Angiography is a technique used in the diagnosis, surgical planning, and treatment of tumours. Presurgical embolisation of the internal carotid artery is a common adjuvant therapy to the surgical resection of head and neck cancers.1 The technique is made possible by the flow compensation provided by the circle of Willis through the intracranial communicating arteries.
Contrast-induced encephalopathy is a rare but reversible complication that appears after the administration of an iodinated contrast agent; it was first described in 1970 in a patient who presented cortical blindness following cardiac catheterisation.2
We present the case of a patient with transient contrast-induced encephalopathy after embolisation of the left internal carotid artery before surgery for nasopharyngeal carcinoma.
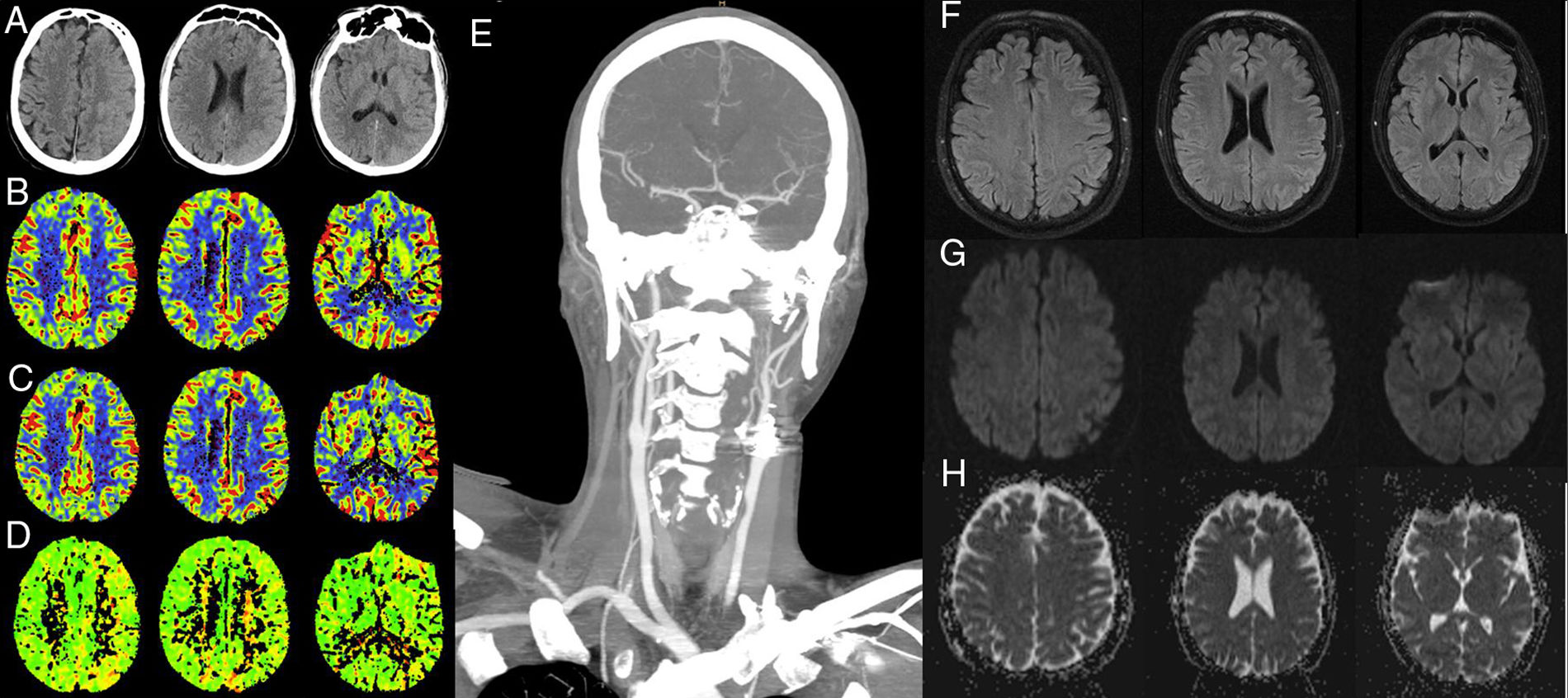
Our patient was a 41-year-old man with a history of locally relapsing squamous cell carcinoma of the nasopharynx; he had previously been treated with surgery, chemotherapy, and radiotherapy, and was admitted electively to our centre for surgical reintervention. Three months before surgery, the patient underwent an angiography-based balloon test occlusion of the carotid artery (200mL of non-ionic iodinated contrast agent were administered), which confirmed that there was sufficient flow compensation by the circle of Willis and the absence of neurological symptoms. The day before the procedure he underwent embolisation of the left internal carotid artery in 2 locations: proximally, beyond the carotid bifurcation, and distally, proximal to the ophthalmic artery (Fig. 1). For the angiography, we used 310mL of non-ionic iodinated contrast. The procedure was uneventful and the patient remained asymptomatic at all times. Renal function was preserved before and after the procedure (glomerular filtration rate >90mL/min) and his arterial blood pressure remained within normal ranges. Six hours after embolisation, the patient presented neurological signs of predominantly motor aphasia, right homonymous hemianopsia, and right facial paralysis. A blood analysis revealed no alterations and the