To evaluate long-term quality of life (QoL) in patients who have experienced a stroke and to analyse differences in QoL between sexes.
MethodsWe conducted a descriptive, cross-sectional, observational study to gather sociodemographic variables and risk factors; data were also obtained on QoL, mood, and functional status using validated scales. The study was approved by our centre's ethics committee.
ResultsOur final sample included 124 patients; mean age was 71.30±11.99 years. In the QoL study, the EuroQol-5D dimensions in which participants presented most problems were anxiety/depression (66.7%) and pain/discomfort (62.2%). We found significant inter-sex differences in the dimensions of mobility and usual activities (P=.016 and P=.005, respectively). Women also achieved substantially poorer EuroQoL-5D index values than men (0.45±0.45 vs 0.65±0.38; P=.013). QoL was found to be associated with dependence for the activities of daily living (r=0.326; P=.001) and depressed mood (r=−0.514; P<.0001). According to the predictive model for the EQ-5D index, 72% of the score on QoL items is explained by functional status, dependence for the activities of daily living (basic and instrumental), and depressed mood. Being married, in contrast, seems to be a protective factor.
ConclusionStroke survivors have poor long-term QoL; this is more marked in women than in men, especially in the dimensions of mobility and usual activities.
Valorar la calidad de vida (CV) a largo plazo en pacientes que presentaron un ictus y analizar si existen diferencias entre sexos.
MétodosEstudio descriptivo, observacional, transversal. El estudio fue aprobado por el Comité Ético. Se recogieron datos sociodemográficos, factores de riesgo, datos sobre la CV, el estado de ánimo y el estado funcional mediante escalas validadas.
ResultadosLa muestra final obtenida fue de 124 pacientes. La edad media fue 71,30 años (DE: 11,99). En el estudio de la CV, las dimensiones que presentaron más problemas en el cuestionario EuroQol-5D fueron las de ansiedad/depresión (66,7%) y dolor/malestar (62,2%). Hubo diferencias significativas entre mujeres y hombres en las dimensiones movilidad y actividades cotidianas (p=0,016 y p=0,005). Y en el índice de salud del EQ-5D, también fue peor el resultado en mujeres que en hombres (0,45±0,45 vs. 0,65±0,38; p=0,013). La CV se relacionó con la dependencia en las actividades básicas de la vida diaria (r=0,326; p=0,001) y con el estado de ánimo deprimido (r=−0,514; p<0,0001). El modelo de predicción, para el índice del cuestionario de CV EQ-5D, estableció que el 72% de la puntuación obtenida en la CV estaría explicada por el estado funcional, la dependencia en las actividades de la vida diaria y el estado de ánimo, mientras que el estar casado aparece como factor protector.
ConclusiónLa CV de los supervivientes a un ictus está afectada negativamente a largo plazo. Son las mujeres las que manifiestan una CV peor, sobre todo en las dimensiones de movilidad y actividades cotidianas.
Stroke constitutes a major public health problem, given its considerable impact on patients, families, and society.1,2 Despite improved control of risk factors, the incidence of cerebrovascular disease will progressively increase due to population ageing and other sociodemographic changes.3
In recent years, patient-reported outcomes have become increasingly relevant both in clinical practice and in healthcare planning.4 The traditional medical model describes treatment outcomes in terms of recovery, remission, or recurrence. However, these outcomes are not applicable to chronic illnesses as they do not account for the true impact of the condition on the patient's family, social, or professional life.5 This has sparked a growing interest in the psychosocial dimension of the disease, with life expectancy interpreted as an increase in quality of life rather than as an increase in the number of years lived; these concepts have been incorporated into clinical outcomes.6
Self-perceived health status and health-related quality of life (HRQoL) complement data from traditional markers of health7 and provide more specific information on health status and treatment effectiveness from patients’ perspective.8
This information is essential in the case of stroke due to the severity of the condition and the wide range of areas affected (cognitive, sensory/motor, functional, and psychological); assessing the impact of stroke on survivors’ HRQoL is as important as evaluating disability and survival.6
Our study aimed to assess long-term HRQoL in patients with stroke, to analyse whether perceived quality of life varied between sexes, and to identify the factors associated with poorer HRQoL.
Patients and methodsWe conducted an observational, descriptive, cross-sectional study between November 2014 and June 2015. The sample included patients who presented stroke between September 2009 and June 2010 and were admitted to our hospital's stroke unit.
Patients with aphasia or moderate-to-severe cognitive impairment were excluded, as these conditions hinder proper communication.
Participants were selected using the stroke unit's database; they were contacted by telephone and informed about the purpose of the study. Patients willing to participate were interviewed at our hospital, in a quiet environment that guaranteed privacy and confidentiality. During the interview, they completed a series of questionnaires about their quality of life, mood, and functional status.
We gathered data on sociodemographic variables, risk factors, and comorbidities. We used the European Quality of Life-5 Dimensions (EQ-5D) questionnaire9 to determine HRQoL, the Barthel Index (BI)10 to quantify the level of dependence in the basic activities of daily living (ADL), and the Lawton-Brody Instrumental Activities of Daily Living (IADL) scale10 to determine functional ability for instrumental activities. Mood was evaluated using the Hamilton Depression Rating Scale (HDRS).11,12
InstrumentsThe EQ-5D9 is a generic tool for measuring HRQoL, where patients rate their self-perceived health status using a descriptive system rating the severity of different dimensions, and a visual analogue scale (VAS) for a more general assessment. The descriptive system addresses 5 health dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), each divided into 3 levels of perceived problems (no problems, moderate problems, and severe problems). The questionnaire also contains a 20-cm vertical VAS scored from 0 (worst imaginable health status) to 100 (best imaginable health status). The VAS score complements the results of the EQ-5D descriptive system. Furthermore, health status may be converted to a single index by applying the crosswalk link function, which weights each level on each dimension. Each health status is assigned a value according to a specific set of values that measure health states. The index ranges from 1 (best imaginable health status) to 0 (death), although it may take negative values, reflecting health statuses perceived as worse than death.
The Barthel Index10 evaluates the level of dependence in ADLs; the scale ranges from 0 (total dependence) to 100 (complete independence), with scores categorised as total dependence (0-20), severe dependence (21-40), moderate dependence (41-60), slight dependence (61-90), or independence (91-100).
The Lawton-Brody IADL scale10 evaluates functional capacities, particularly physical and instrumental independence in ADLs; it may therefore be used to complement BI data on functional ability. The scale contains 8 items assessing instrumental ADLs. Each item has several possible answers, which are scored either 0 or 1. Final scores range from 0 (completely dependent) to 8 (independent).
The Hamilton Depression Rating Scale11,12 is administered by a healthcare professional and is designed to measure the severity of depression. The HDRS is one of the most widely used tools for evaluating mood and affective disorders.12
The Spanish-language version of the scale was validated in 1986.11 Each item has 3 or 5 possible responses, scored from 0 to 2 or from 0 to 4, respectively. The cut-off points used for defining the levels of depression severity are those recommended by the American Psychiatric Association and the Spanish Ministry of Health's clinical practice guidelines on the management of major depression in adults.12
Data confidentiality and ethical considerationsAll patients signed an informed consent form before being included in the study. Data were anonymised to protect patient confidentiality. Only the lead researcher had access to patient data.
The study complies with the applicable ethical standards and with the principles of the Declaration of Helsinki. The study was approved by our hospital's Clinical Research Ethics Committee.
Data analysisWe performed a descriptive analysis for all variables. Categorical variables are expressed as percentages and quantitative variables as means and standard deviations (SD). Correlations between qualitative variables were analysed using the chi-square test. Quantitative variables were compared using the Kolmogorov-Smirnov test for normality. We used parametric (t test, ANOVA, or Pearson correlation coefficient) and non-parametric tests (Mann–Whitney U test, Kruskal–Wallis test, or Spearman correlation coefficient), depending on whether variables followed a normal distribution. We also analysed the relative risk (odds ratio) and performed a predictive study with a multivariate linear regression model. Data were analysed using SPSS statistical software (version 20) for Windows. We used an alpha level of 0.05.
ResultsA total of 218 patients were admitted between September 2009 and June 2010. By the time the study was performed, 38 had died, 19 had dementia or aphasia, 15 could not be contacted, and 20 declined to participate in the study or lived in other Spanish provinces and therefore had difficulties attending our hospital for the assessment. The final sample included 124 patients.
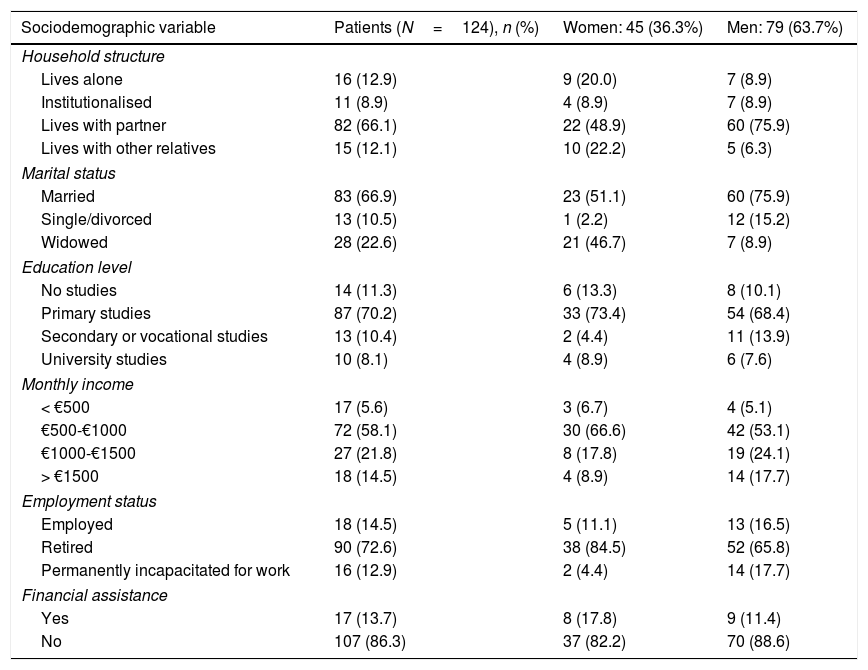
Mean age (SD) was 71.30 (11.99) years; women were older than men (73.58 [SD: 12.47] vs 70 [11.59]), although differences were not statistically significant (P=.111). Patients’ sociodemographic characteristics are listed in Table 1. Most patients were married and had a monthly income ranging from €500 to €1000. A total of 97.6% of patients were receiving at least one drug and 21% had recurrent stroke.
Sociodemographic characteristics of our sample.
| Sociodemographic variable | Patients (N=124), n (%) | Women: 45 (36.3%) | Men: 79 (63.7%) |
|---|---|---|---|
| Household structure | |||
| Lives alone | 16 (12.9) | 9 (20.0) | 7 (8.9) |
| Institutionalised | 11 (8.9) | 4 (8.9) | 7 (8.9) |
| Lives with partner | 82 (66.1) | 22 (48.9) | 60 (75.9) |
| Lives with other relatives | 15 (12.1) | 10 (22.2) | 5 (6.3) |
| Marital status | |||
| Married | 83 (66.9) | 23 (51.1) | 60 (75.9) |
| Single/divorced | 13 (10.5) | 1 (2.2) | 12 (15.2) |
| Widowed | 28 (22.6) | 21 (46.7) | 7 (8.9) |
| Education level | |||
| No studies | 14 (11.3) | 6 (13.3) | 8 (10.1) |
| Primary studies | 87 (70.2) | 33 (73.4) | 54 (68.4) |
| Secondary or vocational studies | 13 (10.4) | 2 (4.4) | 11 (13.9) |
| University studies | 10 (8.1) | 4 (8.9) | 6 (7.6) |
| Monthly income | |||
| < €500 | 17 (5.6) | 3 (6.7) | 4 (5.1) |
| €500-€1000 | 72 (58.1) | 30 (66.6) | 42 (53.1) |
| €1000-€1500 | 27 (21.8) | 8 (17.8) | 19 (24.1) |
| > €1500 | 18 (14.5) | 4 (8.9) | 14 (17.7) |
| Employment status | |||
| Employed | 18 (14.5) | 5 (11.1) | 13 (16.5) |
| Retired | 90 (72.6) | 38 (84.5) | 52 (65.8) |
| Permanently incapacitated for work | 16 (12.9) | 2 (4.4) | 14 (17.7) |
| Financial assistance | |||
| Yes | 17 (13.7) | 8 (17.8) | 9 (11.4) |
| No | 107 (86.3) | 37 (82.2) | 70 (88.6) |
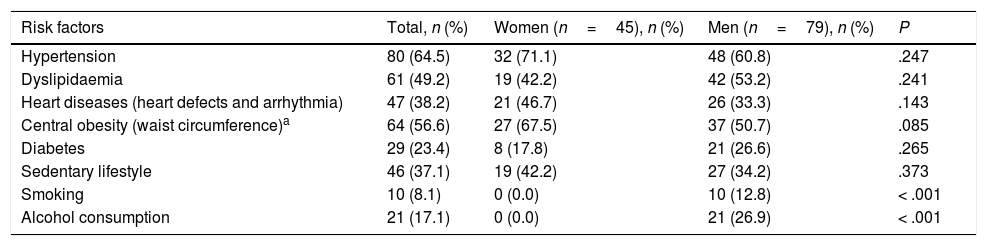
Table 2 shows the risk factors present in our sample: the most prevalent were arterial hypertension (64.5%), dyslipidaemia (49.2%), and heart disease (38.2%). We observed differences in alcohol and tobacco use between men and women.
