Status epilepticus is an important cause of pediatric neurological emergency. Immediate treatment is essential to prevent definitive neurological damage. Several antiepileptic drugs are available for the management of status epilepticus.
MethodsRetrospective study of patients admitted at the emergency department of a tertiary hospital for 5 years (2014–2019). We analyzed the compliance to the treatment guidelines for pediatric status epilepticus.
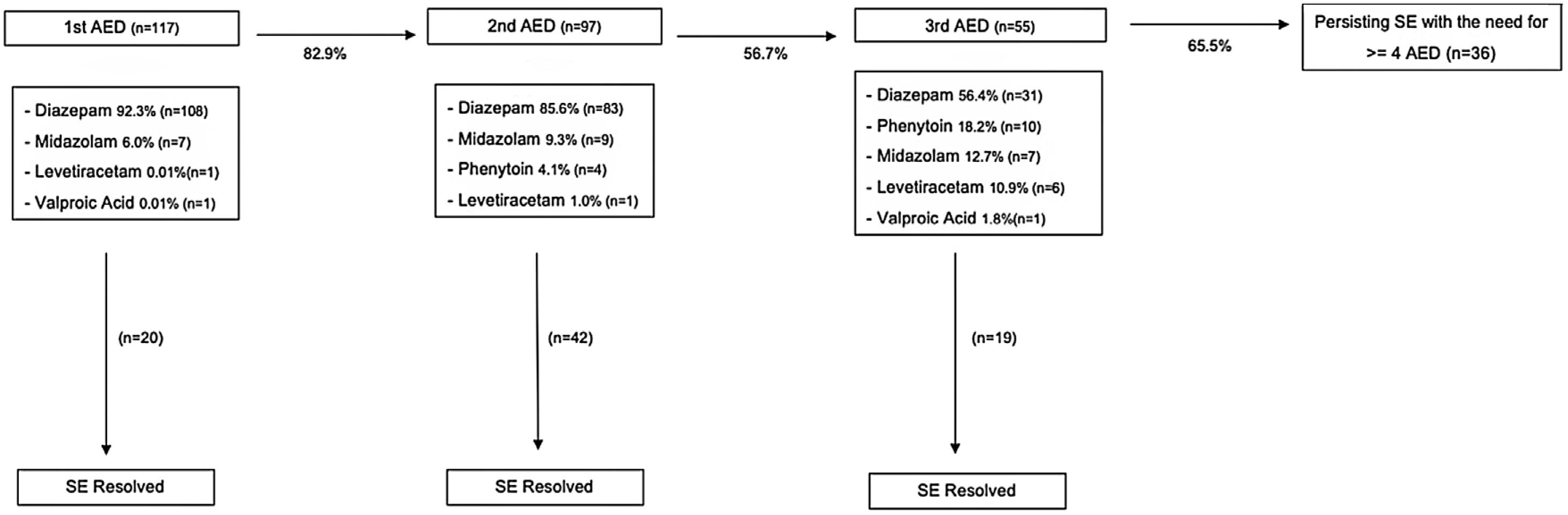
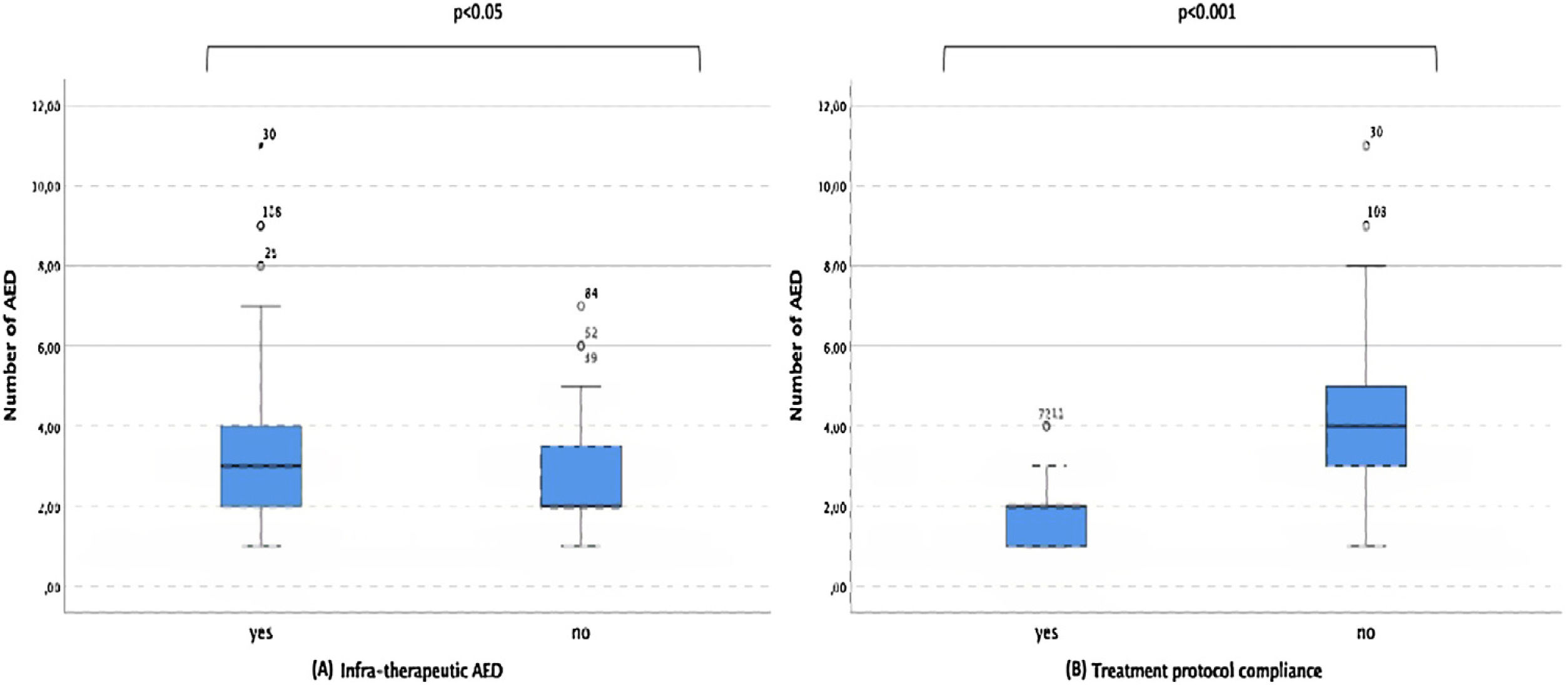
ResultsOne hundred and seventeen admissions were identified, 23.9% of these were febrile status epilepticus. Among the other cases, the most frequent cause was genetic (22.2%). The majority were convulsive status epilepticus (93.1%), 58.7% of which were generalized tonic–clonic seizures. Benzodiazepines were the most used first and second line drug (98.2% and 94.8%). The most frequent third drug used was diazepam (56.4%) followed by phenytoin (18.2%). An infra-therapeutic antiepileptic drug dose was given in 48.7% of cases. 49.6% presented with a prolonged status epilepticus and 6.8% needed intensive care. Incorrect sequence of drugs and infra-therapeutic doses were associated with prolonged status (p<0.001 and p<0.05) and an increased number of antiepileptic drugs used (p<0.001 and p<0.05).
ConclusionsBenzodiazepines were the most frequently first and second line drugs used for status epilepticus management. Surprisingly, the most frequently third line drugs used were also benzodiazepines. These findings were partially explained by the misuse of infra-therapeutic doses of these drugs. Noncompliance with the implemented guidelines was associated with unfavorable outcomes.
