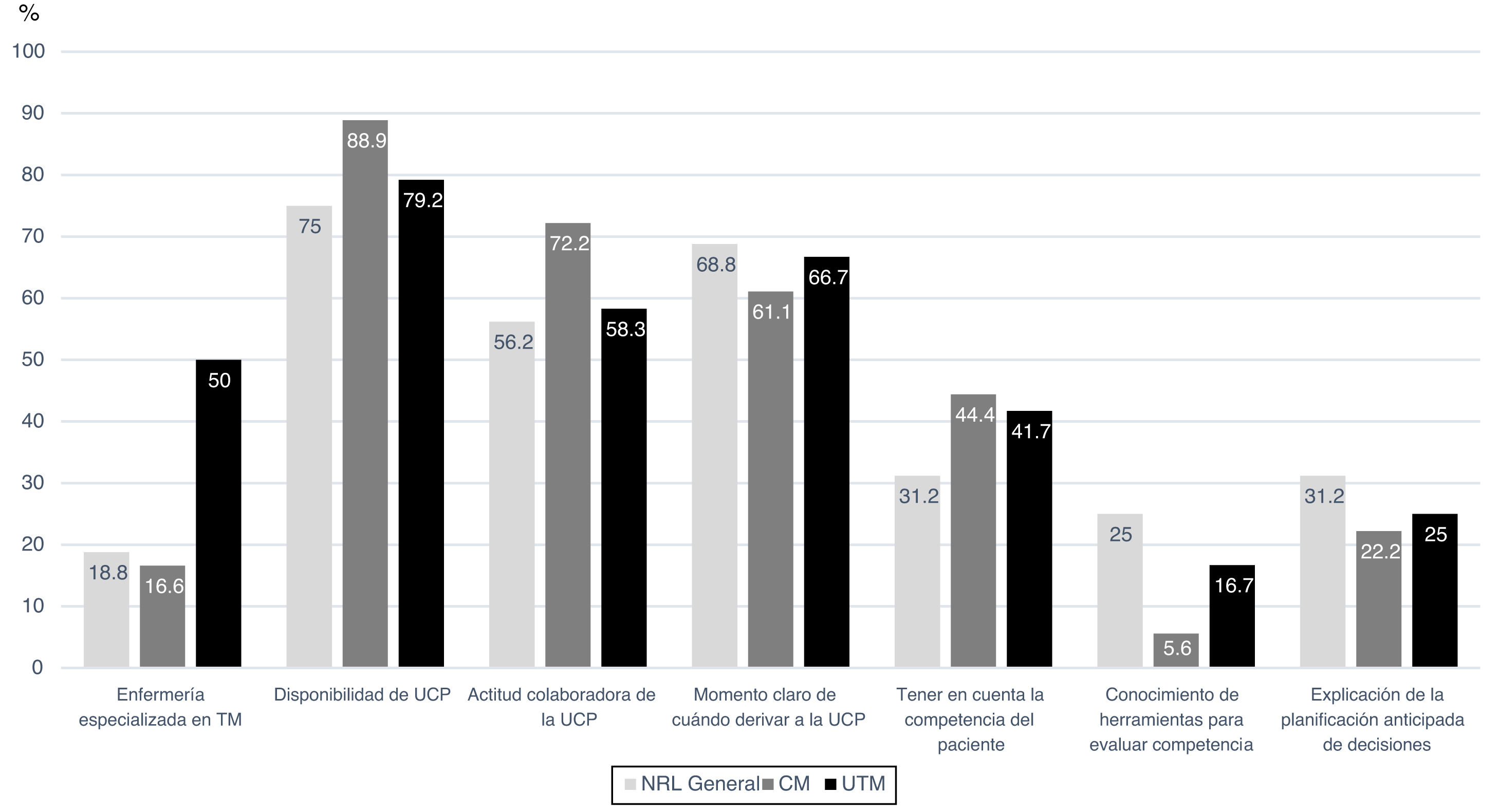
The majority of respondents (69%) reported that their centres did not have nurses specialising in movement disorders, but 81% did report an inpatient and/or outpatient PC unit or team, and 62.1% reported that PC specialists at their centres were open and willing to collaborate in the treatment and follow-up of patients with movement disorders and other neurodegenerative diseases. However, respondents at only 5 hospitals reported that a specific PC protocol was available for patients with neurodegenerative diseases other than ALS. By type of consultation (general neurology, specialist clinic, and MDU), 50% of MDUs had nursing staff specialised in movement disorders, compared to 16.7% in specialist clinics and 18.8% in general neurology consultations (P=.032) (Fig. 1). However, no significant differences were observed in the availability of PC resources between different types of consultation.