Risk factors in our sample.
| Risk factors | Total, n (%) | Women (n=45), n (%) | Men (n=79), n (%) | P |
|---|---|---|---|---|
| Hypertension | 80 (64.5) | 32 (71.1) | 48 (60.8) | .247 |
| Dyslipidaemia | 61 (49.2) | 19 (42.2) | 42 (53.2) | .241 |
| Heart diseases (heart defects and arrhythmia) | 47 (38.2) | 21 (46.7) | 26 (33.3) | .143 |
| Central obesity (waist circumference)a | 64 (56.6) | 27 (67.5) | 37 (50.7) | .085 |
| Diabetes | 29 (23.4) | 8 (17.8) | 21 (26.6) | .265 |
| Sedentary lifestyle | 46 (37.1) | 19 (42.2) | 27 (34.2) | .373 |
| Smoking | 10 (8.1) | 0 (0.0) | 10 (12.8) | < .001 |
| Alcohol consumption | 21 (17.1) | 0 (0.0) | 21 (26.9) | < .001 |
Only 27.4% of patients had normal weight (26.2% of women and 28.0% of men), with nearly 50% of the sample being overweight.
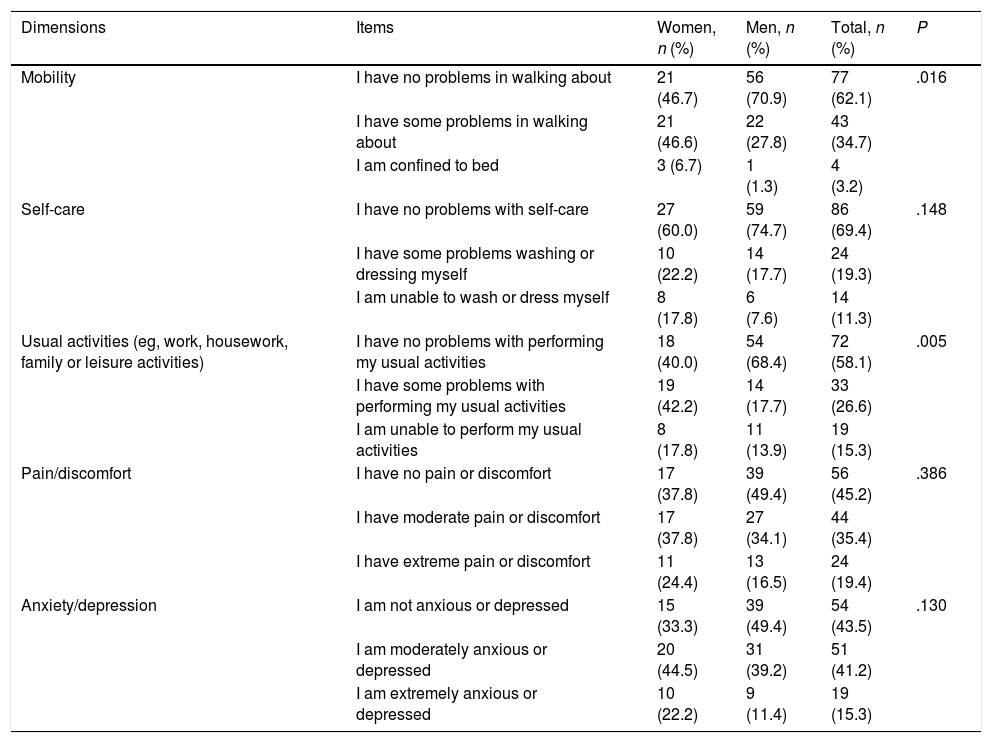
Quality of lifePatients’ self-perceived quality of life was average or poor in nearly 33.9% of cases. Table 3 shows the results of each dimension of the EQ-5D, broken down by sex. The dimensions showing most problems (both moderate and severe) were anxiety/depression (66.7%), pain/discomfort (62.2%), and usual activities (60.0%). Differences between men and women were statistically significant for mobility (P=.016) and usual activities (P=.005). Statistically significant differences were also observed between sexes in the EQ-5D index (VAS), with men showing better quality of life (0.65 points [0.38] vs 0.45 points [0.45] in women; P=.013).
