People who consume drugs have a higher risk of latent tuberculosis infection (LTBI). Our objective was to study the characteristics of people who use drugs and who attended the Centers for Drug Dependence Care and Follow-up of Barcelona during 2017–2021 and presented LTBI or did not perform the reading of the tuberculin skin test (TST) after the test had been done.
Material and methodsA cross-sectional, descriptive study in Centers for Drug Dependence Care and Follow-up of Barcelona was performed during 2017–2021. The sociodemographic and epidemiological profile of people who use drugs that underwent a TST was analyzed and were examined the factors associated with LTBI. Additionally, the same sociodemographic and epidemiological analyses were made in PWUD that did not perform the reading of the TST after the test had been done. Adjusted odds ratios (ORa) and 95% confidence intervals (95% CI) were calculated.
ResultsNine hundred forty-eight persons were profiled. The prevalence of LTBI was 22.9%, and the following factors were associated with it: be older than 41 years; be users of CAS Baluard, or CAS Horta-Guinardó; coming from a WHO region of high TB incidence; be homeless; and low territorial socioeconomic index. The following factors were associated with not performing the reading of the TST after the test had been done: be users from the CAS Baluard, Barceloneta, Nou Barris and Robadors; be homeless and low TSI.
ConclusionsThis study improves TB control and highlights the need for this LTBI control program in CASs.
Las personas que consumen drogas tienen un mayor riesgo de infección tuberculosa latente (ITL). Nuestro objetivo fue medir las características de las personas que cosumen drogas y que acudieron a los centros de atención y seguimiento (CAS) a las drogodependencias de Barcelona entre 2017-2021 y que presentaron ITL, así como conocer el perfil de las que no acudieron a la lectura de la prueba de la tuberculina (PT).
Material y métodosSe realizó un estudio descriptivo transversal en los centros de atención y seguimiento a las drogodependencias de Barcelona durante el periodo 2017-2021. Se analizó el perfil sociodemográfico y epidemiológico de las personas que consumen drogas que se sometieron a una PT y se examinaron los factores asociados a la ITL. Además, los mismos análisis sociodemográficos y epidemiológicos se realizaron en las personas que consumen drogas que no realizaron la lectura de la PT después de realizarla. Se calcularon las odds ratio ajustadas (ORa) y los intervalos de confianza de 95% (IC 95%).
ResultadosSe estudiaron 948 personas. La prevalencia de ITL fue de 22,9%, y los factores asociados fueron: ser mayor de 41 años, ser usuarios del CAS Baluard, o del CAS Horta-Guinardó, provenir de una región de la Organización Mundial de la Salud de alta incidencia de TB, ser una persona sin hogar y bajo índice socioeconómico territorial (IST). Los siguientes factores se asociaron con no acudir a la lectura de PT después de la realización de la prueba: ser personas usuarias del CAS Baluard, Barceloneta, Nou Barris y Robadors; personas sin hogar y bajo IST.
ConclusionesEste estudio mejora el control de la TB y destaca la necesidad de este programa de control de ITL en los CAS.
In 2020, tuberculosis (TB) was the 14th cause of death in the world, and the second by a single infectious agent after COVID-19. In 2022, 10.5 million people became ill with TB and 1.6 million died from it. After two decades with a progressive decreases of TB incidence 2% per year, this growth implies an increase in incidence of 4% and an increase in mortality.1–4 Globally, the 2% decrease in TB incidence per year from 2000 to 2021 has been insufficient to achieve Goal 3 of the Sustainable Development Goals of the 2030 Agenda and the WHO's “End TB” strategy. Goal 3 aims to ensure healthy lives and promote the well-being of all at all ages. Such slow decline in overall TB incidence during the last 20 years has been observed both in high- and low-income countries. However, no decline has been shown among the most vulnerable groups, such as: elderly, chronically ill people, people who use drugs (PWUD), immigrants, homeless people, and people in prison.5–12 The transmission among these vulnerable groups is even higher6; therefore, they are at higher risk of latent TB infection (LTBI), and subsequently of TB.
The PWUD who access the Centers for Drug Dependence Care and Follow-up (Centros de Atención y Seguimiento a las Drogodependencias, CASs) in the city of Barcelona constitute a vulnerable population. This vulnerability is a consequence of the determinants of health inequalities at the urban level such as urban governance, the physical context, the socioeconomic context, and the environments. On the other hand, the influence of these determinants can vary according to the axes of inequality (social class, gender, age, ethnic group and migratory status).13–20
The objective of this work was to study the characteristics of the persons who use drugs (PUWD) and who attended the Centers for Drug Dependence Care and Follow-up (Centros de Atención y Seguimiento a las Drogodependencias, CASs) of Barcelona during 2017–2021 and presented LTBI or did not perform the reading of the TST after the test had been done. This study was based on an intervention directed and created by the Epidemiology Service of the Barcelona Public Health Agency (Agència de Salut Pública de Barcelona, ASPB) which consisted of providing tuberculin skin tests (TST) to the CASs of Barcelona to perform this test on their users. The proportion of LTBI in drug users who attended the CASs in the city of Barcelona during the period 2017–2021 was calculated and their sociodemographic and epidemiological characteristics were analyzed. The same sociodemographic and epidemiological analyses were also performed on drug users who did not take a TST reading after being tested.
