We present our experience with the diagnosis and treatment of spinal angiolipomas (SAL).
MethodsWe used our database of surgical patients to gather epidemiological, clinical, diagnostic, treatment, and follow-up data from confirmed cases of SAL. Patients’ functional status was evaluated using the modified Japanese Orthopaedic Association (mJOA) score for thoracic myelopathy.
ResultsWe included 7 patients with ages ranging between 42 and 63 years; 4 were women. Lesions in all patients were located in the thoracic epidural space; in 2 cases, lesions extended outside the spinal canal. The most frequent form of presentation was pain combined with progressive myelopathy; patients scored 5 to 9 points on the mJOA scale. Radiological findings varied; this variability clearly depended on the proportion of tumour components (cellular variant in one case, predominantly angiomatous in another, and myxoid in yet another case). Four cases displayed radiological signs of bone involvement. Surgery resulted in excellent mJOA scores except in one case (mJOA score of 10); no recurrences were detected during follow-up (periods ranging from 1 to 5 years).
ConclusionsExtradural SAL can present with highly variable radiological and clinical features. Surgery must be tailored to each individual situation according to tumour extension; in some cases, it may include spinal reconstruction. Surgery results in excellent outcomes regardless of preoperative functional status and it is associated with low recurrence rates, even in case of incomplete resection.
Presentamos nuestra experiencia en el manejo diagnóstico y terapéutico de los angiolipomas espinales.
MétodosHemos realizado una revisión en nuestra base de datos quirúrgica correspondiente al diagnóstico patológico de angiolipoma, recogiendo las variables epidemiológicas, clínicas, diagnósticas, terapéuticas y de seguimiento de cada caso. Para la valoración funcional de los pacientes se utilizó la escala de mielopatía modificada de la Asociación Japonesa de Ortopedia (EAJO).
ResultadosObtuvimos un total de 7 casos, con edades comprendidas entre los 42 y 63 años; 4 eran mujeres. Todas las lesiones se localizaron en el espacio epidural torácico, con extensión extrarraquídea en 2 casos. La presentación más frecuente fue la combinación de dolor y mielopatía progresiva, con una puntuación entre 5 y 9 en la EAJO. Los hallazgos radiológicos fueron variables, claramente influenciados por la proporción de los componentes tumorales, identificándose un caso de variante celular, uno de predominio angiomatoso y otro mixoide. Cuatro estudios evidenciaban signos de afectación ósea. Tras el tratamiento quirúrgico se registraron puntuaciones óptimas en la EAJO, salvo en un caso (puntuación de 10 en la EAJO), sin evidenciarse recurrencias tras un periodo de seguimiento que varió entre uno y 5 años.
ConclusionesLos angiolipomas epidurales pueden dar lugar a manifestaciones clínicas y radiológicas muy variables. Su tratamiento quirúrgico debe diseñarse de acuerdo a la extensión de la tumoración, incluyendo en ocasiones un procedimiento reconstructivo espinal, y se traduce en resultados excelentes con independencia de la situación clínica previa. La posibilidad de recurrencia es baja, incluso en caso de resección incompleta.
Angiolipomas (AL) are benign tumours composed of mature adipose cells and abnormal vascularisations, and most frequently affect subcutaneous tissue of the trunk and limbs.1 Although the first descriptions of spinal epidural involvement date from the first half of the 19th century, fewer than 200 cases have been published in the literature.2 This fact, together with the great heterogeneity of clinical and radiological characteristics, makes the condition a diagnostic challenge. We present a series of cases of spinal AL (SAL) treated at our department and analyse the findings based on the relevant scientific literature published to date.
Patients and methodsWe performed a retrospective search on our hospital's electronic database for those cases with an unequivocal pathological diagnosis of SAL. We collected data regarding epidemiology, clinical manifestation, radiological diagnosis, surgical treatment, pathological study findings, and follow-up. Functional status was assessed before and after the procedure with the modified Japanese Orthopaedic Association Scale (mJOA) for thoracic spine disorder, with a minimum score of 0 (disability) and a maximum of 11 (normal function).3
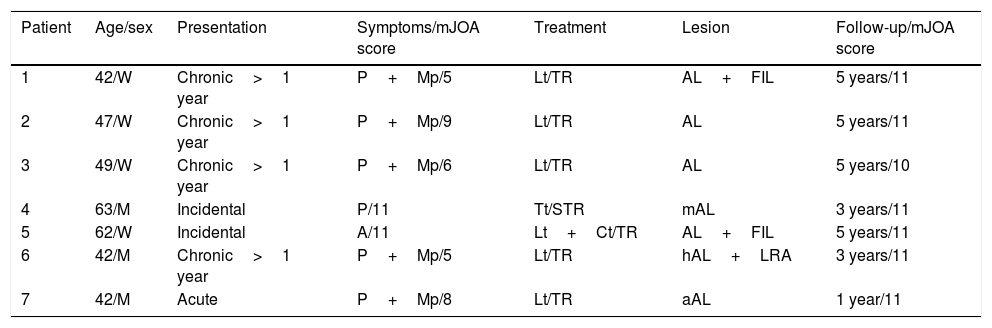
ResultsWe identified a total of 7 patients, whose clinical and radiological data are shown in Tables 1 and 2, respectively. The oldest case dates from 1994. Ages ranged between 42 and 63 years; 4 patients were women. The most frequent form of presentation was mechanical pain with or without radicular radiation (6 cases), followed by signs and symptoms of spinal compression (4 cases). The latter 4 cases developed progressively (in 2 cases for several years), with mJOA scores ranging from 5 to 9. One patient experienced sudden clinical onset following a traffic accident (case 7). In another case, the lesion was identified incidentally in a radiological study performed due to chronic respiratory failure (case 4). Lastly, one AL was detected during tumour staging in a cancer patient (case 5).
Clinical characteristics of our series of epidural angiolipomas.
| Patient | Age/sex | Presentation | Symptoms/mJOA score | Treatment | Lesion | Follow-up/mJOA score |
|---|---|---|---|---|---|---|
| 1 | 42/W | Chronic>1 year | P+Mp/5 | Lt/TR | AL+FIL | 5 years/11 |
| 2 | 47/W | Chronic>1 year | P+Mp/9 | Lt/TR | AL | 5 years/11 |
| 3 | 49/W | Chronic>1 year | P+Mp/6 | Lt/TR | AL | 5 years/10 |
| 4 | 63/M | Incidental | P/11 | Tt/STR | mAL | 3 years/11 |
| 5 | 62/W | Incidental | A/11 | Lt+Ct/TR | AL+FIL | 5 years/11 |
| 6 | 42/M | Chronic>1 year | P+Mp/5 | Lt/TR | hAL+LRA | 3 years/11 |
| 7 | 42/M | Acute | P+Mp/8 | Lt/TR | aAL | 1 year/11 |
A: asymptomatic; aAL: angiolipoma with prominent angiomatous areas; AL: angiolipoma; Ct: costotransversectomy; hAL: hypercellular angiolipoma; LFI: laminar focal infiltration; LRA: laminar reactive areas; Lt: laminectomy; M: man; mAL: angiolipoma with myxoid areas; mJOA: modified Japanese Orthopaedic Association Scale on dorsal myelopathy; Mp: myelopathy; P: pain; STR: subtotal resection; TR: total resection; Tt: thoracotomy; W: woman.