Results from the European Quality of Life-5 Dimensions questionnaire, broken down by sex.
| Dimensions | Items | Women, n (%) | Men, n (%) | Total, n (%) | P |
|---|---|---|---|---|---|
| Mobility | I have no problems in walking about | 21 (46.7) | 56 (70.9) | 77 (62.1) | .016 |
| I have some problems in walking about | 21 (46.6) | 22 (27.8) | 43 (34.7) | ||
| I am confined to bed | 3 (6.7) | 1 (1.3) | 4 (3.2) | ||
| Self-care | I have no problems with self-care | 27 (60.0) | 59 (74.7) | 86 (69.4) | .148 |
| I have some problems washing or dressing myself | 10 (22.2) | 14 (17.7) | 24 (19.3) | ||
| I am unable to wash or dress myself | 8 (17.8) | 6 (7.6) | 14 (11.3) | ||
| Usual activities (eg, work, housework, family or leisure activities) | I have no problems with performing my usual activities | 18 (40.0) | 54 (68.4) | 72 (58.1) | .005 |
| I have some problems with performing my usual activities | 19 (42.2) | 14 (17.7) | 33 (26.6) | ||
| I am unable to perform my usual activities | 8 (17.8) | 11 (13.9) | 19 (15.3) | ||
| Pain/discomfort | I have no pain or discomfort | 17 (37.8) | 39 (49.4) | 56 (45.2) | .386 |
| I have moderate pain or discomfort | 17 (37.8) | 27 (34.1) | 44 (35.4) | ||
| I have extreme pain or discomfort | 11 (24.4) | 13 (16.5) | 24 (19.4) | ||
| Anxiety/depression | I am not anxious or depressed | 15 (33.3) | 39 (49.4) | 54 (43.5) | .130 |
| I am moderately anxious or depressed | 20 (44.5) | 31 (39.2) | 51 (41.2) | ||
| I am extremely anxious or depressed | 10 (22.2) | 9 (11.4) | 19 (15.3) |
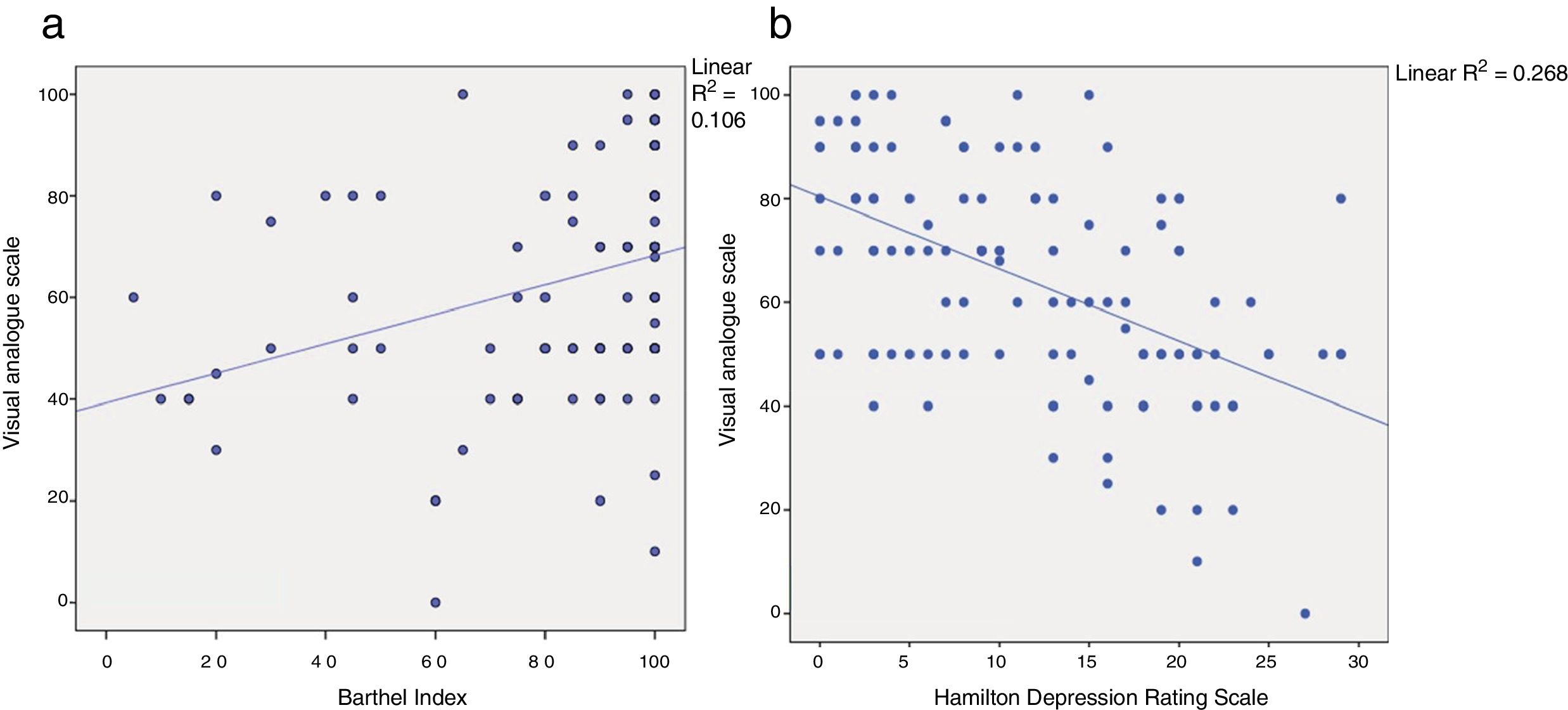