Material and methodsStudy designAn epidemiological, cross-sectional study was performed in the city of Barcelona, in the period 2017–2021.
Study populationThe target population was represented by PWUD in the city of Barcelona during the period 2017–2021. The accessible population consisted in these people that attended the CASs of Barcelona in that same period. Finally, the eligible population was formed by PWUD that agreed to undergo a TST to screen for LTBI. The exclusion criteria were the following: antecedents of TB; already treated LTBI; and being included in a TB case contact study.
All CAS in the city of Barcelona were invited to participate: Baluard, CRD Robadors, Lluís Companys, Barceloneta, Center Català de Solidaritat (CECAS), Sants, Les Corts, Sarriá, Vall d’Hebron, Garbivent, Fòrum, Center de Mental Health and Addictions (CSMA) Gràcia, Horta-Guinardó, Nou Barris, Clínic-Esquerra Eixample and Sant Pau. Finally, the study has been carried out in the CASs of the city of Barcelona dependent on ASPB (7), Parc de Salut Mar (2) and CECAS. To sum up, the information collected came from the following CAS: Baluard, Robadors, Barceloneta, CECAS, Sants, Sarrià, Garbivent, Fòrum, Horta Guinardó and Nou Barris.
DefinitionsA TST was considered positive when the induration (measured in a transverse diameter to the forearm) was equal to or greater than 10mm, or equal to or greater than 5mm for people with HIV infection.21 In case of positivity to TST, the patient was referred to the Tuberculosis Unit (UTB) reference center of the city, Drassanes, to complete the study and eventually diagnose LTBI.
Sources of informationThe first source of information was a database managed by the Epidemiology Service (SEPID) of the ASPB. This database contained personal health data from the CASs. To recover lost information not available in the database, we consulted sources like the shared medical history, the Barcelona TB case repository (MDOWin), and the Barcelona TB contact repository (TBWin). Finally, to access social variables and consumption habits, we consulted the Barcelona Drug Information System, also depending on the ASPB, and the database of the territorial socioeconomic index (TSI) from the Statistic Institute of Catalonia (Institut d’Estadística de Catalunya, Idescat).22
VariablesThe following explanatory variables were collected: CAS; sex; age; country of origin (dichotomized according to Spanish born or foreign born); region of origin (according to WHO criteria); being a homeless person; TSI; being a person injecting drugs (PID); excessive alcohol consumption; history of HIV infection; and current TST. The response variables were LTBI and not performing the reading of the TST after the test had been done.
Age was categorized in two quantiles of older and younger age. WHO regions with a high burden of TB (Southeast Asia, Africa, and Western Pacific) were considered at high risk of developing TB, whereas regions with a low burden of TB (Europe, Eastern Mediterranean, and America) were considered at low risk. People were classified as homeless according to the European Typology on Homelessness and Housing Exclusion (ETHOS) categorization. As an index of the socio-economic characteristics TSI was used. TSI gives information on the employment situation, educational level, immigration status, and income of people residing in a territorial census section of Catalonia. According to the Idescat, TSI was considered high when ≥100 and low when <100.21 Finally, alcohol risk consumption was considered >280g/week in men and >140g/week in women.
Statistical analysisA descriptive analysis of the sociodemographic characteristics, consumption habits, and clinical variables by sex was performed in our population. The distribution of the age variable was analyzed with the Shapiro–Wilk test. Because this variable did not follow a normal distribution, the median was calculated as a central trend measure and the interquartile range (IQR) as a dispersion measure.
Pearson's Chi-square test was used to determine associations between qualitative variables. At the bivariate level, an analysis was carried out using a logistic regression model of the crude odds ratio (ORc) with 95% confidence intervals (CI) for each of the explanatory variables and the response variables LTBI and not going to the reading of the TST after the test had been done. At the multivariate level, an analysis was carried out using a logistic regression model of the adjusted odds ratio (ORa) with 95% CI for each of the explanatory variables and the variables response LTBI and not attending the reading of the TST after the test had been done. The variables introduced in the adjusted model were those that presented statistical significance in the unadjusted model.
For all statistical tests, the level of statistical significance (ρ) was 0.05. The RStudio Version 1.3.1093 program was used.
Ethical considerationsAll data were anonymized and treated in a strictly confidential manner following the directives here indicated: the ethical principles of the Declaration of Helsinki23; the Spanish Law on the Protection of Personal Data processed for the purposes of prevention, detection, investigation and prosecution of criminal offenses and the execution of criminal penalties Organic Law 07/202124; and the Directive (EU) 2016/680 of the European Parliament and of the Council, 27 April 2016.25 The project was approved by the Medicine Research Ethics Committee of the Parc de Salut Mar (CEIm-PSMAR 2021/10193).
ResultsBetween 2017 and 2021, 948 users attending the CASs of the city of Barcelona underwent a TST. The prevalence of LTBI in people who performed the reading of the test was 22.9%.
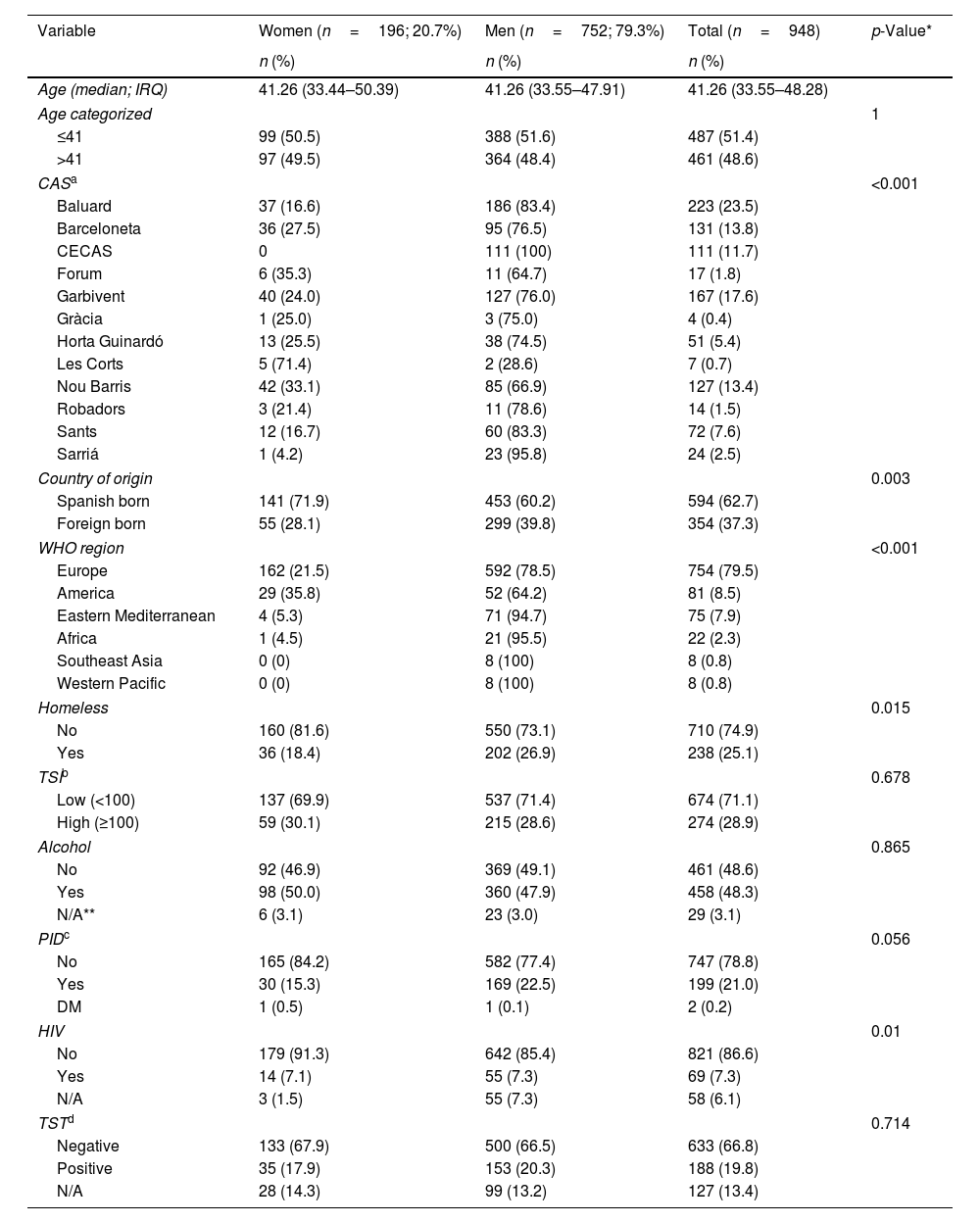
In our sample, the highest proportion of people were men; were from the following CASs: Baluard, Garbivent, Barceloneta, Nou Barris and CECAS; were Spanish born; were from the WHO region of Europe and had low TSI. Significant differences were observed depending on the CASs, the country of origin, the WHO region, being homeless, being a PID, and being positive for HIV (Table 1).
Descriptive characteristics of the Centers for Drug Dependence Care and Follow-up's users of Barcelona who agreed to take a tuberculin test in the period 2017–2021, by sex.