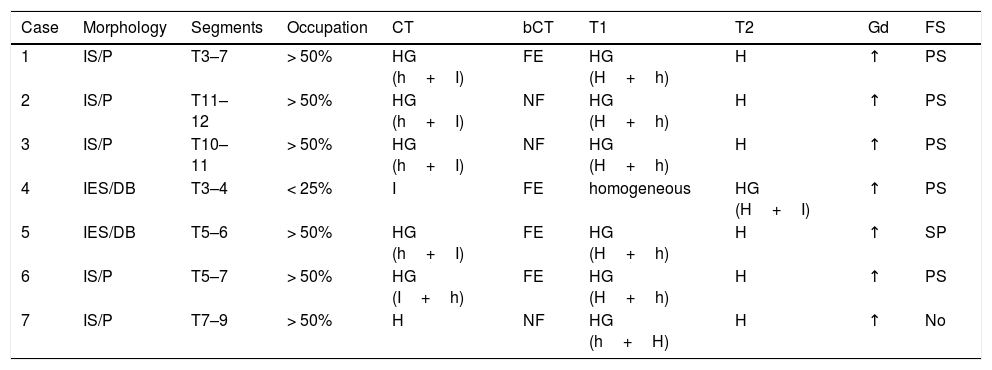
Radiological characteristics of our series of epidural angiolipomas.
| Case | Morphology | Segments | Occupation | CT | bCT | T1 | T2 | Gd | FS |
|---|---|---|---|---|---|---|---|---|---|
| 1 | IS/P | T3–7 | > 50% | HG (h+I) | FE | HG (H+h) | H | ↑ | PS |
| 2 | IS/P | T11–12 | > 50% | HG (h+I) | NF | HG (H+h) | H | ↑ | PS |
| 3 | IS/P | T10–11 | > 50% | HG (h+I) | NF | HG (H+h) | H | ↑ | PS |
| 4 | IES/DB | T3–4 | < 25% | I | FE | homogeneous | HG (H+I) | ↑ | PS |
| 5 | IES/DB | T5–6 | > 50% | HG (h+I) | FE | HG (H+h) | H | ↑ | SP |
| 6 | IS/P | T5–7 | > 50% | HG (I+h) | FE | HG (H+h) | H | ↑ | PS |
| 7 | IS/P | T7–9 | > 50% | H | NF | HG (h+H) | H | ↑ | No |
↑: intense paramagnetic contrast uptake; bCT: CT scan with bone window; DB: dumbbell; FE: focal erosion; FS: fat suppression; h: hypo (intense/dense); H: hyper (intense/dense); HG: heterogeneous; I: iso (intense/dense); IES: intra-extraspinal; IS: intraspinal; NF: no findings indicating bone involvement; No: no suppression; Occupation: percentage of occupation of the spinal canal; P: posterior; PL: posterolateral; PS: partial suppression.
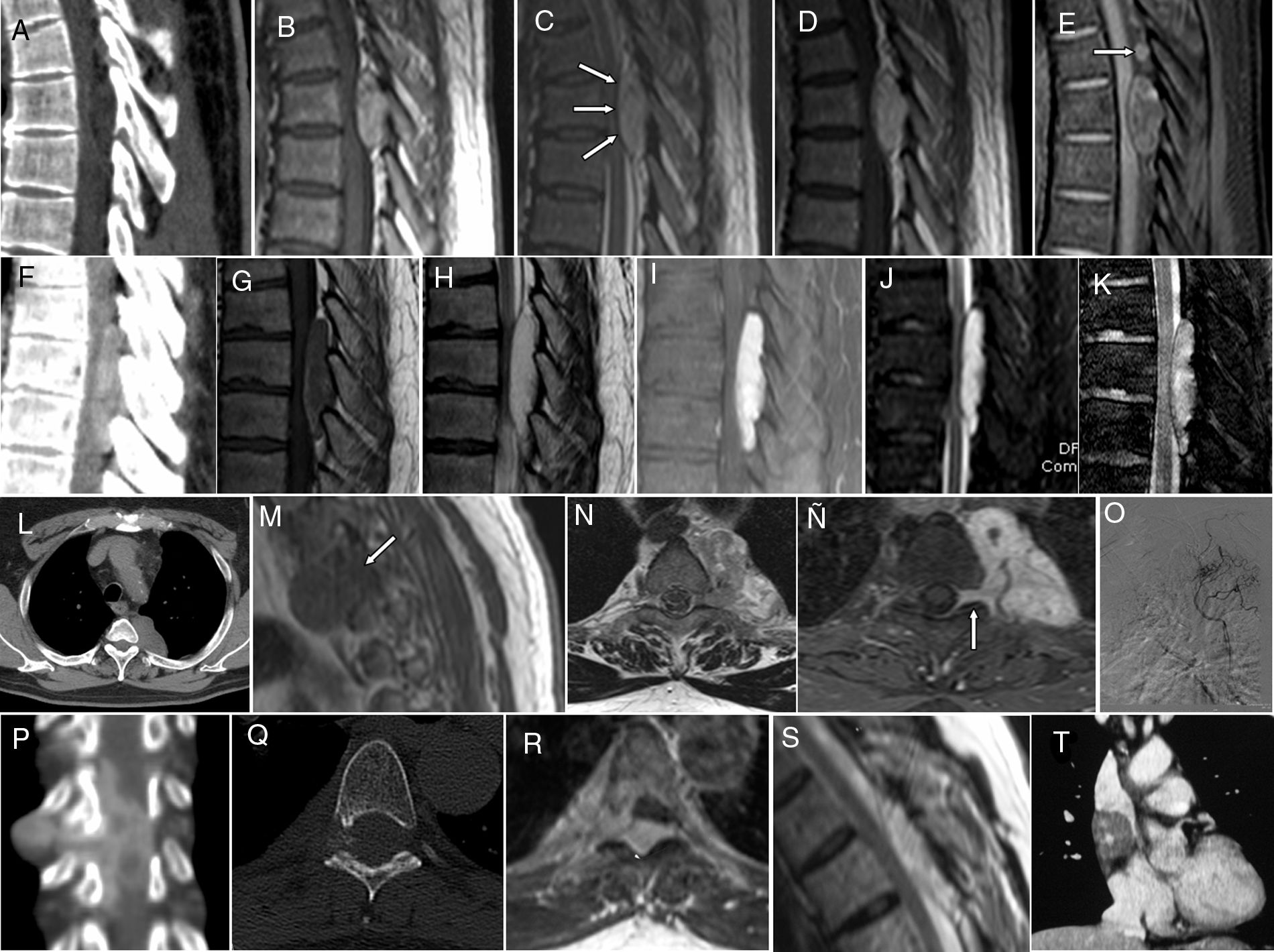
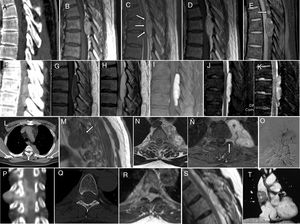
All patients underwent CT and MRI studies (Table 2, Fig. 1A-T). Lesions were identified in the epidural compartment in the thoracic region in all cases, with extension ranging from 2 to 5 levels. Five lesions exclusively affected the spinal canal and presented a fusiform morphology, whereas dumbbell tumours were detected in patients 4 and 5; in the latter case, the tumour was of irregular and polylobulated morphology. Additional angiomas were identified in 3 patients, including multiple vertebral angiomas (cases 4 and 7), and a cavernous angioma in the mediastinum (case 5).