This index was found to be correlated with BI scores (r=0.326; P<.001): patients with greater independence in ADLs reported better quality of life (Fig. 1a). Independent patients scored higher on the VAS for quality of life than dependent patients (71.04 points [SD: 18.96] vs 53.37 [20.67]; P<.001).
Furthermore, quality of life as rated with the VAS was inversely correlated with mood (r=−0.514; P<.0001): higher HDRS scores were associated with poorer self-perceived quality of life (Fig. 1b). Patients with a depressed mood scored lower on the VAS (51.30 [SD: 19.91] vs 72.68 [17.87]; P<.0001). Sleep disorders (sleep-onset, sleep-maintenance, or terminal insomnia) were also associated with poorer quality of life. Patients without sleep disorders scored a mean of 72.34 (18.52) points whereas those with sleep disorders scored 55.77 (21.02) (P<.001). However, no associations were identified between quality of life and such other variables as older age (P=.111) or obesity (P=.795).
We found a statistically significant difference between presence of pain/discomfort and poorer quality of life (patients without pain scored a mean of 71.75 [20.03] points and those with pain scored 57.72 [20.54]; P<.001). Likewise, we found a statistically significant correlation between pain and dependence, for both basic and instrumental ADLs (P=.037 and P=.025, respectively).
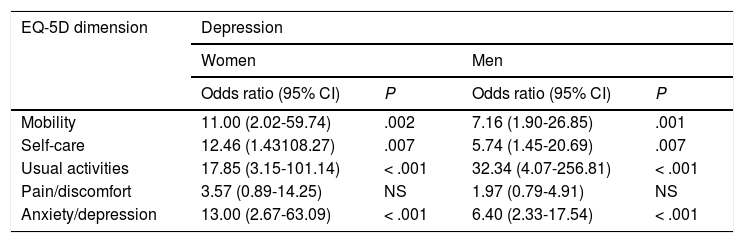
Table 4 shows the risk analysis for EQ-5D dimensions and depressive mood, broken down by sex. All dimensions but pain/discomfort were associated with depression in both men and women.