| Variable | Women (n=196; 20.7%) | Men (n=752; 79.3%) | Total (n=948) | p-Value* |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age (median; IRQ) | 41.26 (33.44–50.39) | 41.26 (33.55–47.91) | 41.26 (33.55–48.28) | |
| Age categorized | 1 | |||
| ≤41 | 99 (50.5) | 388 (51.6) | 487 (51.4) | |
| >41 | 97 (49.5) | 364 (48.4) | 461 (48.6) | |
| CASa | <0.001 | |||
| Baluard | 37 (16.6) | 186 (83.4) | 223 (23.5) | |
| Barceloneta | 36 (27.5) | 95 (76.5) | 131 (13.8) | |
| CECAS | 0 | 111 (100) | 111 (11.7) | |
| Forum | 6 (35.3) | 11 (64.7) | 17 (1.8) | |
| Garbivent | 40 (24.0) | 127 (76.0) | 167 (17.6) | |
| Gràcia | 1 (25.0) | 3 (75.0) | 4 (0.4) | |
| Horta Guinardó | 13 (25.5) | 38 (74.5) | 51 (5.4) | |
| Les Corts | 5 (71.4) | 2 (28.6) | 7 (0.7) | |
| Nou Barris | 42 (33.1) | 85 (66.9) | 127 (13.4) | |
| Robadors | 3 (21.4) | 11 (78.6) | 14 (1.5) | |
| Sants | 12 (16.7) | 60 (83.3) | 72 (7.6) | |
| Sarriá | 1 (4.2) | 23 (95.8) | 24 (2.5) | |
| Country of origin | 0.003 | |||
| Spanish born | 141 (71.9) | 453 (60.2) | 594 (62.7) | |
| Foreign born | 55 (28.1) | 299 (39.8) | 354 (37.3) | |
| WHO region | <0.001 | |||
| Europe | 162 (21.5) | 592 (78.5) | 754 (79.5) | |
| America | 29 (35.8) | 52 (64.2) | 81 (8.5) | |
| Eastern Mediterranean | 4 (5.3) | 71 (94.7) | 75 (7.9) | |
| Africa | 1 (4.5) | 21 (95.5) | 22 (2.3) | |
| Southeast Asia | 0 (0) | 8 (100) | 8 (0.8) | |
| Western Pacific | 0 (0) | 8 (100) | 8 (0.8) | |
| Homeless | 0.015 | |||
| No | 160 (81.6) | 550 (73.1) | 710 (74.9) | |
| Yes | 36 (18.4) | 202 (26.9) | 238 (25.1) | |
| TSIb | 0.678 | |||
| Low (<100) | 137 (69.9) | 537 (71.4) | 674 (71.1) | |
| High (≥100) | 59 (30.1) | 215 (28.6) | 274 (28.9) | |
| Alcohol | 0.865 | |||
| No | 92 (46.9) | 369 (49.1) | 461 (48.6) | |
| Yes | 98 (50.0) | 360 (47.9) | 458 (48.3) | |
| N/A** | 6 (3.1) | 23 (3.0) | 29 (3.1) | |
| PIDc | 0.056 | |||
| No | 165 (84.2) | 582 (77.4) | 747 (78.8) | |