electrocardiography showed sinus rhythm. The baseline sequence of a head CT scan using an iodinated contrast agent (50mL) revealed attenuation of sulci, suggestive of oedema, and cortical contrast uptake in the left hemisphere (Fig. 2A). CT angiography confirmed occlusion of the left internal carotid artery with excellent compensation of intracranial circulation, with perfusion sequences showing no alterations (Fig. 2B-E). In the acute phase, we started antiepileptic treatment with levetiracetam at 1000mg/12h and dexamethasone at 6mg/4h. An MRI scan performed at 24hours showed signal alterations on the FLAIR and DWI sequences in the left parietal and frontal cortex, with no restriction on the ADC map; these findings are compatible with vasogenic oedema. An electroencephalogram revealed slowing of the background rhythm in the left hemisphere. The patient improved clinically, with symptoms resolving 24hours later.
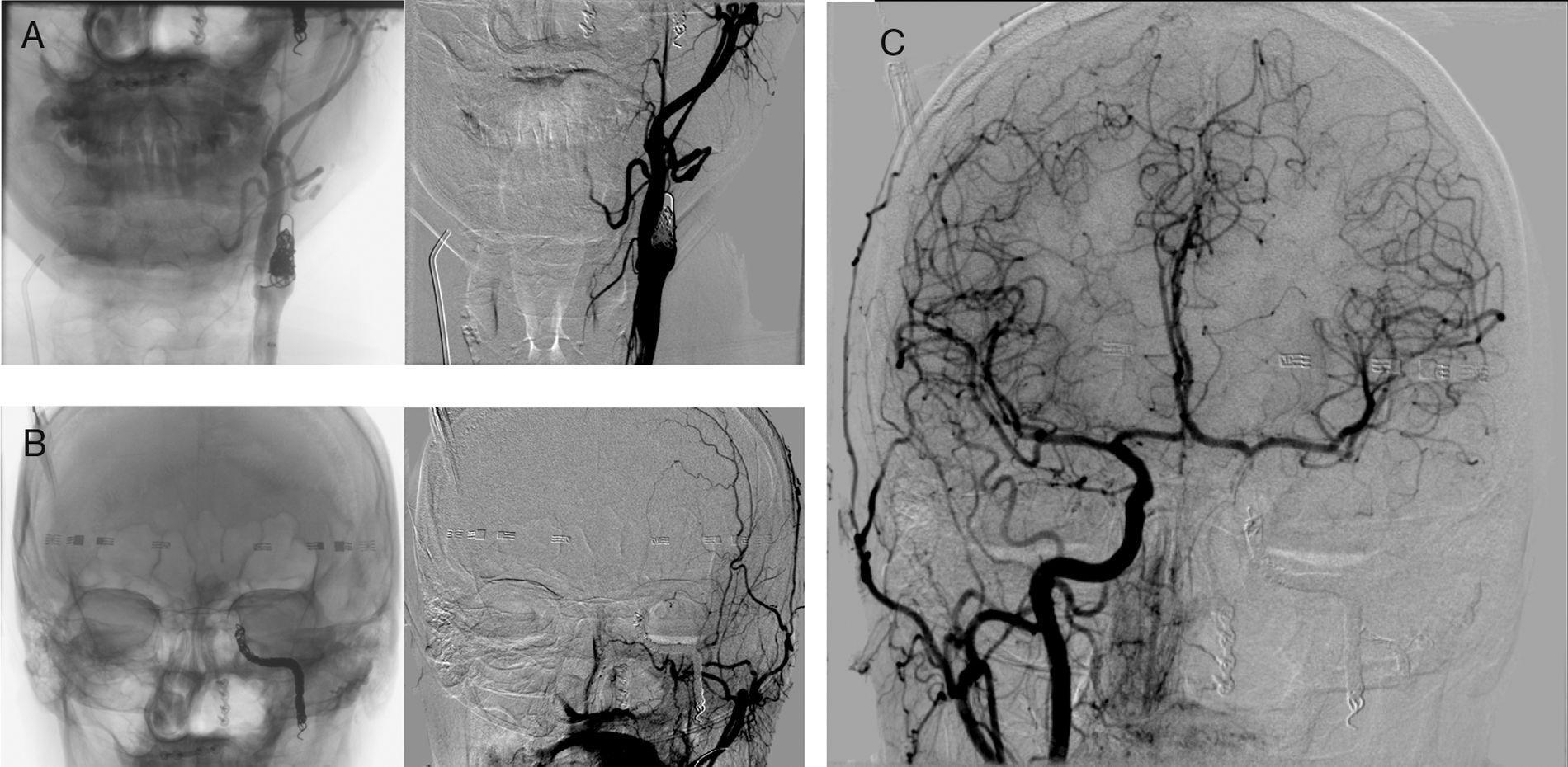
Frontal projections of brain angiography with contrast injection into the left common carotid artery, confirming occlusion of the proximal internal carotid artery (beyond carotid bifurcation) (A) and distal internal carotid artery (proximal to the ophthalmic artery) (B). C) Contrast injection into the right common carotid artery, revealing correct compensation of brain circulation through the anterior communicating artery.
(A-E) Computed tomography: A) baseline axial CT slice showing sulcal effacement and cortical contrast uptake in the left hemisphere; B-D) CBV, CBF, and TTP maps, respectively, showing no alterations in brain perfusion, and E) coronal CT angiography slice confirming occlusion of the internal carotid artery after bifurcation, with excellent intracranial compensation. F-H) Magnetic resonance imaging: F) axial FLAIR slice; G-H) axial DWI and ADC sequences, respectively. Signal alteration is observed on the FLAIR and DWI sequences at left parietal and frontal cortex level, with no restriction on the ADC map, which is compatible with vasogenic oedema.