Inter-sex differences for quality of life dimensions in patients with depression (odds ratios).
| EQ-5D dimension | Depression | |||
|---|---|---|---|---|
| Women | Men | |||
| Odds ratio (95% CI) | P | Odds ratio (95% CI) | P | |
| Mobility | 11.00 (2.02-59.74) | .002 | 7.16 (1.90-26.85) | .001 |
| Self-care | 12.46 (1.43108.27) | .007 | 5.74 (1.45-20.69) | .007 |
| Usual activities | 17.85 (3.15-101.14) | < .001 | 32.34 (4.07-256.81) | < .001 |
| Pain/discomfort | 3.57 (0.89-14.25) | NS | 1.97 (0.79-4.91) | NS |
| Anxiety/depression | 13.00 (2.67-63.09) | < .001 | 6.40 (2.33-17.54) | < .001 |
EQ-5D: European Quality of Life-5 Dimensions questionnaire; NS: not significant.
The model adjusted for sex, dependence in instrumental ADLs, and mood showed that mobility and self-care were independently associated with basic ADLs in men (OR=12.54; 95% CI, 2.41-65.27; P=.03 and OR=75.03; 95% CI, 5.28-106.51; P=.01, respectively), whereas anxiety/depression was associated with depression (HDRS) in both sexes (women: OR=16.48; 95% CI, 1.99-136.53; P=.009; men: OR=5.12; 95% CI, 1.68-15.67; P=.004).
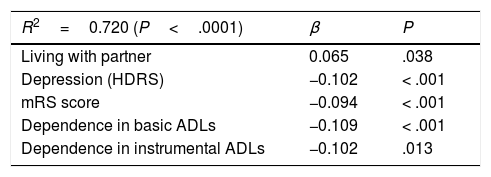
The predictive model for the EQ-5D index (Table 5) was built using multivariate linear regression: 72% of quality of life scores were explained by functional status, dependence in ADLs (basic and instrumental), and depression, whereas living with the partner (social support) seems to be a protective factor.
Predictive model of quality of life.
| R2=0.720 (P<.0001) | β | P |
|---|---|---|
| Living with partner | 0.065 | .038 |
| Depression (HDRS) | −0.102 | < .001 |
| mRS score | −0.094 | < .001 |
| Dependence in basic ADLs | −0.109 | < .001 |
| Dependence in instrumental ADLs | −0.102 | .013 |
Variables included in the model: age, sex, socioeconomic level, sequelae, insomnia, dysarthria, motor impairment, body mass index, hypertension, diabetes. ADL: activities of daily living; HDRS: Hamilton Depression Rating Scale; mRS: modified Rankin Scale.
According to the HDRS, 64.2% of patients had a depressed mood; 31.7% of these had moderate-to-severe depression, 23.6% had minor depression, and 8.9% had major depression. The mean HDRS score in our sample was 11.73 points, with significant differences between men and women: women scored higher on the scale, indicating more severe depression (14.04 [SD: 8.32] vs 10.42 [7.5]; P=.014).
Patients unable to walk had more severe depression than those capable of walking (16.57 [6.61] vs 8.78 [7.28]; P<.001): patients with mobility problems were nearly 9 times more likely to have depression (OR=8.85; 95% CI, 3.15-24.81; P<.001). The same was true for patients who were unable to care for themselves (16.53 [6.51] vs 9.62 [7.65]; P<.001), with an OR of 7.55 (95% CI, 2.46-23.16; P<.001).
Patients with more severe depression had a higher level of dependence in basic (r=−0.459; P<.001) and instrumental ADLs (r=−0.467; P<.001). We found no significant correlation between presence of depression and age (P=.503).
Patients with depression were more likely to have sleep disorders than those without (64.5% vs 16.1%; P<.001).
Functional statusAnalysis of functional status showed that 60.5% of patients were independent in basic ADLs, whereas the remaining 39.5% presented some degree of dependence.
The Lawton-Brody IADL scale confirmed that 60.5% were independent in instrumental ADLs, whereas 21.0% showed complete or severe dependence and 18.5% presented moderate dependence.
Independence in the basic ADLs was found to be inversely correlated with age (r=−0.367; P<.001). We observed statistically significant differences in basic ADLs between sexes, with higher BI scores for men (89.11 [21.76] vs 78.67 [26.53]; P=.019).
DiscussionLong-term quality of life after stroke varies between sexes. Functional status, level of dependence, and mood have an impact on self-perceived quality of life. Few studies have evaluated these differences in the long term.