El estatus epiléptico es una causa importante de urgencia neurológica pediátrica. El tratamiento inmediato es fundamental para prevenir el daño neurológico definitivo. Hay varios fármacos antiepilépticos disponibles para el tratamiento del estatus epiléptico.
MétodoEstudio retrospectivo de pacientes ingresados en el servicio de urgencia de un hospital terciario durante 5 años (2014-2019). Analizamos el cumplimiento de las guías de tratamiento del estatus epiléptico pediátrico.
ResultadosSe identificaron 117 ingresos, el 23,9% de estos fueron estatus epilépticos febril. Entre los demás casos, la causa más frecuente fue genética (22,2%). La mayoría fueron estatus epiléptico convulsivos (93,1%), de los cuales el 58,7% fueron convulsiones tónico-clónicas generalizadas. Las benzodiazepinas fueron el fármaco de primera y segunda línea más utilizado (98,2% y 94,8%). El tercer fármaco más utilizado fue el diazepam (56,4%) seguido de la fenitoína (18,2%). Se administró una dosis de fármaco antiepiléptico infraterapéutico en el 48,7% de los casos. El 49,6% presentó un estatus epiléptico prolongado y el 6,8% necesitó cuidados intensivos. La secuencia incorrecta de fármacos y dosis infraterapéuticas se asociaron con un estatus prolongado (p<0,001 y p<0,05) y un mayor número de fármacos antiepilépticos utilizados (p<0,001 y p<0,05).
ConclusionesLas benzodiazepinas fueron los fármacos de primera y segunda línea más utilizados en el tratamiento del estatus epiléptico. Sorprendentemente, los fármacos de tercera línea más empleados también fueron las benzodiazepinas. Estos hallazgos se explicaron en parte por el uso indebido de dosis infraterapéuticas de estos fármacos. El incumplimiento de las directrices implementadas se asoció con resultados desfavorables.
Status epilepticus (SE) is an important cause of pediatric neurological emergency with an incidence of 17–23/100,000 children per year.1 This condition is considered to be the most extreme form of seizure, caused by either a failure of seizure terminating mechanisms to act or an enabling of initiation mechanisms which lead to a prolonged convulsive event.2 The latest International League Against Epilepsy (ILAE)’s tasks force consensus recommends that treatment should be started at 5min of a tonic–clonic seizure: T(1). At this time the seizure is likely to be prolonged leading to a continuous seizure activity. T(2), at 30minutes of seizure, is defined as the time from which there seem to be long term neurological consequences.3 Therefore, prompt management of these patients is important to prevent neurological damage. The optimal treatment for these patients is under study and there is a lack of controlled prospective studies comparing various antiepileptic agents’ efficacy. Based on the main diagnostic and therapeutic procedures in portuguese Neuropediatric units, Portuguese Society of Pediatrics (PSP) along with Portuguese Society of Neuropediatrics (PSN), have published a consensus guideline regarding treatment management in 2008.4 These have recently been updated in October 2020.5 Our aim with this study was to evaluate SE's treatment management and compliance with the guidelines.
MethodsStudy designWe carried out a retrospective study evaluating patients admitted for status epilepticus in a tertiary hospital's emergency department (Urgência Pediátrica do Porto) between January 2014 and December 2019. The study was approved by the Ethics Committee of Centro Hospitalar e Universitário de São João.
ParticipantsWe identified all patients who were given an antiepileptic drug (AED) in the emergency department, with ages between one month and 18 years old. Patients were included if they had (i) a convulsive event lasting more than five minutes, with no response to the AED or (ii) multiple convulsive events lasting less than five minutes, without recovery between seizures or (iii) non convulsive seizures lasting more than 10min, with no response to the AED. Patients were excluded if they were given an AED for a non-epileptic event. This study did not include patients who had a direct admission to the intensive care unit (ICU) or those who had a SE event during hospitalization.
OutcomesClinical data was collected from electronical clinical records. Our primary outcome was the national PSP/PSN pediatric status epilepticus guideline compliance. Secondary outcomes were: prolonged SE (defined as events lasting longer than 30min) and admission to the ICU.