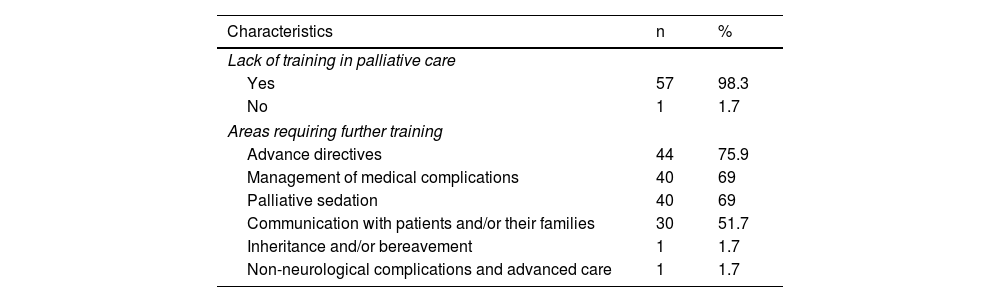
Regarding PC training, all respondents but one (98.3%) believed that neurologists had insufficient training in PC; the areas identified as most urgently requiring training were advance directives (75.9%), management of medical complications (69%), and palliative sedation (69%) (Table 2).
Palliative care training for neurologists.
| Characteristics | n | % |
|---|---|---|
| Lack of training in palliative care | ||
| Yes | 57 | 98.3 |
| No | 1 | 1.7 |
| Areas requiring further training | ||
| Advance directives | 44 | 75.9 |
| Management of medical complications | 40 | 69 |
| Palliative sedation | 40 | 69 |
| Communication with patients and/or their families | 30 | 51.7 |
| Inheritance and/or bereavement | 1 | 1.7 |
| Non-neurological complications and advanced care | 1 | 1.7 |
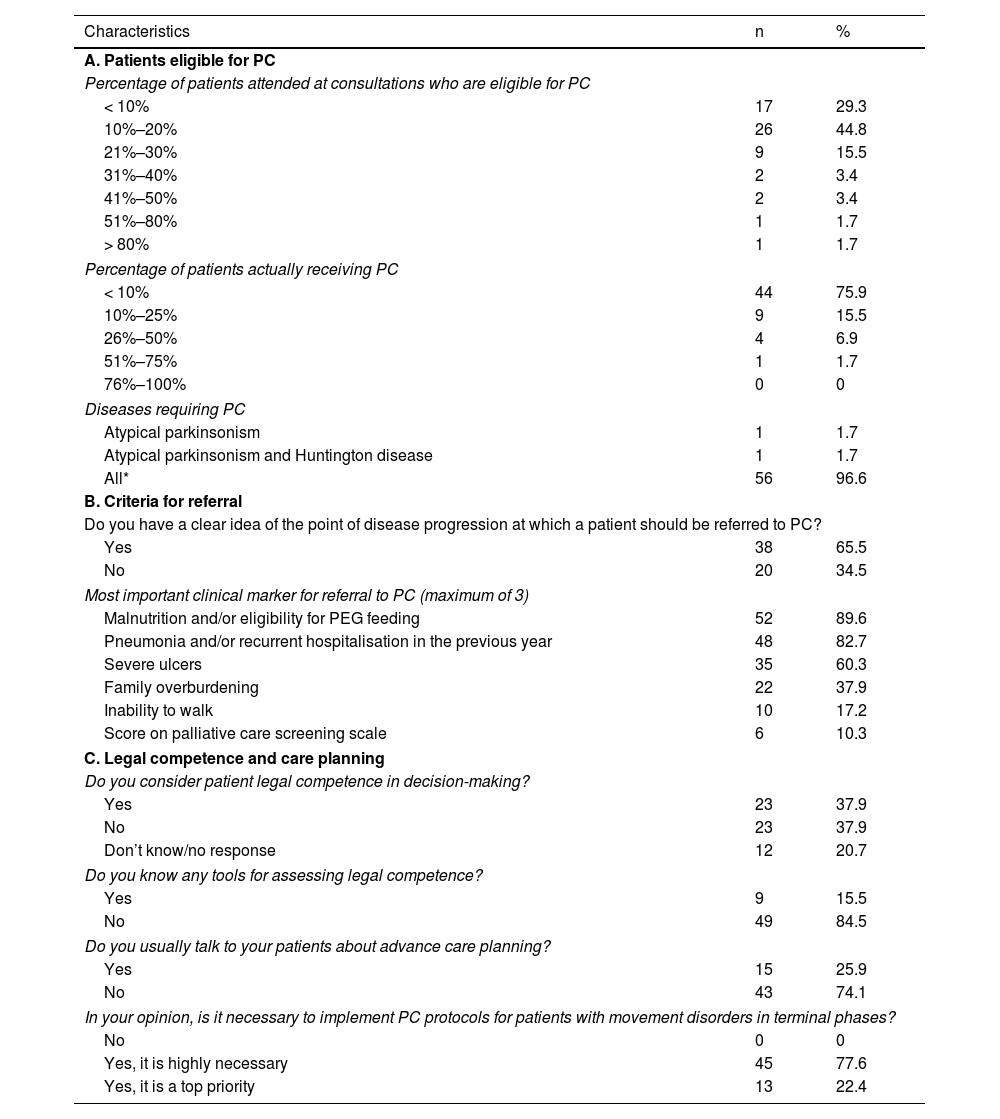
Regarding clinical practice and patient management, 70.7% of respondents reported that at least 10% of patients with movement disorders attended at their consultation or unit were eligible for PC: 10%–20% of patients, according to 44.8% of respondents; 51%–80% of patients, according to 1.7%; and > 80%, according to a further 1.7% (Table 3). However, 75.9% reported that fewer than 10% of their patients with movement disorders who were eligible for PC actually received this type of care. By disease, nearly all respondents (56/58) believed that any disease causing a movement disorder may at some point require PC; the survey specifically enquired about PD, atypical parkinsonism, and Huntington’s disease. One in 3 respondents (34.5%) were unsure about the specific point of disease progression at which the patient should be referred to the PC unit (Table 3). In the view of the survey respondents, the most relevant clinical markers in the decision to refer a patient to the PC unit were malnutrition and/or eligibility for feeding by percutaneous endoscopic gastrostomy (89.6%), pneumonia and/or recurrent hospitalisation in the previous year (82.7%), and severe ulcers (60.3%).
Palliative care provided by neurologists.
| Characteristics | n | % |
|---|---|---|
| A. Patients eligible for PC | ||
| Percentage of patients attended at consultations who are eligible for PC | ||
| < 10% | 17 | 29.3 |
| 10%–20% | 26 | 44.8 |
| 21%–30% | 9 | 15.5 |
| 31%–40% | 2 | 3.4 |
| 41%–50% | 2 | 3.4 |
| 51%–80% | 1 | 1.7 |
| > 80% | 1 | 1.7 |
| Percentage of patients actually receiving PC | ||
| < 10% | 44 | 75.9 |
| 10%–25% | 9 | 15.5 |
| 26%–50% | 4 | 6.9 |
| 51%–75% | 1 | 1.7 |
| 76%–100% | 0 | 0 |
| Diseases requiring PC | ||
| Atypical parkinsonism | 1 | 1.7 |
| Atypical parkinsonism and Huntington disease | 1 | 1.7 |
| All* | 56 | 96.6 |
| B. Criteria for referral | ||
| Do you have a clear idea of the point of disease progression at which a patient should be referred to PC? | ||
| Yes | 38 | 65.5 |
| No | 20 | 34.5 |
| Most important clinical marker for referral to PC (maximum of 3) | ||
| Malnutrition and/or eligibility for PEG feeding | 52 | 89.6 |
| Pneumonia and/or recurrent hospitalisation in the previous year | 48 | 82.7 |
| Severe ulcers | 35 | 60.3 |
| Family overburdening | 22 | 37.9 |
| Inability to walk | 10 | 17.2 |
| Score on palliative care screening scale | 6 | 10.3 |
| C. Legal competence and care planning | ||
| Do you consider patient legal competence in decision-making? | ||
| Yes | 23 | 37.9 |
| No | 23 | 37.9 |
| Don’t know/no response | 12 | 20.7 |
| Do you know any tools for assessing legal competence? | ||
| Yes | 9 | 15.5 |
| No | 49 | 84.5 |
| Do you usually talk to your patients about advance care planning? | ||
| Yes | 15 | 25.9 |
| No | 43 | 74.1 |
| In your opinion, is it necessary to implement PC protocols for patients with movement disorders in terminal phases? | ||
| No | 0 | 0 |
| Yes, it is highly necessary | 45 | 77.6 |
| Yes, it is a top priority | 13 | 22.4 |
PC: palliative care; PEG: percutaneous endoscopic gastrostomy.