The risk factors and clinical and sociodemographic characteristics of our sample are similar to those described in other studies13,14; our results provide further evidence that arterial hypertension and dyslipidaemia are the most prevalent risk factors in these patients. Furthermore, our sample included a considerably lower percentage of smokers than the ICTUSCARE study13 (8% vs 25.1%), probably due to the implementation of smoking bans and the increased awareness of the harmful effects of smoking. These results encourage continued efforts to improve long-term control of cerebrovascular disease risk factors, with a particular emphasis on changing lifestyle habits and monitoring treatment adherence.14
As seen in other series,6,15,16 our sample showed sex-related differences in HRQoL: women have poorer quality of life than men, and living with a partner has a positive impact on self-perceived quality of life.
In our study, as previously reported by Bushnell et al.,16 women achieved poorer results in the EQ-5D dimensions of mobility and usual activities. In line with previous studies,17–20 Bushnell and colleagues suggest that women have more limitations in muscle function (more severe stroke, older age, poorer functional status before stroke, and more concomitant diseases). This fact may influence physical recovery, explaining sex differences in BI scores, and consequently women's higher level of dependence in basic ADLs.20–22 In these studies, differences were observed 3 months after stroke occurrence. In our sample, such differences persisted at 5 years.
Another interesting finding of our study is that women showed more limitations in basic or instrumental ADLs; this may be due to the fact that, in our setting, domestic tasks are considered “women's work,”10 resulting in women's continued responsibility for these tasks after retirement. This may explain men scoring higher in the dimension of usual activities, since most were retired and therefore may not perform or feel that they did not perform any usual activities. Poor performance in domestic tasks may also have an impact on overall HRQoL and mood, as it may be linked to a feeling of uselessness.
According to some studies,22,23 the first year and particularly the first months after stroke are crucial in improving HRQoL and physical function; these studies also report a correlation between basic and instrumental ADLs and HRQoL.
Depression is the most frequent affective disorder in these patients.24 A recent systematic review calculated the prevalence of post-stroke depression at 31%,25 although this rate may be underestimated. In fact, 64.2% of our patients had depression, with nearly 41% of patients showing severe or major depression. As reported in other studies,26,27 post-stroke depression is associated with pain and functional dependence and is an important factor in patients’ quality of life. In line with the literature,26,28,29 post-stroke depression was found to be more frequent in women, and is strongly associated with HRQoL: poorer quality of life is associated with depression. Furthermore, failure to detect depression early may have a major impact on patients and healthcare systems,27 as early diagnosis may improve functional recovery.24 In our sample, the association between depression and HRQoL persisted in the long term.
The patients who had difficulties participating and were therefore not included in the study may have been those with the most severe problems and sequelae; although they account for only a small proportion of the cohort, their exclusion may constitute a source of bias.
The scales used in our study (Lawton-Brody IADL scale, HDRS, and EQ-5D) enable comprehensive, holistic assessment of quality of life, functional status, and mood.
Future studies should analyse the impact of different adaptation processes and coping strategies for sequelae on patients with different personality traits, focusing on the impact of concomitant diseases on quality of life. Participants’ cultural setting should also be considered as it is usually more demanding for women, who continue to perform domestic tasks during retirement: less efficient performance of these tasks may negatively impact their mood and other dimensions of quality of life.
ConclusionDespite technical and scientific advances in the rehabilitation of patients with cerebrovascular diseases, survivors’ quality of life frequently decreases in the long term. Women tend to show poorer quality of life than men, particularly in the dimensions of mobility and usual activities.
Female sex, pain, functional dependence, and depression are significantly associated with poorer HRQoL, whereas being married (i.e., having social support) has a positive impact on quality of life.
Effective interventions on these factors may help improve HRQoL in stroke survivors.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank all patients and their families for their participation, and the management and directors of our healthcare area for their support for research on stroke care.
We also wish to thank Irene, Jaime, and Elena.
Please cite this article as: López Espuela F, Portilla Cuenca JC, Leno Díaz C, Párraga Sánchez JM, Gamez-Leyva G, Casado Naranjo I. Diferencias de género en la calidad de vida a largo plazo tras un ictus: influencia del estado funcional y el estado de ánimo. Neurología. 2020;35:470–478.