| Yes | 30 (15.3) | 169 (22.5) | 199 (21.0) | |
| DM | 1 (0.5) | 1 (0.1) | 2 (0.2) | |
| HIV | 0.01 | |||
| No | 179 (91.3) | 642 (85.4) | 821 (86.6) | |
| Yes | 14 (7.1) | 55 (7.3) | 69 (7.3) | |
| N/A | 3 (1.5) | 55 (7.3) | 58 (6.1) | |
| TSTd | 0.714 | |||
| Negative | 133 (67.9) | 500 (66.5) | 633 (66.8) | |
| Positive | 35 (17.9) | 153 (20.3) | 188 (19.8) | |
| N/A | 28 (14.3) | 99 (13.2) | 127 (13.4) | |
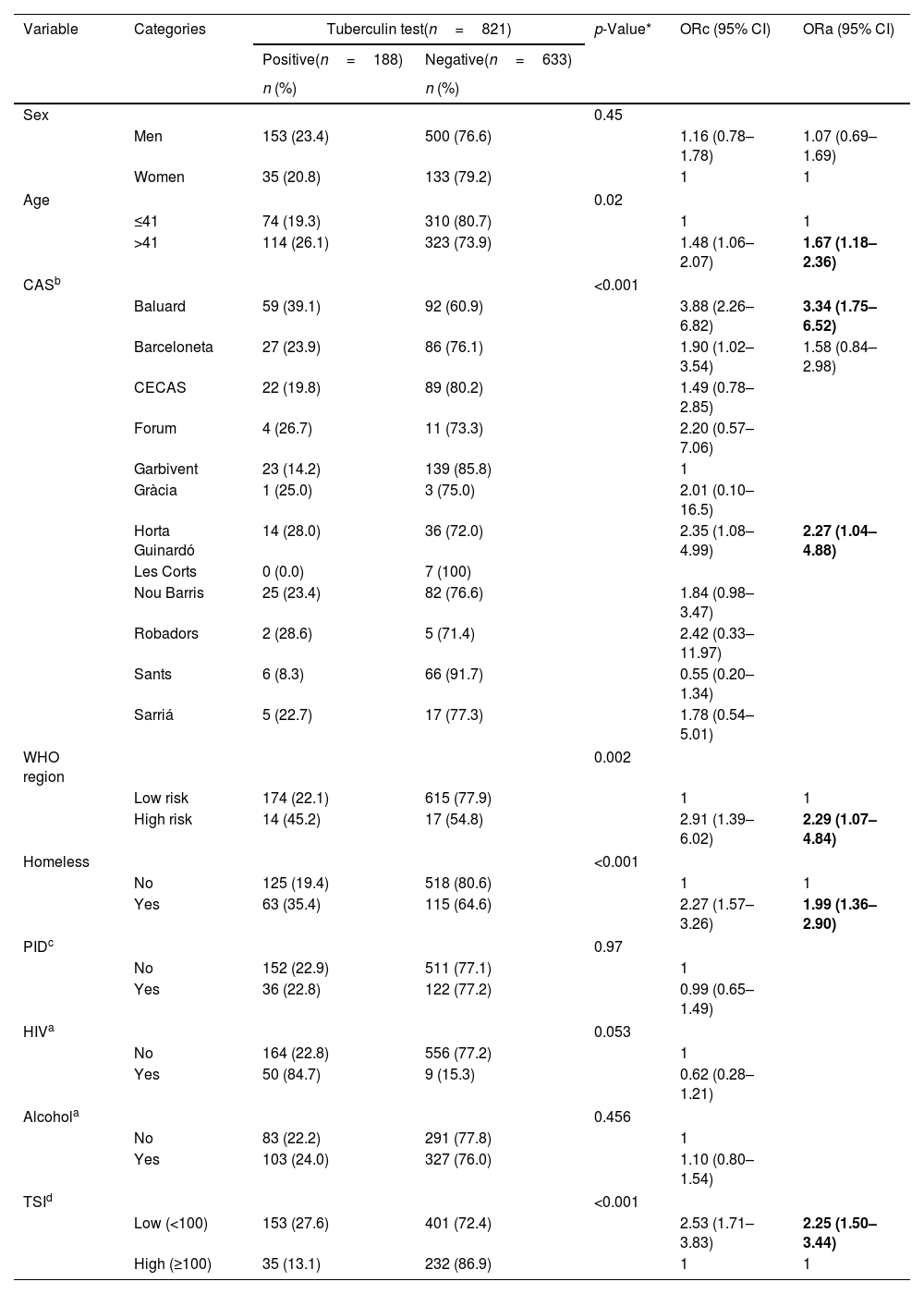
People were significantly more predisposed to be positive for LTBI were older than 41 years; when belonging to CAS Baluard, Barceloneta, and Horta-Guinardó; coming from WHO regions with highest risk of TB; being homeless; and living in a census section of Barcelona with low TSI. No significant differences were observed by sex, PID, HIV, or alcohol. Finally, the factors independently associated with LTBI were users of CAS Baluard or Horta-Guinardó; be older than 41 years; come from a WHO region at highest risk of TB; be homeless and live in a neighborhood with low TSI (Table 2).
Factors associated with latent tuberculosis infection of the Centers for Drug Dependence Care and Follow-up's users of Barcelona who agreed to take a tuberculin test in the period 2017–2021.
| Variable | Categories | Tuberculin test(n=821) | p-Value* | ORc (95% CI) | ORa (95% CI) | |
|---|---|---|---|---|---|---|
| Positive(n=188) | Negative(n=633) | |||||
| n (%) | n (%) | |||||
| Sex | 0.45 | |||||
| Men | 153 (23.4) | 500 (76.6) | 1.16 (0.78–1.78) | 1.07 (0.69–1.69) | ||
| Women | 35 (20.8) | 133 (79.2) | 1 | 1 | ||
| Age | 0.02 | |||||
| ≤41 | 74 (19.3) | 310 (80.7) | 1 | 1 | ||
| >41 | 114 (26.1) | 323 (73.9) | 1.48 (1.06–2.07) | 1.67 (1.18–2.36) | ||
| CASb | <0.001 | |||||
| Baluard | 59 (39.1) | 92 (60.9) | 3.88 (2.26–6.82) | 3.34 (1.75–6.52) | ||
| Barceloneta | 27 (23.9) | 86 (76.1) | 1.90 (1.02–3.54) | 1.58 (0.84–2.98) | ||
