To evaluate the efficacy and safety of intracranial stenting as a rescue therapy after failed mechanical thrombectomy in patients with acute ischemic stroke.
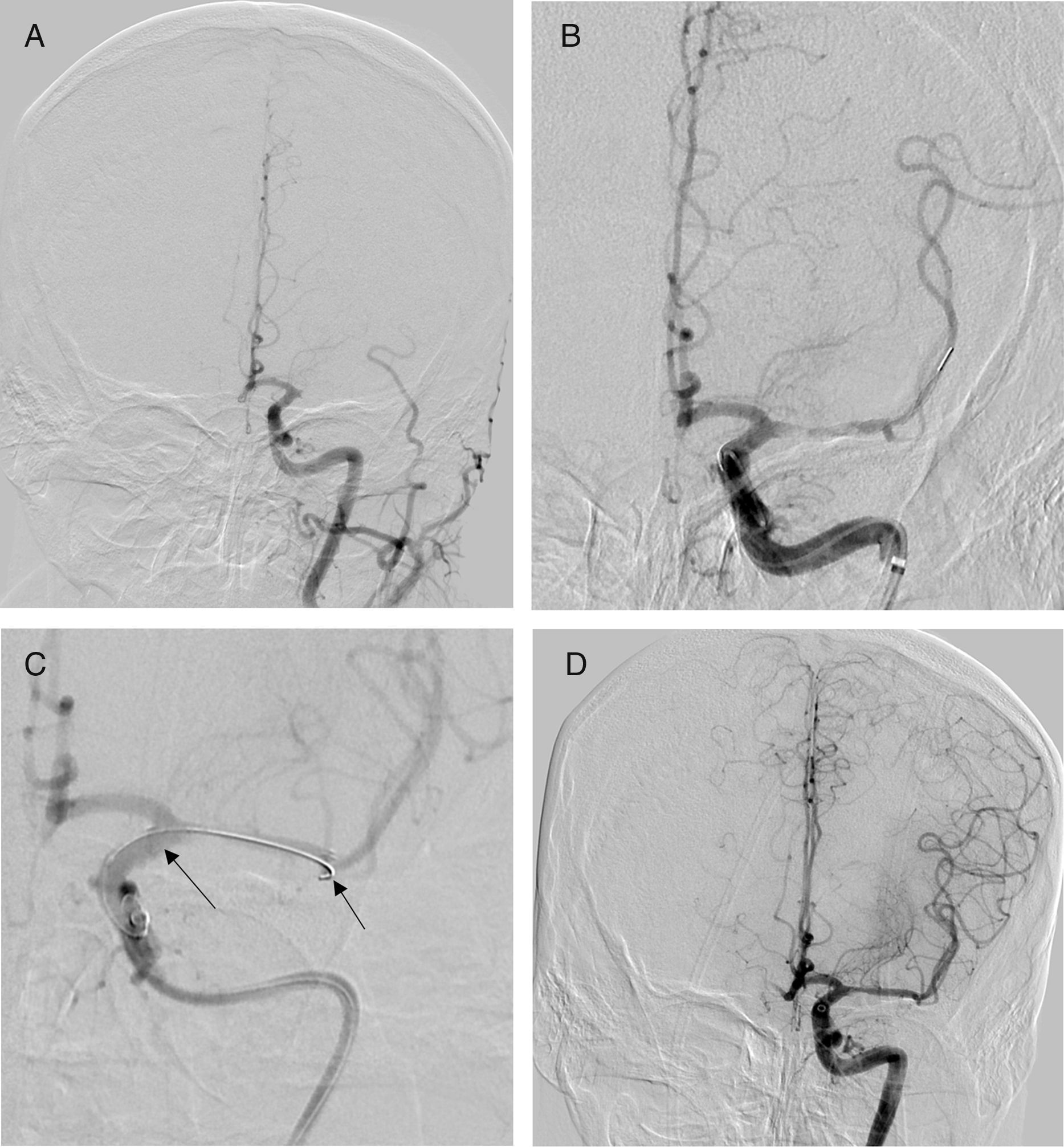
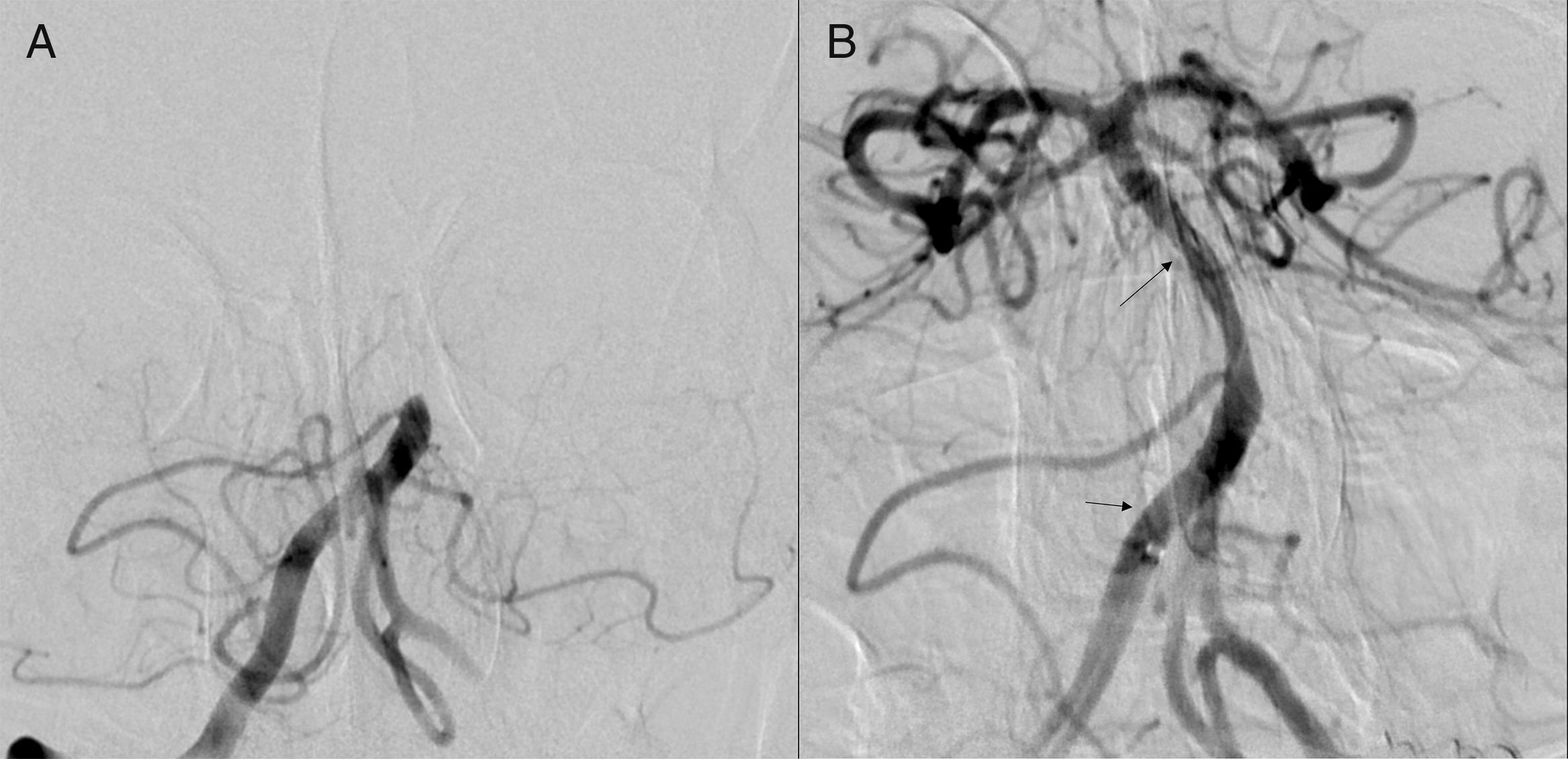
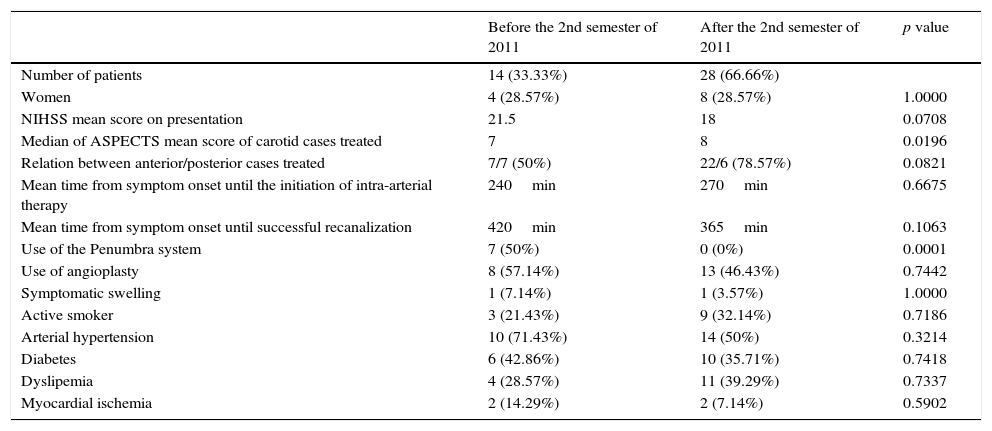
Material and methodsWe retrospectively studied 42 patients treated with intracranial stenting after failed mechanical thrombectomy between December 2008 and January 2016. We compared outcomes before and after the incorporation of stentrievers. We assessed the degree of recanalization in the carotid and basilar territories (modified TIMI score), prognostic factors, and outcome (modified Rankin scale at 3 months). Safety was evaluated in function of the appearance of symptomatic intracranial hemorrhage (SICH).