Only one in 4 respondents (25.9%) reported that they frequently provided advance care planning. Furthermore, although 37.9% indicated that they considered patients’ legal competence during decision-making, the vast majority (84.5%) did not know the tools needed to evaluate legal competence (Table 3). Although differences were not significant, we observed that a higher percentage of neurologists working at general neurology consultations reported knowing the tools needed to evaluate patient legal competence (25%, vs 5.6% and 16.7% of those working at specialist clinics and MDUs, respectively; P=.289); furthermore, these neurologists more frequently discussed advance care planning with their patients (Fig. 1). All respondents (100%) agreed on the need to implement PC protocols for patients with movement disorders in advanced stages; 77.6% believed this to be highly necessary and 22.4% considered it a top priority.
After data collection was complete, we contacted the 5 centres that, according to the respondents from those centres, had a specific PC protocol for patients with movement disorders; these centres indicated that no such official protocol was in place, although physicians did occasionally work with PC teams for the management of specific patients.
DiscussionThe results of our survey reveal overwhelming agreement among neurologists from across Spain that PC should be provided to patients with movement disorders. However, most neurologists reported that only a small percentage of patients eligible for PC actually receive this care (less than 10%, according to three-quarters of respondents). Although these results only reflect the opinions of neurologists specialising in movement disorders, they do reveal important shortcomings in the integral care of these patients and their families. In this regard, a study conducted in the Spanish city of Málaga analysed the most frequent diseases in patients eligible for PC who did or did not receive PC before death. Of the 950 patients studied, 417 (43.9%) were eligible for PC, but only 277 of these (66.4%) actually received PC. The most frequent diseases among patients eligible for PC were cancer (61.9%), Alzheimer disease and dementia (19.9%), and chronic obstructive pulmonary disease (6.2%). However, among the patients actually receiving PC, the percentage with cancer was higher (86.8%), whereas Alzheimer disease and dementia (20.5%) and PD (13.8%) were less frequent.14 Both our study and the study conducted by Martínez Ríos et al.14 show the need to expand and improve PC at all levels in Spain, with a particular emphasis on neurodegenerative diseases. Furthermore, in several countries, a considerable proportion of all deaths due to PD occur at hospitals, which are probably not the optimal setting for end-of-life care and death. Efforts should be made to reduce the number of patients with movement disorders who die in hospital15; PC may be a great help in achieving this.
Our results also reflect the lack of PC protocols for neurodegenerative diseases that cause movement disorders, despite the large number of PC units available at Spanish hospitals. Although guidelines for PC have been published in Spain (https://www.secpal.org), little reference is made to the care of patients with movement disorders. This should encourage us to improve collaboration with PC specialists, drafting joint guidelines and improving care processes.