| CECAS | 22 (19.8) | 89 (80.2) | 1.49 (0.78–2.85) | |||
| Forum | 4 (26.7) | 11 (73.3) | 2.20 (0.57–7.06) | |||
| Garbivent | 23 (14.2) | 139 (85.8) | 1 | |||
| Gràcia | 1 (25.0) | 3 (75.0) | 2.01 (0.10–16.5) | |||
| Horta Guinardó | 14 (28.0) | 36 (72.0) | 2.35 (1.08–4.99) | 2.27 (1.04–4.88) | ||
| Les Corts | 0 (0.0) | 7 (100) | ||||
| Nou Barris | 25 (23.4) | 82 (76.6) | 1.84 (0.98–3.47) | |||
| Robadors | 2 (28.6) | 5 (71.4) | 2.42 (0.33–11.97) | |||
| Sants | 6 (8.3) | 66 (91.7) | 0.55 (0.20–1.34) | |||
| Sarriá | 5 (22.7) | 17 (77.3) | 1.78 (0.54–5.01) | |||
| WHO region | 0.002 | |||||
| Low risk | 174 (22.1) | 615 (77.9) | 1 | 1 | ||
| High risk | 14 (45.2) | 17 (54.8) | 2.91 (1.39–6.02) | 2.29 (1.07–4.84) | ||
| Homeless | <0.001 | |||||
| No | 125 (19.4) | 518 (80.6) | 1 | 1 | ||
| Yes | 63 (35.4) | 115 (64.6) | 2.27 (1.57–3.26) | 1.99 (1.36–2.90) | ||
| PIDc | 0.97 | |||||
| No | 152 (22.9) | 511 (77.1) | 1 | |||
| Yes | 36 (22.8) | 122 (77.2) | 0.99 (0.65–1.49) | |||
| HIVa | 0.053 | |||||
| No | 164 (22.8) | 556 (77.2) | 1 | |||
| Yes | 50 (84.7) | 9 (15.3) | 0.62 (0.28–1.21) | |||
| Alcohola | 0.456 | |||||
| No | 83 (22.2) | 291 (77.8) | 1 | |||
| Yes | 103 (24.0) | 327 (76.0) | 1.10 (0.80–1.54) | |||
| TSId | <0.001 | |||||
| Low (<100) | 153 (27.6) | 401 (72.4) | 2.53 (1.71–3.83) | 2.25 (1.50–3.44) | ||
| High (≥100) | 35 (13.1) | 232 (86.9) | 1 | 1 | ||
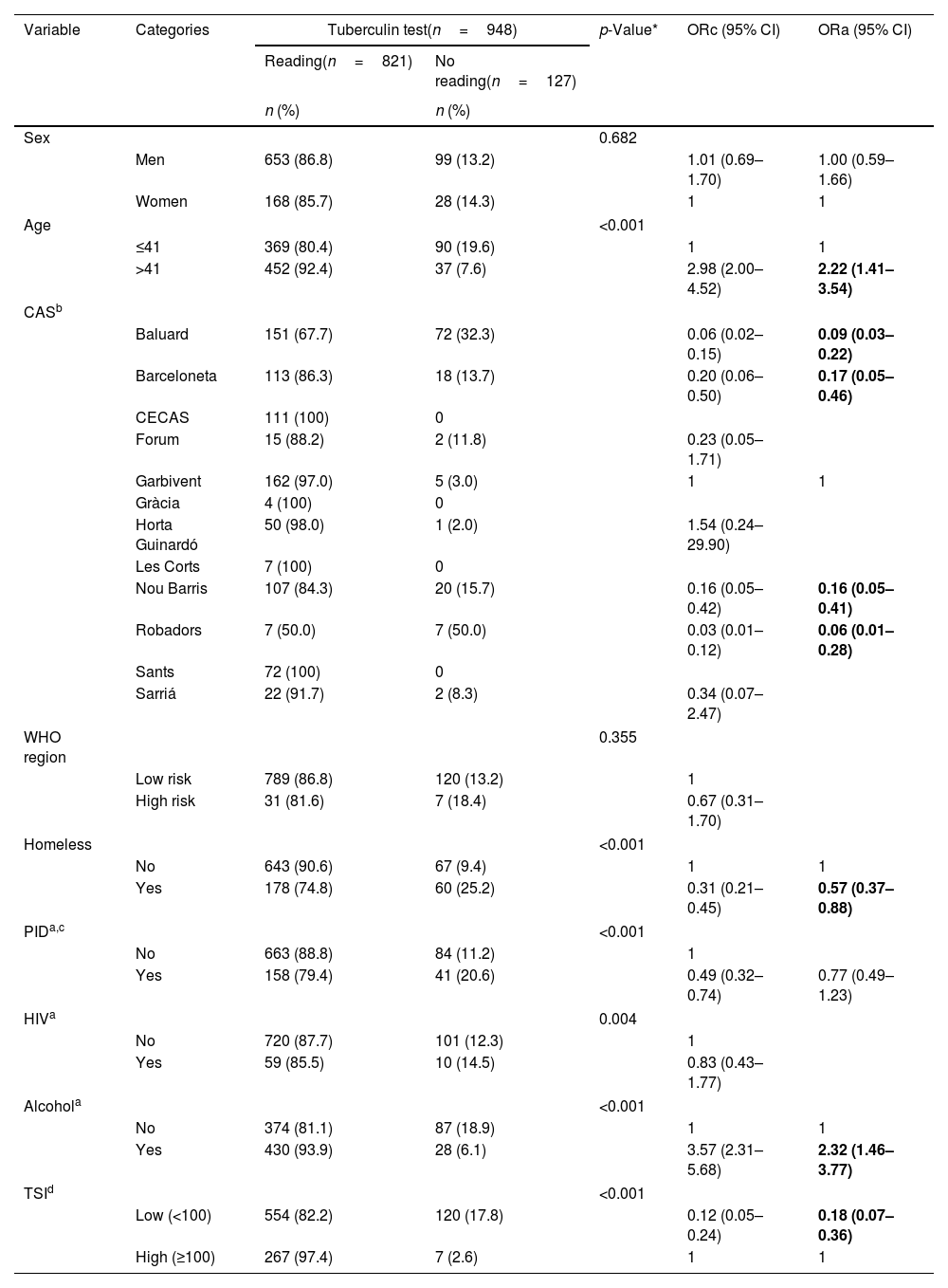
A total of 127 (13.4%) people did not perform the reading of the TST after the test had been done. In the multivariate analysis, the factors associated with not performing the reading of the test after it had been done were: be users from the CAS Baluard, Barceloneta, Nou Barris and Robadors; be homeless and low TSI. On the contrary, factors associated with performing the reading of the TST after it had been done were: be older than 41 years and present an excessive alcohol consumption (Table 3).