Spinal epidural AL: diagnostic imaging gallery. Case 6: (A) sagittal CT reconstruction with soft-tissue window showing a well-delimited, spindle-shaped, heterogeneous lesion with predominantly fat density occupying the posterior portion of the spinal canal, with remodelling of the vertebral lamina. The lesion appears heterogeneous and predominantly hyperintense on T1- (B) and T2-weighted MRI sequences (C); it compresses the spinal cord without invasion of the dural barrier (arrows in C) and shows intense enhancement (D) as well as suppression areas on the SPIR sequence (E), revealing an angiomatous peripheral nodular portion (arrow). Case 7: lesion showing increased uptake on CT (F), hypointense on T1-weighted sequences with peripheral areas with stronger signal (G), hyperintense on T2-weighted sequences (H), with homogeneous contrast uptake on SPIR with contrast (I), hyperintensity on STIR (J), and no signs of bleeding on the gradient echo sequence (K). Case 4: axial chest CT slice (L) showing a well-delimited, homogeneous lesion occupying the left costovertebral mediastinal region. The lesion is isointense on T1-weighted sequences; heterogeneous, isohyperintense on T2-weighted sequences (N), with intense and homogeneous contrast uptake on T1-weighted sequences with fat suppression (Ñ), and extending to the ipsilateral foraminal region (arrows in M and Ñ). Angiography after selective canalisation of a left superior intercostal trunk, with vessels from the superior branch irrigating the neoplasm (O). Case 5: Spinal CT image with coronal reconstruction showing a heterogeneous lesion with irregular contours and heterogeneous contrast uptake (P); it presents posterior, foraminal, and paravertebral epidural components, with signs of remodelling of the right intervertebral foramen in the axial CT scan with bone window (Q). The lesion is hyperintense on both T1-weighted (R) and T2-weighted (S) sequences. CT with coronal reconstruction revealing coexistence of a lesion in the middle mediastinum, which was finally diagnosed as cavernous angioma (T).
