Continuous positive airway pressure (CPAP) is the gold standard therapy for obstructive sleep apnoea (OSA). However, non-adherence is common and costly. The COVID-19 pandemic required the use of novel solutions to ensure service provision and quality of care. This retrospective analysis determined the impact and value of a digital versus standard pathway for the management of OSA in Spain.
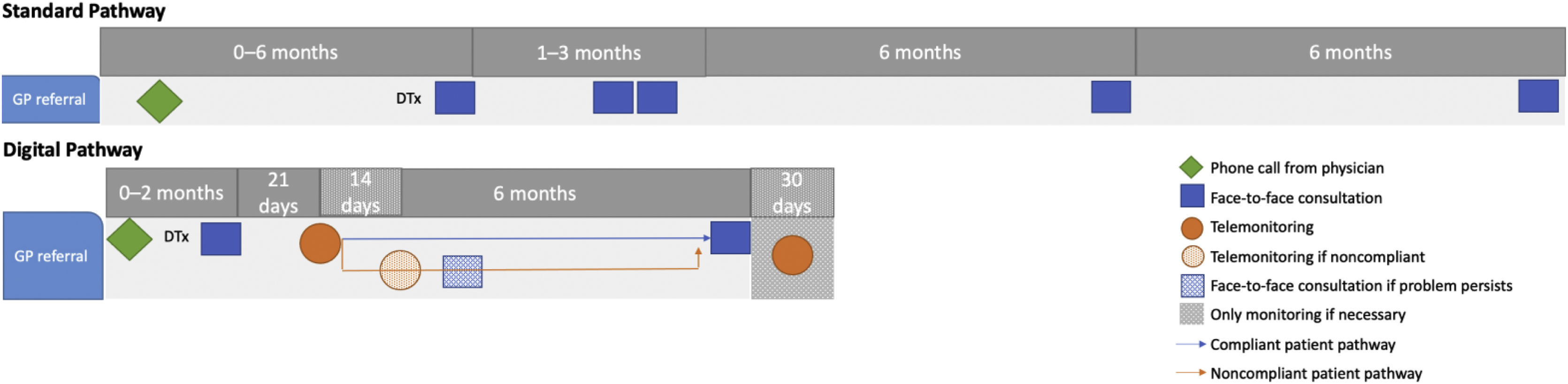
Material and methodsA time-driven activity-based costing approach was applied to OSA management over 1 year using a standard or digital pathway. The standard pathway included face-to-face appointments at the time of diagnosis, then after 1–3 months and every 6 months thereafter. The digital pathway had fewer face-to-face appointments and utilised telemonitoring. A cost analysis was performed to determine the per-patient cost per healthcare professional (HCP) for a digital pathway for therapy implementation and follow-up compared with the standard pathway.
ResultsCompared with the standard pathway, the digital pathway decreased the waiting list time from 18 to 2 months, the overall pathway time from 12 to 6 months, HCP cost per patient from €95 to €85, and number of hospital appointments per patient from 6 to 3.1. Furthermore, CPAP device usage improved from 5.7 to 6.3h/night and the proportion of individuals defined as adherent increased from 79% to 91%.
ConclusionsImplementation of digital processes using available technology reduced HCP time and costs, and improved adherence to CPAP in people with OSA. Greater utilisation of a digital pathway could improve access to therapy, allow personalised patient management, and facilitate better clinical outcomes.
La presión positiva continua en la vía aérea (CPAP) es el tratamiento de referencia para la apnea obstructiva del sueño (AOS). Sin embargo, su incumplimiento es frecuente y costoso. La pandemia de COVID-19 requirió el uso de soluciones novedosas para garantizar la prestación de servicios y la calidad de la atención. Este análisis retrospectivo determinó el impacto y el valor de un pathway digital frente a un pathway estándar para el manejo de la AOS en España.
Material y métodosSe aplicó el Time-DrivenActivityBasedCosting al tratamiento de la AOS durante 1 año utilizando el pathway estándar o digital. El pathway estándar incluía citas presenciales en el momento del diagnóstico, después de 1 a 3 meses y posteriormente cada 6 meses. el pathway digital tenía menos citas presenciales y utilizaba la telemonitorización. Se realizó un análisis de costes para determinar el coste por paciente y profesional sanitario (HCP) del pathway digital para la implementación y el seguimiento de la terapia en comparación con el pathway estándar.
ResultadosEn comparación con el pathway estándar, el pathway digital redujo el tiempo de la lista de espera de 18 a 2 meses, el tiempo total del pathway del paciente de 12 a 6 meses, el coste del HCP por paciente de 95 a 85 euros, y el número de citas hospitalarias por paciente de 6 a 3,1. Además, el uso del dispositivo de CPAP mejoró de 5,7 a 6,3 h/noche y la proporción de pacientes definidos como adherentes aumentó del 79% al 91%.
ConclusionesLa implementación de procesos digitales utilizando la tecnología disponible redujo el tiempo y los costes del HCP y mejoró la adherencia a la CPAP en personas con AOS. Una mayor utilización de un pathway digital podría mejorar el acceso a la terapia, permitir una gestión personalizada del paciente y facilitar mejores resultados clínicos.
Obstructive sleep apnoea (OSA) is the most common form of sleep-disordered breathing. Nearly 1 billion individuals aged 30–69 years worldwide have been estimated to have OSA based on an apnoea-hypopnoea index (AHI) cut-off value of 5events/h, with 425 million having moderate-to-severe disease requiring treatment (AHI≥15h−1).1 The number of people in Europe with any or moderate-to-severe OSA is approximately 175 million and 90 million, respectively.2 In Spain, around 26%–28% of the adult population are affected by OSA, and the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) has estimated that only 25% of these receive treatment.3
OSA is not a benign condition. Symptoms such as excessive daytime sleepiness can have a negative impact on normal daily functioning, cognitive function, mood and quality of life.4–7 In addition, the presence of OSA increases the risk of developing or worsening several significant comorbidities, including hypertension, cardiovascular disease, stroke, atrial fibrillation and diabetes.8–14 Prior to diagnosis, people with OSA have significantly higher healthcare consumption than healthy individuals or matched controls,15–17 and accurate diagnosis followed by effective treatment has been shown to significantly reduce healthcare costs.18
Continuous positive airway pressure (CPAP) is the gold standard therapy for treating moderate-to-severe OSA.19 Adequate adherence to CPAP therapy over the long term is essential to allow the benefits of therapy to be realised.20 Furthermore, Spanish data show that treatment of symptomatic moderate-to-severe OSA with CPAP was cost effective from the second year of therapy.21 Nevertheless, achieving good adherence to CPAP therapy remains a significant challenge in the management of individuals with OSA.
In Spain, positive airway pressure therapies such as CPAP are delivered by home care providers on a “one size fits all” basis. However, only about two-thirds of patients achieved good long-term CPAP adherence in one large Spanish study,22 and similar (although slightly higher) CPAP adherence rates were seen during the COVID-19 pandemic.23 Therefore, there is room for improvement in service delivery and adherence rates. The first wave of the COVID-19 pandemic saw the suspension of in-person sleep unit services. Based on a good existing level of experience with telemonitoring, the Hospital Marqués de Valdecilla, Santander, Spain, was ideally placed to adapt workflows and implement a more digitally-based approach to OSA management. However, the effects of this process change were not clearly understood. Therefore, this retrospective analysis determined the effects and value of a digital versus standard pathway to management of OSA in Spain. The hypothesis was that changes in processes to utilise telemonitoring and remote patient management during the COVID-19 pandemic would decrease healthcare professional (HCP) resource requirements and have a beneficial effect on process quality indicators.
Material and methodsStudy designThis retrospective analysis included all patients referred during two different periods to the Sleep and Ventilation Unit of the Marqués de Valdecilla Hospital, Santander, Spain, who were diagnosed with OSA with indication for treatment with CPAP and treated in accordance with standard clinical practice. This unit is a SEPAR-accredited unit of excellence that provides approximately 2400 diagnostic tests per year, is responsible for the prescription of around 1200 home care therapies each year, has about 9000 individuals receiving home care therapies, and has the largest number of individuals managed using telemonitoring of any centre in Spain (approximately 8000). The two time periods were chosen for retrospective data collection: 1 January to 31 December 2019 (standard therapy pathway group) and 1 January to 31 December 2021 (digital therapeutic pathway group).
This analysis formed part of the secondary endpoints of a larger Spanish study Big Data analysis of OSA patients on Positive Airway Pressure (PAP) treatment: real-life monitoring. TeleVAL Study, which was approved by the Comité de Ética de la Investigación con Medicamentos y productos sanitarios de Cantabria (CEIm). All patient data from hospital records was deidentified, and all analyses were conducted in accordance with local privacy legislation.
Score cardIn the absence of any specific core set for OSA patients from the International Consortium for Health Outcomes Measurement (ICHOM), a ‘score card’ was developed based on discussions with the clinical team, information collected in clinical records, and patient interviews. This includes outcome measures (Epworth Sleepiness Scale [ESS] score, AHI, adherence, therapy termination, annual compliance rate), healthcare resource utilisation (healthcare professional [HCP] time, HCP cost, number of hospital visits per person, number of telemonitoring sessions per person) and process quality indicators (waiting list time, time from diagnostic to treatment initiation, and time from treatment initiation to discharge from regular follow-up). Data for all these parameters were obtained from hospital records and/or device data download. As per the SEPAR definition, an individual was considered compliant with CPAP therapy when device usage was >4h/night on >70% of nights.
Process mapping and costsEach process had two main components: diagnosis and therapy. The diagnostic process, and associated HCP time and costs per patient, was assumed to be identical for the standard and digital pathways (Figure S1). Therapy was mapped separately for each of the two pathways of interest (Figure S2). Therapy pathways were defined by the clinical team involved in patient care, using the hospital database and other therapy-related information. Key components were consultation, therapy initiation (titration in the standard pathway and via telemonitoring in the digital pathway), and follow-up; these are summarised in Fig. 1.
A time-driven activity-based costing (TDABC) approach24,25 was used to determine administrative, nursing and pulmonologist time and costs for all components of the therapeutic pathway. Total available annual clinical minutes and average salary for each type of HCP were used to calculate the cost per minute of HCP time (Table S1); this was multiplied by the number of minutes required to perform each task in both therapeutic pathways to assign per-patient costs to each task (Table S2).
Statistical analysisAll data are presented using descriptive statistics. Qualitative data are reported as absolute and relative frequencies. For quantitative variables, the normality of data distribution was determined using the Kolmogorov–Smirnov test, then values are reported as mean±standard deviation (if normally distributed) or median [interquartile range] (if not normally distributed). Statistical analyses were performed using IBM SPSS Statistics for Windows Version 25.0 (IBM Corp., Armonk, NY) and MedCalc Statistical Software Version 19.6 (MedCalc Software by, Ostend, Belgium; https://www.medcalc.org; 2020).
ResultsDatasetData from a total of 2329 individuals were used in the current analysis; 1094 were managed using the standard pathway and 1235 were managed using the digital pathway.