Factors associated with performing TST reading after taking the tuberculin test in people attending in the Centers for Drug Dependence Care and Follow-up of Barcelona in the period 2017–2021.
| Variable | Categories | Tuberculin test(n=948) | p-Value* | ORc (95% CI) | ORa (95% CI) | |
|---|---|---|---|---|---|---|
| Reading(n=821) | No reading(n=127) | |||||
| n (%) | n (%) | |||||
| Sex | 0.682 | |||||
| Men | 653 (86.8) | 99 (13.2) | 1.01 (0.69–1.70) | 1.00 (0.59–1.66) | ||
| Women | 168 (85.7) | 28 (14.3) | 1 | 1 | ||
| Age | <0.001 | |||||
| ≤41 | 369 (80.4) | 90 (19.6) | 1 | 1 | ||
| >41 | 452 (92.4) | 37 (7.6) | 2.98 (2.00–4.52) | 2.22 (1.41–3.54) | ||
| CASb | ||||||
| Baluard | 151 (67.7) | 72 (32.3) | 0.06 (0.02–0.15) | 0.09 (0.03–0.22) | ||
| Barceloneta | 113 (86.3) | 18 (13.7) | 0.20 (0.06–0.50) | 0.17 (0.05–0.46) | ||
| CECAS | 111 (100) | 0 | ||||
| Forum | 15 (88.2) | 2 (11.8) | 0.23 (0.05–1.71) | |||
| Garbivent | 162 (97.0) | 5 (3.0) | 1 | 1 | ||
| Gràcia | 4 (100) | 0 | ||||
| Horta Guinardó | 50 (98.0) | 1 (2.0) | 1.54 (0.24–29.90) | |||
| Les Corts | 7 (100) | 0 | ||||
| Nou Barris | 107 (84.3) | 20 (15.7) | 0.16 (0.05–0.42) | 0.16 (0.05–0.41) | ||
| Robadors | 7 (50.0) | 7 (50.0) | 0.03 (0.01–0.12) | 0.06 (0.01–0.28) | ||
| Sants | 72 (100) | 0 | ||||
| Sarriá | 22 (91.7) | 2 (8.3) | 0.34 (0.07–2.47) | |||
| WHO region | 0.355 | |||||
| Low risk | 789 (86.8) | 120 (13.2) | 1 | |||
| High risk | 31 (81.6) | 7 (18.4) | 0.67 (0.31–1.70) | |||
| Homeless | <0.001 | |||||
| No | 643 (90.6) | 67 (9.4) | 1 | 1 | ||
| Yes | 178 (74.8) | 60 (25.2) | 0.31 (0.21–0.45) | 0.57 (0.37–0.88) | ||
| PIDa,c | <0.001 | |||||
| No | 663 (88.8) | 84 (11.2) | 1 | |||
| Yes | 158 (79.4) | 41 (20.6) | 0.49 (0.32–0.74) | 0.77 (0.49–1.23) | ||
| HIVa | 0.004 | |||||
| No | 720 (87.7) | 101 (12.3) | 1 | |||
| Yes | 59 (85.5) | 10 (14.5) | 0.83 (0.43–1.77) | |||
| Alcohola | <0.001 | |||||
| No | 374 (81.1) | 87 (18.9) | 1 | 1 | ||
| Yes | 430 (93.9) | 28 (6.1) | 3.57 (2.31–5.68) | 2.32 (1.46–3.77) | ||
| TSId | <0.001 | |||||
| Low (<100) | 554 (82.2) | 120 (17.8) | 0.12 (0.05–0.24) | 0.18 (0.07–0.36) | ||
| High (≥100) | 267 (97.4) | 7 (2.6) | 1 | 1 | ||
The prevalence of LTBI in the CASs of the city of Barcelona (22.9%) is similar to the one estimated at global level, but 10% higher than the one estimated for the European WHO region to which Barcelona belongs (13%).9,26,27 Moreover, the prevalence is even higher in the CASs located in more disadvantaged neighborhoods with a higher incidence of TB. Indeed, among the PWUD of CAS Baluard, the prevalence of LTBI is 39.7%, similar to what found in the period 2013–2016 in the district of Nou Barris (33.2%).16
The prevalence of LTBI was greater in older people. This could be due to the exposure that people accumulate over time. Other studies in inmates recently incarcerated in a men's prison in Barcelona and Madrid found an association of LTBI with being older than 40 years and coming from countries with high TB burden or being people with a low income.14,15,19
In our study we found a high proportion of LTBI in PIDs (19.1%) and people with HIV (26.5%), however no association was observed. In the case of PID, this might be due to the fact that people that actively consume drugs, and so are more exposed to the infection, may not be visited in CAS. In the case of people diagnosed with HIV, most of them are treated with antiretrovirals, therefore lowering the risk of TB.28
The prevalence of LTBI founded (22.9%) is lower than that of other studies that calculate this prevalence in people in prison (54.6% and 40.4%).14,15 This difference is probably related to the fact that the ITBL calculation in these prison studies is done with men and, in our sample, there was a 20.7% of women.
In the implementation of the program, we detected that the people who did not perform the reading of the TST after the test had been done were people in a situation of vulnerability who were users of the CAS Baluard, Barceloneta, Nou Barris or Robadors, homeless people and people with low TSI. These results are essential when planning future public health interventions aimed specifically at this group of people and intensifying those already started.