Contrast-induced encephalopathy is a rare complication that may manifest as cortical blindness, encephalopathy, seizures, and focal neurological signs.3–6 Transient cortical blindness is the most frequent clinical manifestation.4,6 Risk factors include arterial hypertension, kidney failure, diabetes, and adverse reactions to contrast agents.3–7 However, the latter seem to be an idiosyncratic reaction not directly related to the concentration, volume, or type of iodinated contrast used.4 Symptoms manifest soon after the administration of the contrast agent and resolve within 24-72hours.3,4,6 Prognosis is usually favourable, although cases have been reported of permanent deficits or deaths secondary to oedema (15%).4,5 The most frequent CT findings are cortical or subcortical contrast uptake and sulcal effacement (23%-54%).4 Dual-energy CT may be useful for differentiating cerebral oedema from pseudoedema.5 Brain MRI frequently reveals increased signal on T2-weighted and FLAIR sequences, with increased intensity on DWI sequences and ADC maps, compatible with vasogenic oedema.5–7 Pathogenic mechanisms include damage to the blood-brain barrier caused by neurotoxicity of the contrast, changes in osmotic concentrations or release of endothelins, and vasospasms caused by vessel wall irritation with subsequent hypoperfusion.5 There is no evidence regarding the treatment of choice.4 Treatment sometimes consists of supportive management with hydration,6 although some authors opt to administer dexamethasone, manitol, antiepileptic drugs, antihypertensive drugs, or even intra-arterial verapamil.5,6
In conclusion, contrast-induced encephalopathy is an important and potentially severe entity to be considered in the differential diagnosis of patients displaying acute focal neurological signs after angiographic procedures with iodinated contrast. It is diagnosed by exclusion, and prognosis is generally excellent; it should therefore be considered before starting thrombolytic treatments.
Please cite this article as: Montejo C, Rodríguez A, Pascual-Vicente M, Renú A. Encefalopatía transitoria por contraste tras la embolización de la arteria carótida interna previa a la cirugía de carcinoma nasofaríngeo. Neurología. 2020;35:287–289.