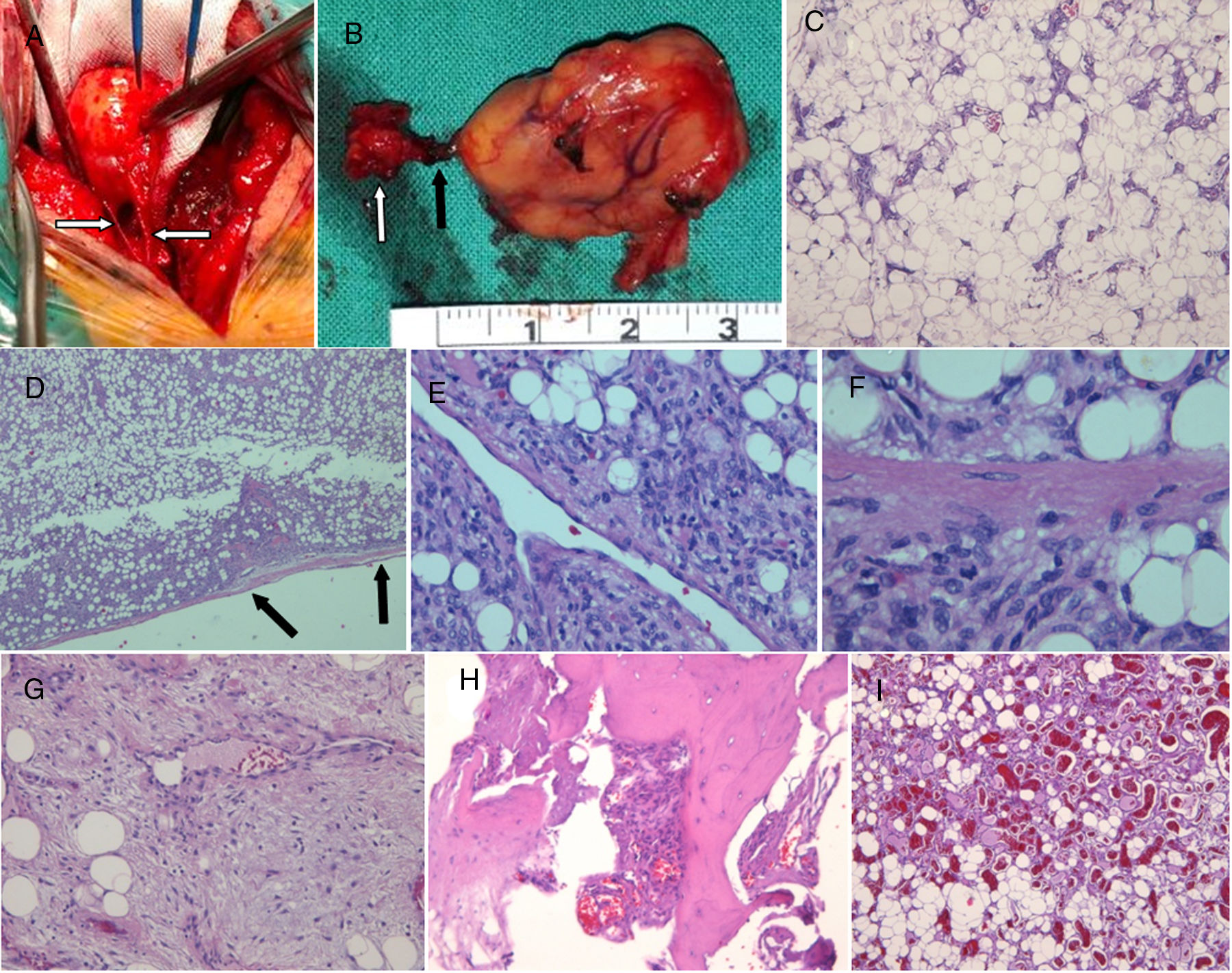
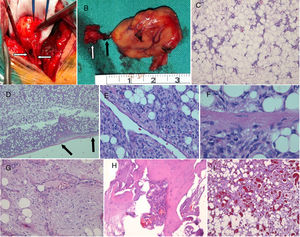
From an anatomopathological viewpoint, we identified 4 classic ALs, one myxoid variant, one cellular variant, and another with predominance of angiomatous areas; involvement of the laminae was observed in 3 cases, with severe cortical erosion and occupation of the cavity caused by the tumour (Table 1, Fig. 2A–I).
Spinal epidural AL: pathological gallery. (A) Intraoperative photograph (case 6) showing a well delimited, yellowish-red, encapsulated, slightly lobulated lesion of elastic consistency, resectable from the dural surface, supplied by numerous vascular channels from the epidural space (arrows). (B) It is connected to another nodular component (white arrow) by a vascular formation (black arrow). (C) Classic angiolipoma with proliferation of mature adipocytes and thin-walled, capillary-sized vessels (H-E×4). (D) Angiolipoma delimited by a thin conjunctive capsule (arrows) (case 6, H-E×4), with areas of hypercellularity (E) (case 6, H-E×20) composed of spindle-shaped cells which were positive for endotelial markers. (F) Identification of mitosis in the area of hypercellularity (case 6, H-E×40). (G) Angiolipoma with myxoid areas, rich in extracellular matrix (case 4, H-E×10). (H) Focal infiltration of spongy bone (case 5, H-E×10). (I) Angiolipoma with prominent angiomatous areas and frequent thrombi (case 7, H-E×4).
Most tumours were treated surgically with laminectomy, complemented by costotransversectomy in case 5, achieving complete resection with microsurgical techniques. As an exception, case 4 underwent a subtotal resection by thoracotomy; a tumour remnant smaller than 1cm was detected in the foramen in the follow-up imaging study. In all cases, lesions were macroscopically described as well-delimited, encapsulated processes, which could be separated by blunt dissection from the adjacent tissues, with multiple superficial vascular channels coming from the epidural space. No patient required spinal stabilisation.