Statistical analysisStatistical analysis was carried out using IBM SPSS, version 26.0 (IBM Corp., Armonk, New York, USA). X2-test was performed for categorical variables. Continuous variables were expressed as mean±interquartil range and compared using Mann–whitney test. A p value<0.05 was considered statistically significant.
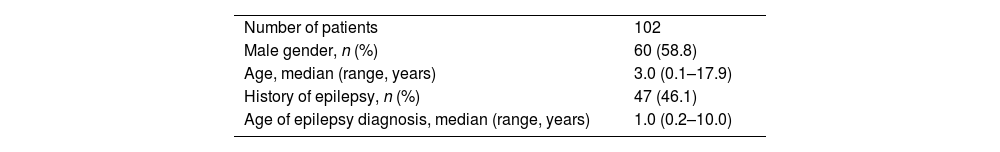
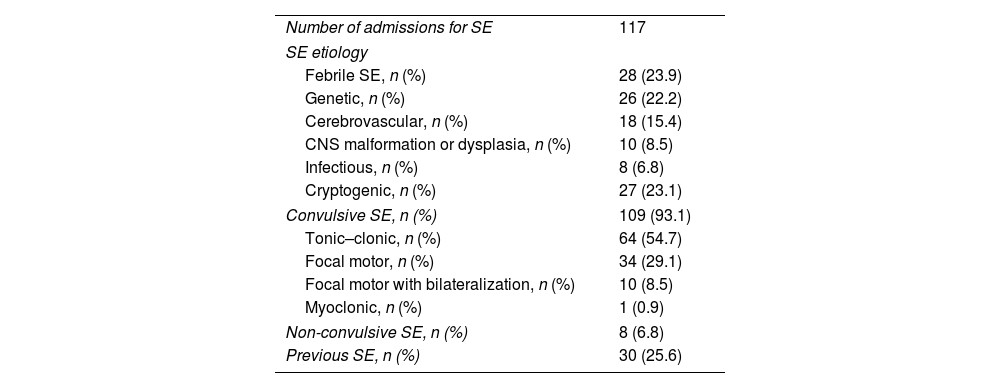
ResultsSample characteristicsA total of 117 admissions to the pediatric emergency for SE were identified, corresponding to 102 different patients. Thirteen patients had two admissions due to SE and one patient had three admissions for SE. 60% were boys with a median age of three years old (ranging from one month to 17 years). A previous diagnosis of epilepsy was reported in 46.1% of the admitted patients (Table 1). From the 117 admissions, 25.6% had a previous episode of SE (Table 2). We identified 28 cases of febrile SE. Among the non-febrile SE, the most common etiology was genetic (22.2%), followed by cerebrovascular (15.4%). Most of the SE were convulsive (93.1%), presenting frequently as a tonic–clonic seizure (58.7%). Only 6.8% were clinically classified as non-convulsive SE (Table 2).
Demographic and clinical characteristics of the 102 patients admitted for status epilepticus to the emergency department.
| Number of patients | 102 |
| Male gender, n (%) | 60 (58.8) |
| Age, median (range, years) | 3.0 (0.1–17.9) |
| History of epilepsy, n (%) | 47 (46.1) |
| Age of epilepsy diagnosis, median (range, years) | 1.0 (0.2–10.0) |
Characterization of the status epilepticus admissions to the emergency department.
| Number of admissions for SE | 117 |
| SE etiology | |
| Febrile SE, n (%) | 28 (23.9) |
| Genetic, n (%) | 26 (22.2) |
| Cerebrovascular, n (%) | 18 (15.4) |
| CNS malformation or dysplasia, n (%) | 10 (8.5) |
| Infectious, n (%) | 8 (6.8) |
| Cryptogenic, n (%) | 27 (23.1) |
| Convulsive SE, n (%) | 109 (93.1) |
| Tonic–clonic, n (%) | 64 (54.7) |
| Focal motor, n (%) | 34 (29.1) |
| Focal motor with bilateralization, n (%) | 10 (8.5) |
| Myoclonic, n (%) | 1 (0.9) |
| Non-convulsive SE, n (%) | 8 (6.8) |
| Previous SE, n (%) | 30 (25.6) |
The 117 admissions received a first AED for the management of SE, the majority of which received a BZD (98.2%). A second AED was administered in 82.9% of the SE (diazepam in 85.6%). A third AED was needed in 56.7%. In this group, diazepam was also the most frequently used drug (56.4%) (Fig. 1). Thirty-six patients needed four or more drugs for seizures control. When analysing the protocol compliance, we observed that in 54 admissions (46.2%) treatment guidelines were not followed because of incorrect drug sequence. Furthermore, in 48.7% of the cases, at least one infra-therapeutic dose of an AED was administered. Regarding our secondary outcomes, 49.6% of cases presented with a prolonged SE lasting more than 30min. 6.8% were transferred to the ICU due to need of ventilatory support. There were no deaths documented.
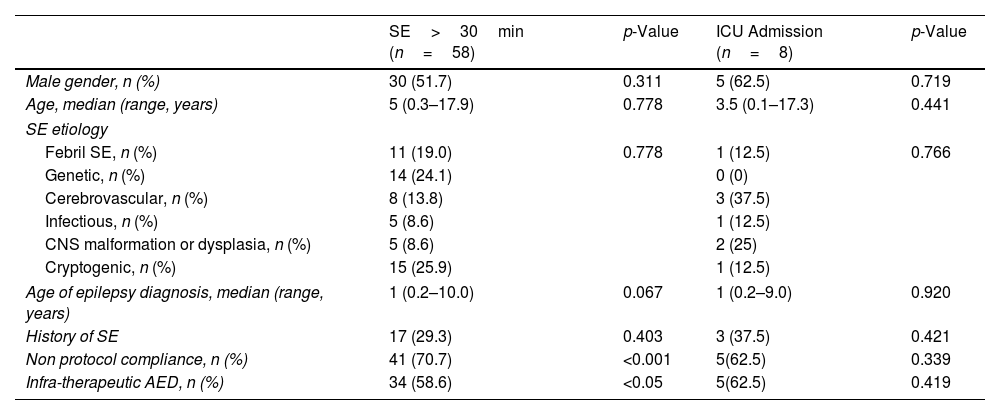
Outcome analysisStatus epilepticus episodes in which AED sequence guidelines were not followed were associated with a prolonged SE (p<0.001) (Table 3). These patients also needed a higher number of AED for SE control (p<0.001) (Fig. 2). In addition, patients who were given infra-therapeutic doses of AED had a higher frequency of prolonged SE and needed a higher number of AED for SE control (p=0.034 and p=0.004). In most patients who were admitted to the intensive care unit, AED sequence guidelines were not followed and infra-therapeutic AED doses were used, although there was no statistically significant difference (p=0.339 and p=0.419). Prolonged SE and intensive care admission did not correlate with gender; age of SE presentation; age of epilepsy diagnosis; history of SE or SE etiology.
Univariate analysis of factors related to SE>30min and ICU Admission, p<0.05 statistically significant.
| SE>30min (n=58) | p-Value | ICU Admission (n=8) | p-Value | |
|---|---|---|---|---|
| Male gender, n (%) | 30 (51.7) | 0.311 | 5 (62.5) | 0.719 |
| Age, median (range, years) | 5 (0.3–17.9) | 0.778 | 3.5 (0.1–17.3) | 0.441 |
| SE etiology | ||||
| Febril SE, n (%) | 11 (19.0) | 0.778 | 1 (12.5) | 0.766 |
| Genetic, n (%) | 14 (24.1) | 0 (0) | ||
| Cerebrovascular, n (%) | 8 (13.8) | 3 (37.5) | ||
| Infectious, n (%) | 5 (8.6) | 1 (12.5) | ||
| CNS malformation or dysplasia, n (%) | 5 (8.6) | 2 (25) | ||
| Cryptogenic, n (%) | 15 (25.9) | 1 (12.5) | ||
| Age of epilepsy diagnosis, median (range, years) | 1 (0.2–10.0) | 0.067 | 1 (0.2–9.0) | 0.920 |
| History of SE | 17 (29.3) | 0.403 | 3 (37.5) | 0.421 |
| Non protocol compliance, n (%) | 41 (70.7) | <0.001 | 5(62.5) | 0.339 |
| Infra-therapeutic AED, n (%) | 34 (58.6) | <0.05 | 5(62.5) | 0.419 |
In accordance with previous literature, we found that the most common underlying cause of SE was a febrile seizure. We distinguished this entity from febrile SE with an underlying cause (for example encephalitis) because of the potential difference in mortality and morbidity of these two groups.1 Furthermore, and in line with other studies, most cases of SE were convulsive, presenting as tonic–clonic seizures and occurred in children with no previous history of SE.6,7
Our study showed that the combination of protocol noncompliance and infra-therapeutic drug doses was associated with a higher frequency of prolonged SE and the need for a higher number of AED to SE control. In fact, we found that in nearly half of our patients the established treatment protocol for SE was not followed, due to incorrect sequence of the AED used. We documented that, in accordance to the guidelines, BZD were the first and second line preferential choice. However, these drugs were also the most frequently third line treatment used, instead of escalating to another AED. In addition, 48.7% of the patients received infra-therapeutic doses of AEDs. According to these two findings, we were able to understand that the patients who received infra-therapeutic doses of BZD had a higher chance of receiving more than two trials of BZD. Previous studies have shown a pattern of BZD sub-dosing in SE. In a retrospective study, Abhishek et al. found that approximately 70% of patients received a lower than guideline recommended dose of first line treatment with a pattern of administering multiple small doses of BZD.8 Similarly, Langer and Fountain et al. found that approximately 50% of patients treated for SE were also given multiple small doses of BZD and only 11% received recommended dose treatment.9 These findings can be explained by the perceived risk of cardiorespiratory depression as a side effect of these drugs. Nevertheless, prolonged untreated SE may lead to more pronounced respiratory consequences than the ones caused by BZD administration.10 Moreover, BZD are only proven to be efficient in the initial treatment of SE. This is due to the internalization of synaptic GABA receptors which lead to a time-dependent pharmaco-resistance to BZD. In consequence, the efficacy of these drugs decreases over time, causing the need to use other AEDs.11 Correct drug sequence and dose administration seems crucial to prevent further complications.
The most used non-BZD drug was phenytoin. Levetiracetam and valproic acid have been proven to be an efficient alternative to phenytoin with fewer cardiorespiratory side effects.12,13 Nonetheless, our data shows that these drugs were still seldom used, reflecting the previous national protocols in place until 2020. The new 2020 SE guidelines recommend the use of a BZD as first and second line drugs, and the optional use of phenytoin, levetiracetam or valproic acid as third line drugs.5
This was a nonrandomized, retrospective, single-center study, with its inherent limitations. We only analyzed patients who were admitted to the emergency department leaving out patients who had direct admission to the ICU or those who had an SE episode during hospitalization. Nevertheless, we were able to analyze a large number of pediatric patients admitted in a tertiary hospital and to identify treatment approach factors that may be reviewed and corrected in the future in order to improve protocol compliance and patients’ outcomes.
ConclusionManagement of children with SE can be challenging given the need for a rapid response. The establishment and disclosure of protocols to guide clinical practice in these cases is the key to improve emergency treatment and subsequent clinical outcome.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestsThe authors declare that they have no conflict of interest.