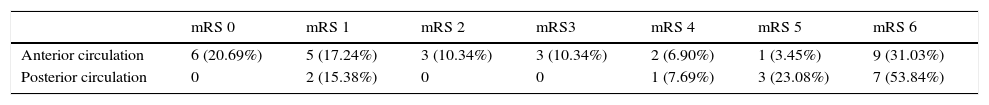
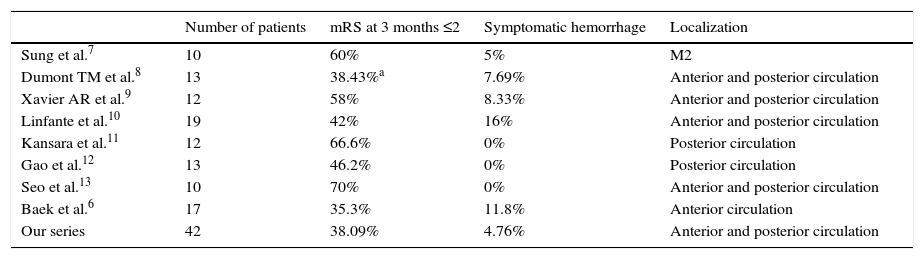
ResultsMedian NIHSS was 17 in patients with carotid territory strokes and 26 in those with vertebrobasilar territory strokes. Median time from onset of symptoms to treatment was 225min in carotid territory strokes and 390min in vertebrobasilar territory strokes. A total of 10 patients underwent intravenous fibrinolytic therapy before treatment with stentrievers. Two patients developed SICH; both had undergone intravenous fibrinolytic therapy (p=0.0523). Recanalization was effective in 30 (71.4%) in the entire series: in 7 (50%) of 14 patients treated before the incorporation of stentrievers and in 23 (82.1%) of 28 treated after the incorporation of stentrievers (p=0.0666). Outcome at 3 months was good in 2 (14.3%) patients in the earlier group and in 14 (50%) patients in the later group (p=0.042). We found significant associations between recanalization and outcome (p=0.0415) and between shorter time to treatment and outcome (p=0.002). Outcome was good in 14 (48.3%) of the 29 patients with carotid territory strokes and in 2 (15.4%) of the 13 patients with vertebrobasilar territory strokes (p=0.078).
ConclusionsIntracranial stenting is the rescue treatment when the usual treatment fails. Stentrievers must be used to eliminate the clot burden before stenting. In our study, antiplatelet treatment did not seem to increase the risk of SICH except in patients with prior intravenous fibrinolytic therapy.
Valorar la eficacia y seguridad del stent intracraneal (SI) como rescate tras el fallo de la trombectomía mecánica en el ictus isquémico agudo.
Material y métodosRevisión retrospectiva de 42 pacientes (diciembre de 2008-enero de 2016) con SI como rescate. Comparamos la evolución antes y tras incorporar los stentrievers. Valoramos el grado de recanalización en territorio carotídeo y basilar (escala TICIm), factores pronósticos y evolución (escala mRS a los 3 meses). El grado de seguridad se valoró por la aparición de hemorragia sintomática intracraneal (HSI).
ResultadosLa mediana del NIHSS en territorio carotídeo fue 17 y en posterior 26. La mediana del tiempo desde la clínica hasta el tratamiento en territorio carotídeo fue de 225 minutos, y en vertebrobasilar, de 390 minutos. Un total de 10 pacientes fueron tratados con fibrinólisis intravenosa (FIV) antes de usar stentrievers. Hubo dos casos con HSI, ambos con FIV previa (p=0,0523). La recanalización fue efectiva en 30 (71,42%), 7 de 14 antes de los stentrievers y 23 de 28 (82,14%) tras ello (p=0,0666). Dos pacientes mostraron buena evolución a 3 meses en el primer grupo y 14 en el segundo (p=0,042). La asociación fue estadísticamente significativa entre recanalización y evolución (p=0,0415) y entre menor tiempo del tratamiento y evolución (p=0,002). Un total de 14 de 29 pacientes en territorio carotídeo y 2 de 13 en posterior tuvieron buena evolución (p=0,078).
ConclusionesEl SI es un método de rescate si el tratamiento habitual falla. Antes hay que usar stentriever para eliminar la carga de trombos. En nuestro estudio, la antiagregación no parece incrementar el riesgo hemorrágico excepto en pacientes con FIV previa.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora