Cerebral fat embolism (CFE) is an infrequent complication of displaced fractures of long bones. Diagnosis is usually clinical (the condition is characterised by neurological impairment, dyspnoea, and petechiae)1 and confirmed by neuroimaging. Computed tomography (CT) shows either no alterations or non-specific findings,2 with brain magnetic resonance imaging (MRI) being the most sensitive test for diagnosing the condition, especially with diffusion-weighted sequences (DWI) taken during the acute phase (<5 days). During the subacute phase (days 5-14), however, susceptibility-weighted imaging (SWI) is of greater use, as shown by the case presented here.
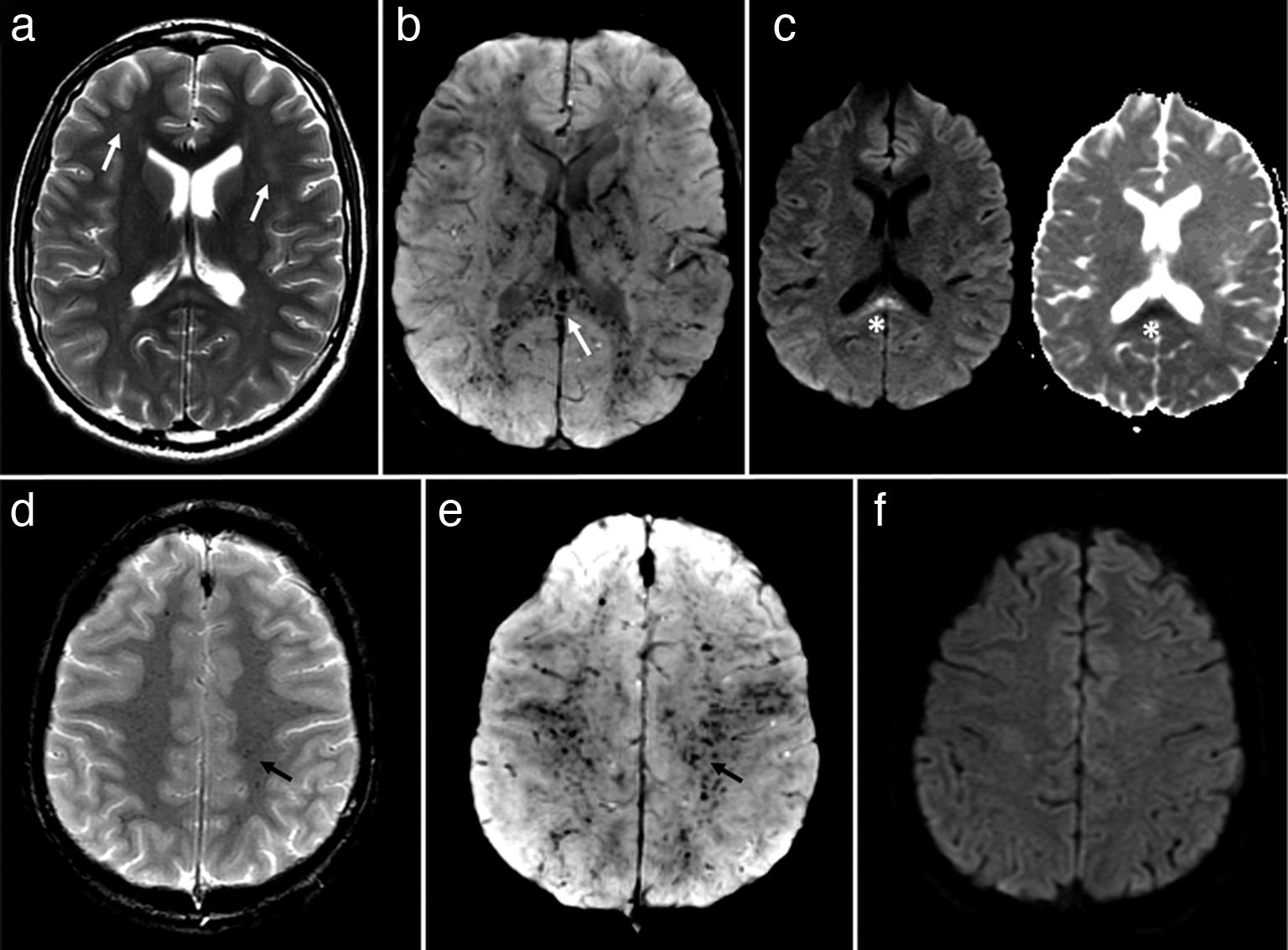
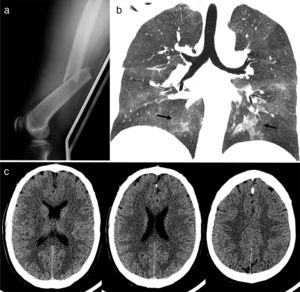
Our patient was a healthy, 32-year-old man who had suffered severe trauma to the left femur. He was conscious and stable upon arrival at the emergency department. Several hours later, after external fixation of the femur, the patient presented confusion, fever, and oxygen desaturation. We suspected CFE. A chest CT scan revealed ground-glass opacities suggestive of fat embolism; the head CT scan showed no abnormalities (Fig. 1). The eye fundus examination revealed isolated cotton-wool spots in the right eye. The patient improved over the following days, but bradypsychia, inattention, and reduced verbal fluency persisted. Clinical progression was favourable; on day 11, the external fixator was replaced with intramedullary nails made of an MRI-compatible material. A T2-weighted brain MRI scan revealed mild focal hyperintensities in the infra- and supratentorial white matter, especially in the semioval centres and the splenium of the corpus callosum. No abnormal diffusion restriction was observed, except in the lesion located in the splenium. SWI revealed diffuse punctiform hypointensities on the cerebellar white matter, lentiform nuclei, corpus callosum, and semioval centres, consistent with petechial haemorrhages. These findings were barely perceptible on T2*-weighted gradient-echo sequences (Fig. 2). Upon discharge, 16 days after admission, the patient displayed lack of concentration and no other neurological alterations or cognitive symptoms.
Studies performed upon admission to the emergency department. (a) Lateral radiograph of the left femur showing a displaced transverse fracture of the diaphysis. (b) Chest CT scan, coronal view: bilateral ground-glass opacities in the hilar region and both inferior lobes, typical of CFE. (c) Head CT scan showing no relevant alterations or white matter lesions.
Brain MRI study performed 12 days after symptom onset. (a) Bilateral, frontal deep white matter lesions that are barely visible on T2-weighted sequences (arrows). (b) Diffuse haemorrhagic petechiae affecting the white matter, lentiform nuclei, and splenium of the corpus callosum (arrow) are seen as markedly hypointense punctiform lesions on SWI. (c) The only lesion showing abnormal diffusion restriction (left) was located in the splenium (asterisk) (diffusion-weighted sequence on the right). (d) The T2*-weighted sequence shows less evident haemorrhagic petechiae in the semioval centres; these lesions are more clearly seen on SWI sequences (e) (arrow). (f) The DWI sequence shows no lesions with abnormal diffusion restriction, a typical feature of CFE.
CFE is rare in cases of long bone fractures, although patients with the condition frequently show some degree of asymptomatic fat embolism. Brain MRI during the acute phase is the most sensitive imaging technique for diagnosis: DWI reveals lesions arranged in a characteristic “starfield” pattern in a high percentage of patients.3 Cytotoxic oedema associated with CFE lesions is transient; therefore, the pattern typically seen on DWI is only observed in 18% of patients during the subacute phase.4,5 A considerable percentage of patients undergo MRI during this phase for numerous reasons, including the use of an external fixator (which is not compatible with MRI) or patient instability. In the light of the above, SWI constitutes a highly useful diagnostic tool6 and should always be included in the assessment protocol, since it is more sensitive than DWI and T2*-weighted sequences, which have traditionally been used to rule out bleeding.7,8 Around 60% of patients with CFE show diffuse petechial haemorrhages, predominantly affecting the white matter; the lesions usually appear on the first day and persist until the chronic phase.5,9 Two main hypotheses have been proposed to explain the pathophysiology of CFE: the first suggests that lesions result from mechanical vascular occlusion due to embolism, whereas the second postulates that lesions result from the proinflammatory effect of fatty acids; an interaction between both mechanisms is also plausible.8,10 The usefulness of MRI for determining the association between lesion extension and long-term neurological progression has not been studied, but should be addressed in future research.
We wish to thank Herminia Argente and Luis Bataller for their cooperation.
Please cite this article as: Gil-Perotin S, Carreres-Polo J. Valor de la secuencia de susceptibilidad magnética en formas subagudas de embolismo graso cerebral. Neurología. 2019;34:616–618.