Follow-up times ranged from 1 to 5 years, with no patient displaying residual changes in spinal signal, relapses, or tumour regrowth. No patient developed clinical or radiological signs of spinal instability. All patients showed significant clinical improvement, scoring 11 on the mJOA, with the exception of case 3, who presented persistent urethral sphincter dysfunction.
DiscussionAngiolipomas are infrequent, representing 0.14% to 1.2% of spinal tumours and 2% to 3% of epidural spinal tumours.1 Our series includes a total of 7 cases from the past 22 years, which demonstrates the low incidence of this neoplasm in our setting. The AL topography observed in our patients attests to its preference for the epidural space, mainly in the thoracic region; cases have been described at all spinal levels.2,4,5 In 5 patients, lesions were limited to the spinal canal, involving the posterior epidural space (as in slightly below 90% of cases described in the literature), fusiform morphology and variable length; cases have been described of lesions affecting up to 8 levels.5 Less frequently, AL may also occupy intervertebral foramina and extend beyond the spinal canal, as in case 5, even developing as tumour masses of predominantly extraspinal extension, as in case 4; complicating differential diagnosis with regards to other epidural expansive processes.2
The WHO classification categorises AL as a subgroup of lipomas composed of a variable proportion of mature adipocytes and capillary-sized vessels, with presence of thrombi and interstitial fibrosis in long-term lesions.6 Both cellular components are characterised by the absence of mitosis, atypia, or pleomorphism.6 Differential diagnosis is usually easy to establish, except in the case of cellular AL, which should be distinguished from spindle-cell angiosarcoma and Kaposi sarcoma.