One area for improvement identified in our study is PC training for neurologists. Most respondents agreed that they needed to deepen their knowledge of palliative therapies and advance directives. Advance care planning, including the drafting of advance directives, helps minimise suffering and reduce unnecessary medical care (unwanted hospitalisation, unnecessary procedures, etc).16 An ever-growing number of people have a clear idea of the care they wish to receive at the end of life, and we should endeavour to fulfil these wishes. Advance care planning should be considered as soon as the disease is diagnosed, before the patient begins to present cognitive impairment, to ensure their legal competence is not affected.17 In our study, nearly half of respondents reported knowing what legal competence is and how it affects decision-making; however, most did not know how to assess it. This represents a contradiction, and reflects a lack of training and understanding of this subject, suggesting that patients’ legal competence is not being considered in decision-making. In this sense, only one in 4 neurologists frequently explain advance care planning to their patients, including advance directives. This low rate seems not to be exclusive to neurologists attending patients with movement disorders. A study recently conducted in 4 hospitals in Madrid explored healthcare professionals’ perceptions of advance directives with a view to improving understanding of their lack of success among physicians, concluding that these documents are not used in clinical practice due to the complexity of their implementation, lack of education (both for professionals and the general population), and the lack of procedural clarity.18 As a consequence, healthcare professionals are not aware of how advance directives can improve clinical decision-making, when and for whom they are appropriate, and who is responsible for providing information about them. This situation contributes to patients’ lack of interest in drafting these documents and physicians’ scepticism about their usefulness. It is essential to expand physicians’ knowledge about advance directives, underscoring the need to develop strategies to improve training about this tool. Furthermore, patients with PD and other parkinsonisms seem to be more sensitive to advance directives; one study found that these patients are more likely to use advance directives than controls.19 This should further encourage us to talk with our patients about these documents and to develop other educational initiatives to raise awareness about advance care planning in the community.20
In chronic diseases, doctor-patient communication is key to building trust and ensuring treatment adherence. According to our survey, over 30% of respondents believed that communication skills were an area for improvement. In PD, quality of life depends not only on the adequate control of motor and non-motor symptoms but also on the patient-doctor relationship and treatment compliance; the latter factor is directly linked to the quality of doctor-patient relationships.21 PC frequently has negative connotations, causing aversion among patients and their families, many of whom associate PC with the end of life. Optimising communication skills, as respondents to our survey suggest, would not only improve the perception and acceptance of PC by patients and their families, but would also encourage patients to prepare advance directives, taking a more active role in their disease.
Regarding the practical question of when and how PC should be provided, our study shows that although over half of neurologists know when to refer a patient to PC, the criteria for referral vary, probably because they are not based on unified, reproducible scales or tools. International guidelines have also underscored the need for training and the lack of specific tools as obstacles to the implementation of PC, particularly highlighting inadequate training during the neurology residency or training in movement disorders, and the lack of evidence-based studies that justify and guide PC models and therapeutic interventions. Therefore, research efforts should be focused on the validation of needs assessment tools to guide patient selection, validation of outcome measures, evaluation of patient and caregiver interventions, and dissemination and implementation efforts.22
Our study presents several limitations. Firstly, it included a small sample, with a total of 58 valid survey responses. Only a small proportion of the neurologists who received the e-mail completed the survey, which may have introduced a selection bias. We did not enquire about the number of patients treated by the respondents, or their experience with the management of movement disorders, although we assume that all respondents were experienced in this field as they all were members of the GETM. Furthermore, over 90% of responses were submitted by neurologists working at public healthcare centres. Our results must therefore be interpreted with caution. In any case, they provide interesting data, as this is, to our knowledge, the first study into expert opinions about the current state of PC for movement disorders in Spain. In fact, responses were received from neurologists working in nearly all Spanish autonomous communities, providing a global view. We found no differences in the resources available at general neurology consultations, specialist clinics, or MDUs, except the availability of nurses specialising in movement disorders, which was only reported at MDUs. In spite of the small size of our sample, our results suggest that there are no substantial differences in patient management in Spain, reflecting equitable care regardless of the region or type of consultation. Our survey did not enquire about the time allocated to PC planning and execution, including advance care planning. Another limitation is that some responses were submitted by several neurologists working at the same centre and others were even inaccurate, such as those reporting the availability of a PC protocol for patients with movement disorders; this provides further evidence of the limited knowledge about PC among neurologists.
Despite advances in the treatment of PD in recent decades, many barriers remain for the integration of PC in the management of patients with movement disorders. There is growing interest in the development of an action plan aiming to minimise the suffering and improve the quality of life of patients with movement disorders and their families, while new lines of research are focusing on the development of new symptomatic and curative treatments.23
Although the present study is merely descriptive and reports data from a small sample, our results reveal significant deficits in the management of movement disorders, and provide a starting point for the development of a plan for improvement. Even small changes may result in substantial improvements in the quality of life of these patients and their families. These results should motivate us to design awareness campaigns for neurologists and other healthcare professionals involved in the care of patients with movement disorders, implement specific training programmes, and develop protocols for early identification of patients who may benefit from PC. The shortcomings in PC revealed by our study should serve as a stimulus to support multidisciplinary work and the implementation of organisational changes to enable more tailored management of these patients’ changing needs.
Conflicts of interestThe authors have no conflicts of interest to declare.
We wish to thank the staff of the Spanish Society of Neurology, all members of the GETM, and the neurologists who completed our survey.