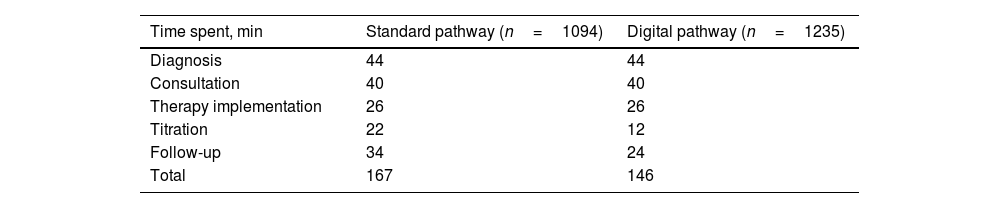
Process timings and costsTotal times for diagnosis, consultation, and therapy initiation were the same in the standard and digital pathway groups; however, times spent on CPAP titration and follow-up were lower in the digital pathway group meaning that the total pathway time was 13% shorter in the digital group (146 vs. 167min) (Table 1). The total number of telemonitoring interactions per patient in the digital pathway group was two.
Overall times from diagnosis to treatment (10 vs. 14 days; a 28% reduction) and from treatment to discharge from regular follow-up (6 vs. 12 months; a 50% reduction) were lower in the digital versus standard pathway group. In addition, the waiting list time for sleep services decreased substantially from 18 months with the standard pathway to 2 months with the digital pathway (a reduction of 1 year and 4 months).
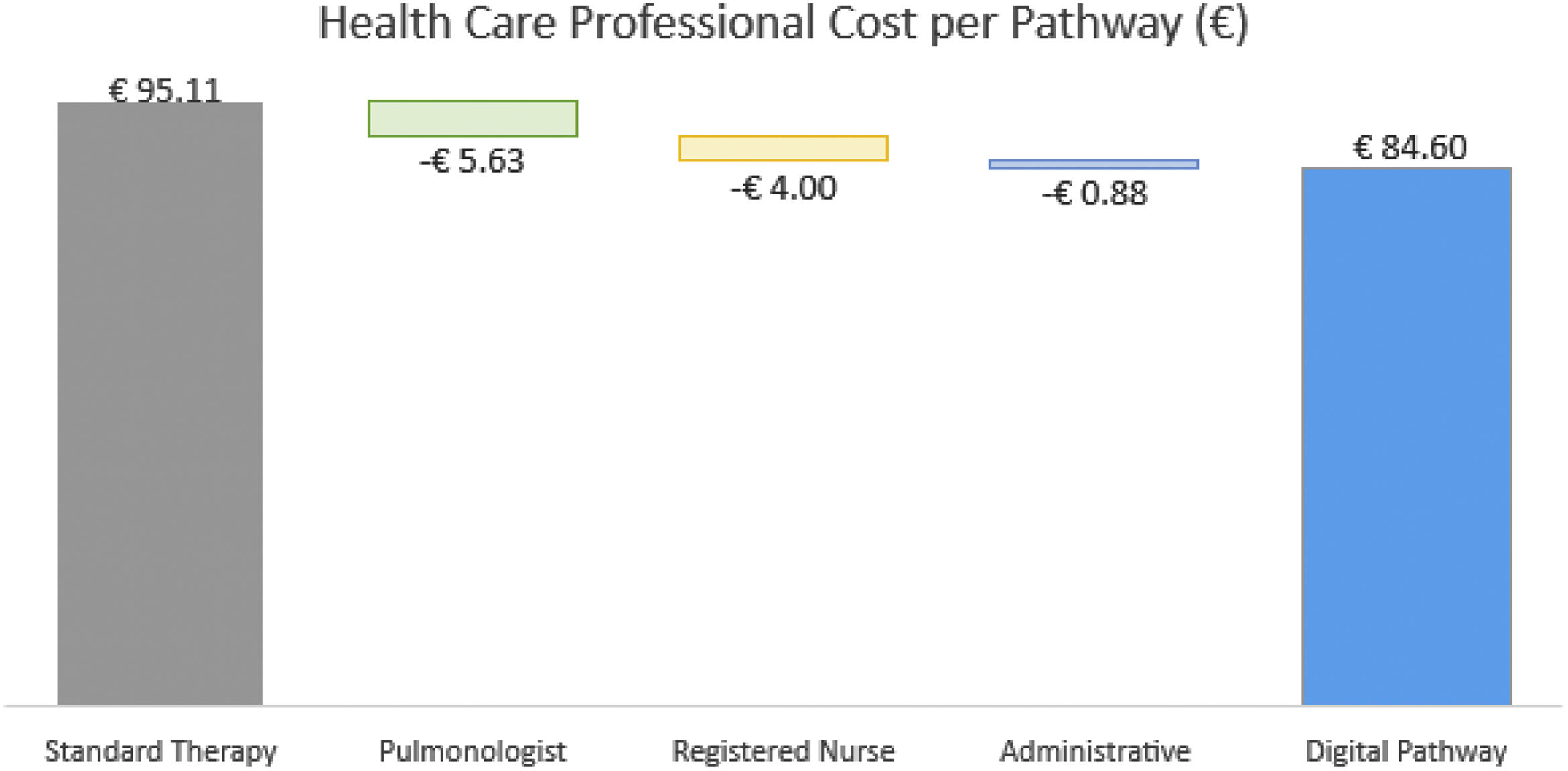
Costs per patient for administrative, nurse and pulmonologist time were all lower in the digital versus standard pathway group (Fig. 2). Therefore, the total cost per patient for the digital pathway (€85) was 10.5% lower than that for the standard pathway group (€95.11).
Therapy outcomes and device usageIndividuals managed using the digital pathway approach had a mean residual AHI of 3.7h and a mean ESS score of 3.4; no data on these parameters were available for those managed using the standard pathway. The number of hospital appointment visits per patient in the digital pathway group was half that in the standard pathway group (3.1 vs. 6.0, respectively).
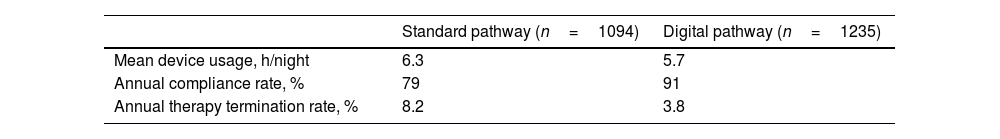
Mean CPAP device usage improved by more than half an hour per night in individuals managed using the digital versus standard pathway (Table 2). In addition, the annual adherence rate was higher and the therapy termination rate was lower in those managed using the digital pathway compared with the standard pathway (Table 2).
DiscussionThe results of this analysis showed that the implementation of a digital pathway for management of CPAP therapy in people with OSA dramatically reduced waiting lists, decreased HCP time and costs, improved device usage and compliance rates, and decreased the need for face-to-face appointments/consultations.
Revisions to the OSA patient pathway at Hospital Marqués de Valdecilla, Santander, Spain were driven by the COVID-19 pandemic. The pandemic and associated restrictions on in-person health consultations resulted in the temporary closure of sleep units, limiting access to diagnostic evaluation and treatment initiation. Already having a good foundation of telemonitoring utilisation during routine clinical care allowed the hospital to transform the patient management pathway to a digital approach.
Although absolute cost savings per patient after switching to the digital pathway were relatively modest, these would add up quickly given the substantial number of individuals with OSA (about 26–28% of the adult population in Spain). In addition, the huge reduction in waiting list time seen after the implementation of a digital pathway would be expected to have a clinically relevant impact on access to sleep services and the efficiency of patient care. Untreated OSA is costly,15–17 and early and effective treatment with CPAP can help to at least partly ameliorate some of the negative impacts of OSA.26–28 Therefore, using a digital pathway to facilitate earlier access to treatment could potentially contribute to a reduction in the negative effects of OSA on development and progression of comorbid conditions.
Device usage after the transition from a standard pathway to a digital pathway for the management of individual with OSA increased from 5.7 to 6.3h/night. This level of device usage is higher than that reported in a previous Spanish study (median 5h/night),22 which may reflect greater use of telemonitoring in the current population compared with the earlier study, although other unknown factors may also have had an effect. The increase in device usage of 0.6h/night with a digital versus standard pathway for CPAP therapy management is greater than the clinically relevant difference of 0.5h/night,29 and consistent with data from a meta-analysis showing that telemedicine-based strategies in general are associated with improved adherence to positive airway pressure therapy in people with OSA.30 Furthermore, a clear dose-response relationship has been reported between hours of positive airway pressure usage for OSA treatment and healthcare utilisation.31 Therefore, any increase in CPAP usage is likely to have incremental benefits. It has previously been reported that each additional hour per night of device usage was associated with a 5%–10% reduction in the number of emergency room visits and hospitalisations.31 In the current study, the number of planned hospital appointments per patient in the digital pathway group was half that in the standard pathway group. This means that the digital approach could reduce the patient burden of travel time to appointments (resulting in a gain in work and/or leisure time). Recent data from Spain found that the use of telemonitoring for CPAP therapy follow-up allowed patients to avoid hospital visits, which saved travel costs and reduced work absenteeism.32
The annual compliance rate for people with OSA treated at this expert centre using the standard pathway was quite good (79%). This is consistent with the compliance rates reported in a recent Spanish study (75%–80%),23 and higher than the 64.4% of participants who had good CPAP compliance in an earlier study from Spain.22 However, the annual compliance rate in the current analysis was even higher in those managed using the digital pathway (91%).
Therapy termination is the most extreme form of non-adherence to positive airway pressure. Termination of CPAP therapy has been shown to be associated with a significantly higher risk of all-cause death compared with continued CPAP usage,33 highlighting the value of strategies designed to improve ongoing usage of CPAP in people with OSA. The therapy termination rate in the digital pathway group in this study was less than half that in the standard pathway group (3.8% vs. 8.2%). A study from Germany in new users of positive airway pressure reported 1-year therapy termination rates of 5.4% in the telemonitoring group and 11.0% in the standard care group,34 both of which are slightly higher than the corresponding groups in the current study. However, the magnitude of benefit with a digital strategy was similar.
The key strength of this study is that it evaluates the impact of two different patient care pathways on objective CPAP therapy metrics in individuals with OSA. However, several limitations also need to be considered when interpreting the findings. Firstly, this was a retrospective analysis rather than a randomised controlled trial, meaning that the possibility of bias exists. In particular, because the different pathways were used sequentially there is the potential for change in factors that could have influenced study parameters other than the patient pathway model (e.g. other advances in therapy, specific patient characteristics). In addition, the analysis utilised a database that was designed for clinical (rather than research) purposes. For example, this meant that it was not possible to extract data on the ESS score and the AHI for the standard pathway period, and to allow for matched data only mean values for each period could be compared. It is also possible that pandemic-related restrictions on in-person healthcare could have contributed to the lower number of hospital visits in the digital pathway versus standard pathway groups. Finally, this analysis was conducted at a single centre in Spain and therefore the study findings may not be directly generalisable to other centres or healthcare settings. This is especially the case for different countries where processes for managing OSA may differ from those in Spain.
In conclusion, this study showed that technology-enabled process improvements have the potential to improve CPAP device usage, reduce therapy termination rates, decrease HCP time and costs, and improve outcomes in people with OSA. Additional studies are needed to determine whether a digital patient pathway would have similar effects in different healthcare settings, and to evaluate the impact of the improvements seen on hard clinical outcomes.
FundingThis study did not receive any external funding.
Authors’ contributionsConception and design: SC, PP. Analysis: SC, MD, MG. Interpretation: MD, MG. Drafting the first version of the manuscript: SC. Review and editing of the manuscript: all authors.
Conflicts of interestSC and MD are employees of ResMed, and MD is a shareholder in ResMed. MG and PP have no conflicts of interest to disclose.
Medical writing support for preparation of the manuscript first draft was provided by Nicola Ryan, independent medical writer, funded by ResMed.