The origin of AL has historically been subject to debate. Depending on their microscopic composition, they have been considered to be tumours developed from mesenchymal cells, hamartomatous lesions, congenital malformations, and haemangiomas with insertions of epidural adipose tissue.4 The latter hypothesis is supported by some authors who have observed larger vessels (and even cavernomas7) in epidural AL than in subcutaneous AL; some authors have even suggested a change in nomenclature to vascular lipoma.8 This consideration is related to the controversy regarding infiltrating AL,9–11 a term initially used to refer to mainly or entirely nonencapsulated ALs infiltrating adjacent tissues, which tend to recur if surgical treatment does not include wide resection margins.9 In the case of epidural AL, infiltrating ALs are usually located anterior or anterolateral to the thecal sac, with involvement of one or several vertebral bodies and pedicles; in exceptional cases, they may be located posteriorly, which may be interpreted as an extension of an angiomatous lesion of vertebral origin.12 However, other authors propose that the bone damage may be caused by compression, with clear boundaries free of tumour infiltration,3 and that the term “infiltrating” should only be used in those exceptional cases of AL invading the dura mater.13
Although it has often been attributed to Berenbruch, the first case of SAL was described in the first half of the 19th century and is an excellent description of the natural progression of these tumours. The patient was a 24-year-old woman who developed a slowly progressive functional disability of the lower limbs over a period of 5 years, which progressed to complete spinal cord lesion and death due to associated complications, including pressure ulcers.1,4,14 The autopsy study revealed an adipose lesion under the laminae of the tenth to the twelfth thoracic vertebrae, which did not invade the dura mater; the compressed segment of spinal cord was completely atrophic.14 We now know that epidural AL mainly affects middle-aged adults, especially those in the fifth decade of life, with a slight preference for women2; this is reflected in our series. Symptoms usually comprise slowly progressive neurological dysfunction; cases have been reported of up to 17 years of progression.2,5 Relapsing-remitting clinical courses have been described and associated with such dynamic changes in the vascular component of the tumour as increased epidural venous pressure, brain sparing, the Valsalva manoeuvre (pregnancy, delivery), subclavian steal syndrome, spinal venous return impairment or thrombosis, hormonal changes (steroids), and obesity.2,3,5,15 Manifestation may also be acute, especially in cases of intratumoural haemorrhagic lesions, which seem to occur predominantly in AL of the neck located close to the C6 segment.16 One of our patients presented acute symptoms after multiple trauma, with no evidence of tumour bleeding. Lastly, these neoplasms may also be an incidental finding during a systemic study performed due to another pathological process, as described in cases 4 and 5.