One of the main limitations of our study is the heterogeneity of the population with different risks of LTBI. For example, on a regular basis, the reference CAS is the closest to home; therefore, the profiles of people attending different CAS can be very different.29 Another of the limitations of our study is the selection bias caused by different factors: performing the TST was voluntary; some of the people who did the test did not perform the reading; the study specifically involved the CAS of the city of Barcelona depending on ASPB, Parc de Salut Mar, and CECAS. Another limitation of the study was not having the vaccination variable, which can lead to error in the reading of the tuberculin test. Another limitation is represented by the lack of knowledge on previous history of LTBI and TB, on specific living conditions (i.e., overcrowding), and on variables referring to substance consumption. For this work, we started conceiving a population-based study considering the population that attended some of the CAS of the city of Barcelona. Subsequently, we found out that not all CAS attendants are screened for LTBI. Therefore, we must insist in screening the entire population attending the CAS and improving the follow-up of people testing positive, and this should be the first main improvement of the intervention.
One of the strengths of our study is that it is the first one analyzing the prevalence of LTBI in CAS users, whereas others studied it in prisons in Spain14,15 or in one CAS in Barcelona.16 Knowing the factors associated with LTBI will allow us to improve our intervention in vulnerable populations, with impaired access to the health system and a consequently impaired diagnosis of the infection. This would finally lead to a better treatment of these populations.
From a Public Health approach, it is essential to continue the search for LTBI cases, both in the group of people who use drugs and in other vulnerable ones. This way, it would be possible to address reservoirs of probable cases in the future in order to move toward the elimination of TB, as marked by the WHO End TB strategy.7 Also, it is necessary to perform further studies to evaluate the introduction of LTBI treatment as a preventive measure for the development of TB. Finally, other studies must specifically analyze CAS users according to their sociodemographic characteristics and stratify them by the different centers of Barcelona.
This study aimed to assess this intervention in the CAS of Barcelona, within the TB Prevention and Control Program. It allowed to establish improvements in the collection of information and in the establishment of measures to control infection in a vulnerable population, guiding future public health interventions for the detection of LTBI.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributionsEach of the authors of the article has contributed substantially to the elaboration of the manuscript.
Conflicts of interestNone declared.
We want to thank all the participants in the study, both Drug Dependence Care and Follow-up professionals and citizens. We also express our gratitude for the support received by the staff of the Servei d’Epidemiologia and Servei de Prevenció i Atenció a les Drogodependències of the Agència de Salut Pública de Barcelona.
CAS Nou Barris, Barcelona, Spain (MA Carrillo Conde, N Mestres Lechón, I Osorio, Y Cordova); CAS Baluard, Barcelona, Spain (C Nadal); CAS Horta-Guinardó, Barcelona, Spain (A Mesalles Ruiz, M Jiménez, A Benedetti, L Choueva); CAS Barceloneta, Barcelona, Spain (A Roquer Grau, MC Martínez Quesada), CAS Sarrià, Barcelona, Spain (M Soler, A Bruguera Guitart); CAS Forum, Barcelona, Spain (F Díaz Alcoba, N Sabadell Aparicio, S Amador Muñoz).
ASPB: Public Health Agency of Barcelona (Agència de Salut Pública de Bareclona)
BCG: Bacillus de Calmette and Guérin
CAS: Centros de Atención y Seguimiento a las Drogodependencias (Centers for Drug Dependence Care and Follow-up)
CEIC: Clinical Research Ethics Committee
CI: Confidence interval
DOT: Directly observed treatment
EDO: Notifiable disease
ETODA: Outpatient Direct Observation Treatment Team
EU: European Union
HIV: Human immunodeficiency virus
IGRA: Interferon-gamma release assay
IMAS: Municipal Institute of Health Care
LTBI: Latent tuberculosis infection
MDOWIN: Application for notifiable diseases of the ASPB
Orc: Crude odds ratio
Ora: Adjusted odds ratio
PID: Person who injects drugs
PPCTB: Tuberculosis Prevention and Control Program
PWUD: People who consume drugs
Rx: Chest X-ray
TB: Tuberculosis
TBWIN: Application for studies of tuberculosis contacts in the city of Barcelona
TITL: Treatment of latent tuberculosis infection
TSI: Territorial socioeconomic index
TST: Tuberculin skin test
UTB Tuberculosis Unit
WHO World Health Organization
A form has been designed to collect the variables. To facilitate the recording, the definition of each of the variables is explained in this document.
Country of birth: Country where the person was born.
Date of birth: Indicator of age. It will be entered as day, month, and year.
Date of screening: Day in which the tuberculin skin test is administered.
First and last name: Patient identifier. It can be replaced by the CIP.
Homeless person: Variable indicating a person living on the street, in squatters’ houses, narco-apartments, or municipal shelters. 1: Yes, 2: No, 9: N/A.
HIV: Indicator of HIV infection. The values for the variable are 1 for infected, 2 for not infected, 3 for test not performed, and 9 for unread.
NHC: Número de Historia Clínica, clinical history number at the screening center.
PID: Variable including people that inject or injected drugs. Value 1 is selected for Yes, 2 for No, and 9 N/A.
Sex: Possible variable for stratification. It is entered as value 1 for men and 2 for women.
TST current: Result of the tuberculin test administered on the screening date. The values are 0 for not performed, 1 for positive, 2 for negative, and 9 for unread. mm: millimeters of induration of the TST. It is recorded in numbers.