The peculiarities of AL in neuroimaging studies are a reflection of the previously described pathological characteristics. Simple radiography studies may reveal signs of bone involvement, including pedicular erosion, foraminal expansion, or trabeculation of the vertebral body.12 Spinal CT scan is more sensitive for detecting these changes, but may be non-specific when defining soft tissues due to the variability in the proportion of tumoural components and the possible presence of such intralesional events as calcification and/or haemorrhage.2 This consideration is also applicable when interpreting MRI findings.3,15,17 Adipose tissue emits a high-intensity signal in both T1- and T2-weighted sequences, with loss of signal in fat suppression images, mainly STIR and SPIR sequences.3,15 SPIR is a hybrid technique including a selective radiofrequency pulse for adipose tissue and spoiler gradient pulse, together with suppression of the residual fat magnetisation through similar inversion recovery to that of STIR, enabling enhancement of the suppressed areas with regard to those displaying gadolinium uptake (Fig. 1E). These sequences are especially useful for diagnosing AL, since the angiomatous component is hypointense and isointense with regard to the spinal cord in T1-weighted sequences, and hyperintense in T2-weighted sequences, with intense enhancement after administration of a paramagnetic contrast (Fig. 1).3,15 ALs are also characterised by the absence of vascular flow voids, due to the lack of well-developed vessels.17 Dura mater integrity is optimally assessed in T2-weighted sagittal slices showing a low-intensity line between the tumour and the cerebrospinal fluid of the subarachnoid space or the spinal cord, depending on the degree of occupation of the spinal canal (Fig. 1). There have been several attempts to systematise the radiological characteristics of AL; Hu et al.15 classify ALs into type 1 (with a predominant fat component and fusiform morphology) and type 2 (predominant vascular component, located in the central part of the tumour). Si et al.3 propose distinguishing type I, or intraspinal (IA without lipomatosis and IB with peripheral lipomatosis), and type II, or dumbbell-shaped. However, we consider that these classifications lack prognostic value and present serious limitations when including the different radiological forms of presentation of AL, as reflected in our series (Table 2 and Fig. 1). Rarely performed angiographic studies usually reveal arterial supply from branches of the intercostal arteries, as in our case 4 (Fig. 1), with preoperative embolisation not constituting a significant advantage during the procedure as vascular supplies are usually well controlled.2
Radiological differential diagnosis of AL composed predominantly of fatty tissue includes lipoma and lipomatosis, with enhancement after paramagnetic contrast administration and signal in fat suppression sequences being particularly significant, as they may represent a small vascular component. Furthermore, AL predominantly composed of the vascular component or located in the central part of the tumour may be mistaken for angiomas or neurogenic tumours, since the peripheral fat component may be interpreted as epidural fat compressed by the tumour. Depending on the proportions of the different tumour components, their variable morphology, the presence or absence of complications (bleeding), and the detection of bone involvement, we may observe a greatly heterogeneous radiological presentation which, depending on the clinical context (especially cancer or trauma), may represent a considerable diagnostic challenge.
Surgery is the treatment of choice for epidural ALs.5 Given their typical location, they can usually be treated with laminectomy. During the procedure, they are described as highly vascularised, yellowish-red lesions with a tendency to bleed (Fig. 2A and B). ALs are easily resected away from adjacent tissues, although they present multiple attachment points to the epidural vessels supplying them, usually enabling resection of the AL as a whole or in fragments, in the case of larger lesions. ALs with thoracic extraforaminal extension may be approached through costotransversectomy. The approach is anterolateral when the main tumour component is extraspinal and in infiltrating tumours with extensive involvement of the vertebral body. The need for spinal stabilisation will depend on the degree of bone and ligament resection required for the approach and resection; it is particularly recommended in the case of corpectomy, combined anterior and posterior approaches, and in procedures involving the junctions and areas of greater mobility.2 As previously mentioned, thoracic laminectomy is the most frequent clinical context; pedicle screw fixation or laminoplasty are reserved for more extensive approaches, given the biomechanical stability of this spinal segment. In fact, there were no cases of kyphosis in our series, even in more extensive posterior thoracic approaches.
ALs are tumours with a very favourable prognosis after surgical treatment, with satisfactory functional recovery achieved in almost all cases, regardless of the initial degree of involvement and the time to surgery.2 Furthermore, the associated recurrence rate is near zero, regardless of the degree of resection and the histological variant of the tumour.5,12 The most important prognostic factor is the speed of onset of the neurological deficit, especially in those cases with sudden onset of severe neurological deficit due to intratumoural bleeding,18 in which emergency treatment should be considered. Although cases of AL treated with radiotherapy have been reported, this type of therapy is currently considered ineffective in treating this entity.2,5
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Carrasco Moro R, Gutiérrez Cierco JA, Martínez San Millán JS, Pian H, Martínez Rodrigo MA. Spinal extradural angiolipomas: 7 new cases and review of the literature. Neurología. 2019;34:98–104.
Part of this study was presented in poster format by Dr Gutiérrez Cierco at the annual meeting of the European Association of Neurosurgical Societies, held in Madrid, 18 to 21 October 2015.